Top videos

Breast Cancer spreads by 3 mechanisms- local spread, by lymph nodes, or through the blood. Dr. Lorraine Champion, and Dr. Lisa Bailey discuss how breast cancer spreads. They discuss the different methods of spread and how this will affect the treatment of breast cancer.
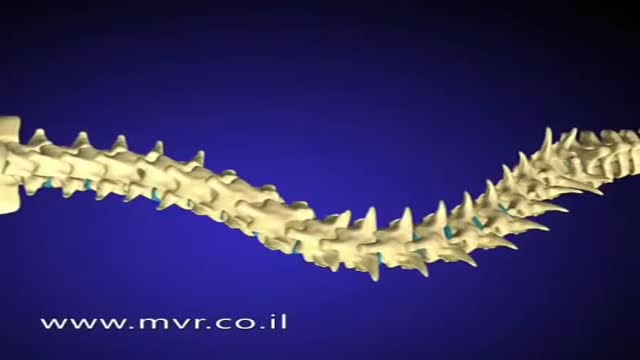
There are several approaches to scoliosis surgery, but all use modern instrumentation systems in which hooks and screws are applied to the spine to anchor long rods. The rods are then used to reduce and hold the spine while bone that is added fuses together with existing bone.

Initial treatment of a deviated septum may be directed at managing the symptoms of the tissues lining the nose, which may then contribute to symptoms of nasal obstruction and drainage. Your doctor may prescribe: Decongestants. Decongestants are medications that reduce nasal tissue swelling, helping to keep the airways on both sides of your nose open. Decongestants are available as a pill or as a nasal spray. Use nasal sprays with caution, however. Frequent and continued use can create dependency and cause symptoms to be worse (rebound) after you stop using them. Decongestants have a stimulant effect and may cause you to be jittery as well as elevate your blood pressure and heart rate. Antihistamines. Antihistamines are medications that help prevent allergy symptoms, including obstruction and runny nose. They can also sometimes help nonallergic conditions such as those occurring with a cold. Some antihistamines cause drowsiness and can affect your ability to perform tasks that require physical coordination, such as driving. Nasal steroid sprays. Prescription nasal corticosteroid sprays can reduce inflammation in your nasal passage and help with obstruction or drainage. It usually takes from one to three weeks for steroid sprays to reach their maximal effect, so it is important to follow your doctor's directions in using them. Medications only treat the swollen mucus membranes and won't correct a deviated septum.

Rotator cuff pain commonly causes local swelling and tenderness in the front of the shoulder. You may have pain and stiffness when you lift your arm. There may also be pain when the arm is lowered from an elevated position. Beginning symptoms may be mild. Patients frequently do not seek treatment at an early stage. These symptoms may include: Minor pain that is present both with activity and at rest Pain radiating from the front of the shoulder to the side of the arm Sudden pain with lifting and reaching movements Athletes in overhead sports may have pain when throwing or serving a tennis ball As the problem progresses, the symptoms increase: Pain at night Loss of strength and motion Difficulty doing activities that place the arm behind the back, such as buttoning or zippering If the pain comes on suddenly, the shoulder may be severely tender. All movement may be limited and painful.

The menstrual cycle is the regular natural change that occurs in the female reproductive system that makes pregnancy possible. The cycle is required for the production of oocytes, and for the preparation of the uterus for pregnancy.
The dural venous sinuses are spaces between the endosteal and meningeal layers of the dura. They contain venous blood that originates for the most part from the brain or cranial cavity. The sinuses contain an endothelial lining that is continuous into the veins that are connected to them.
The anus is close to the vagina and sometimes it’s hard to say what’s going on inside the body. Is it possible to get pregnant from anal sex? The answer is yes and this video explains the circumstances. Please protect yourselves and stay curious.

-Failure to thrive (FTT) is not a diagnosis in itself; rather, it is a term used to describe failure to gain weight in children younger than two years old. Children categorized as FTT weigh less than the 5th percentile for their age; more severe cases involve a slowing of linear growth and head circumference as well. The three causes of FTT are inadequate calorie intake, inadequate calorie absorption, and increased calorie requirements. Newborn infants need 110 kcal/kg/day, while children up to twelve months need 100