Top videos

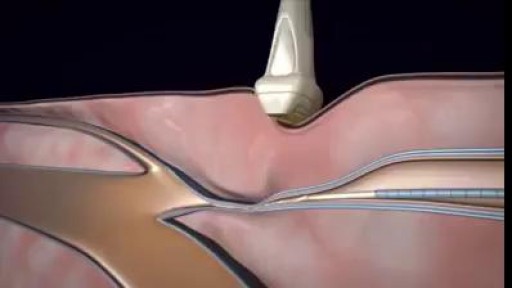
This 25 year young female wanted her split earlobe hole to be repaired.Ear lobe ring hole usually elongated due to continuous use of fancy heavy ear rings.most young ladies suffer from this problem, subsequently this get converted to complete split ear lobe.This needs surgical repair only.This is a cosmetic repair .watch the video , how this repair is done.Usually the split is completely closed with suture.After healing new hole to be done little distance from the repair site.
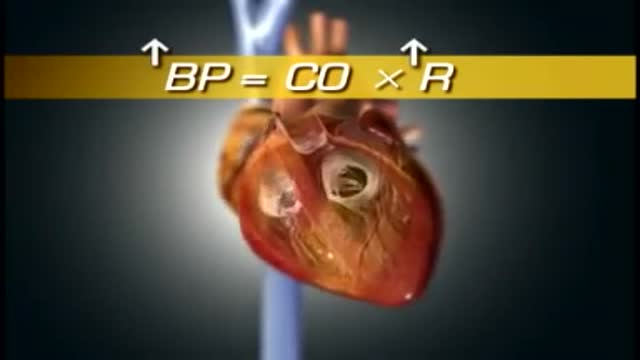
High blood pressure is a common condition in which the long-term force of the blood against your artery walls is high enough that it may eventually cause health problems, such as heart disease. Blood pressure is determined both by the amount of blood your heart pumps and the amount of resistance to blood flow in your arteries. The more blood your heart pumps and the narrower your arteries, the higher your blood pressure. You can have high blood pressure (hypertension) for years without any symptoms. Even without symptoms, damage to blood vessels and your heart continues and can be detected. Uncontrolled high blood pressure increases your risk of serious health problems, including heart attack and stroke. High blood pressure generally develops over many years, and it affects nearly everyone eventually. Fortunately, high blood pressure can be easily detected. And once you know you have high blood pressure, you can work with your doctor to control it.
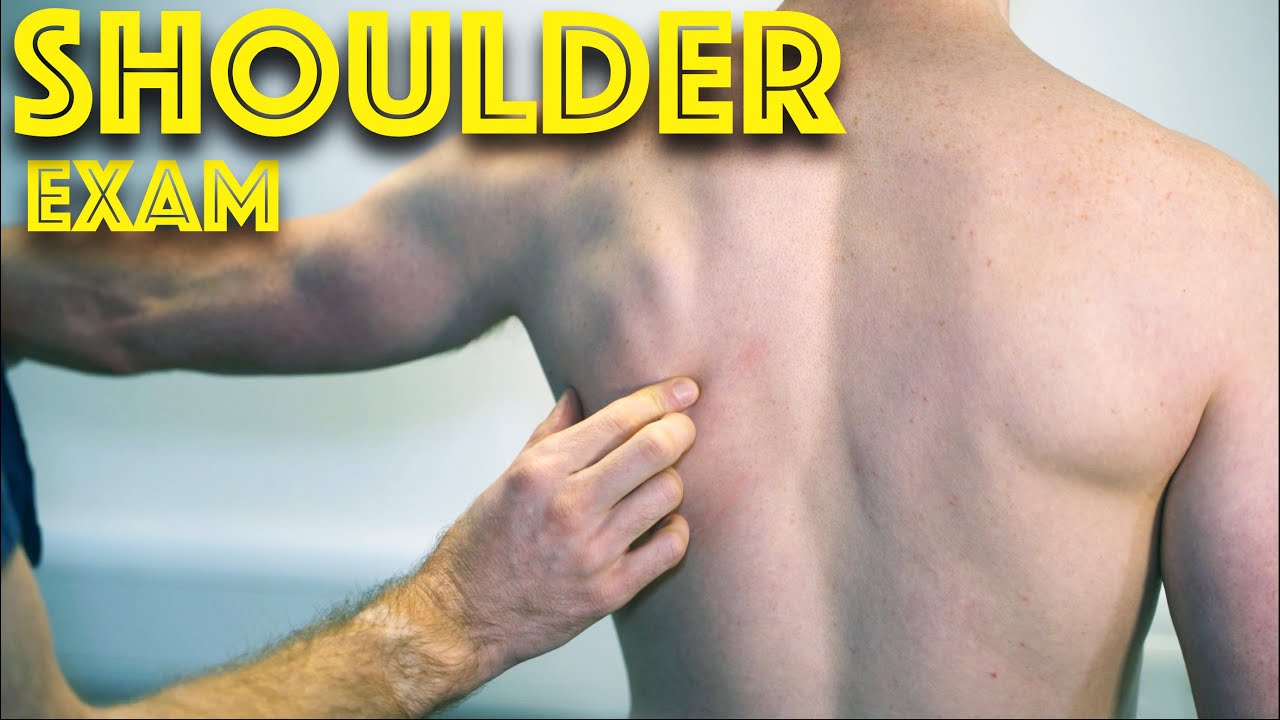
Shoulder Clinical Examination - Medical School Clinical Skills - Dr Gill
Personally, I find the shoulder examination the most complex examination possibly as there are so many variations and special tests. Some of which overlap and some will relate specifically to a patients presentation.
Often in a medical school syllabus, only select special tests will be used. In this shoulder exam demonstration, we include the Hawkins-Kennedy Test looking for impingement. This is dovetailed with examination for bicipital tendonitis as this is another possible cause of impingement type symptoms.
This shoulder upper limb exam follows the standard "Look, Feel, Move" orthopaedic exam approach, and overall order as set out in MacLeods Clinical Examination
Watch further orthopaedic examinations for your OSCE revision:
The Spine Examination:
https://youtu.be/pJxMHa6SCgU
Knee Examination
https://youtu.be/oyKH4EYfJDM
Hip Joint Clinical Examination
https://youtu.be/JC9GKq5nSdQ
________
Please note that there is no ABSOLUTE way to perform a clinical examination. Different institutions and even clinicians will have differing degrees of variations - the aim is the effectively identify medically relevant signs.
However during OSCE assessments. Different medical schools, nursing colleges, and other health professional courses will have their own preferred approach to a clinical assessment - you should concentrate on THEIR marks schemes for your assessments.
The examination demonstrated here is derived from Macleods Clinical Examination - a recognized standard textbook for clinical skills.
#ShoulderExamination #ClinicalSkills #DrGill
Symptoms of liver failure include vomiting, diarrhea and fatigue as well as the symptoms from stage 3. While the progression from cirrhosis to failure can take years, the damage is irreversible and leads to eventual death. The key to treating liver disease is to diagnose the condition as early as possible.
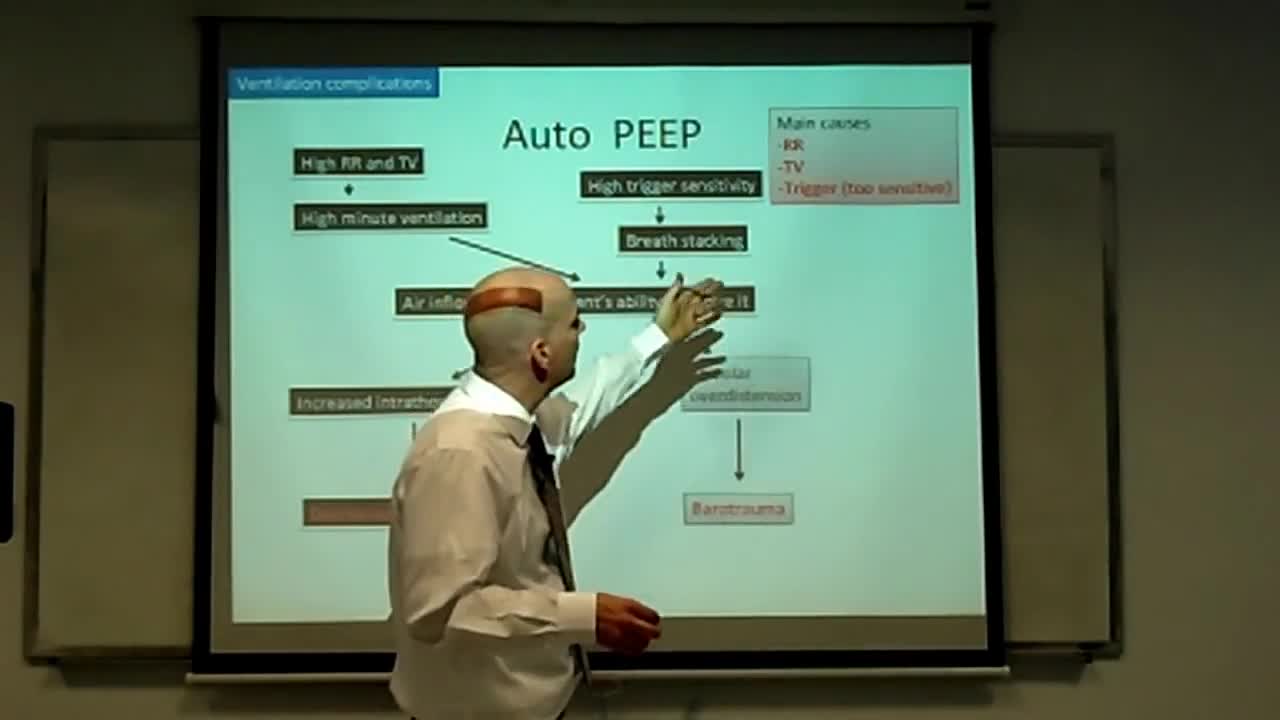
This is an introduction to ventilator settings like FIO2, PEEP, Flow rate,trigger,TV, and RR. I also discuss how these settings relate to CO2 and O2 control and to complications like oxygen toxicity and barotrauma with an emphasis on physiology.

Butt implants are a popular plastic surgery procedure among those who wish to enhance the appearance, shape, and size of their rear ends. Buttock augmentation involves the surgical insertion of artificial body implants into a patient’s buttocks to create a larger, shapelier, and more sensuous rear end. Patients who have underdeveloped buttocks can achieve a more proportionate figure with butt implants. Women who wish to achieve an “hour glass” figure or are unhappy with the size of their buttocks can benefit from female butt implants. Men with flat or poorly developed buttocks can enhance the shape of the area to their liking with male butt implants. Many buttock augmentation patients say that their clothes fit better, they feel more attractive, and their confidence levels have improved.
There are four major blood groups determined by the presence or absence of two antigens – A and B – on the surface of red blood cells: Group A – has only the A antigen on red cells (and B antibody in the plasma) Group B – has only the B antigen on red cells (and A antibody in the plasma) Group AB – has both A and B antigens on red cells (but neither A nor B antibody in the plasma) Group O – has neither A nor B antigens on red cells (but both A and B antibody are in the plasma)

Dr. Eric Janssen of SportsMED Orthopaedic Surgery & Spine Center in Huntsville, Alabama demonstrates a total knee replacement using dry bones model. In this demonstration he uses the Wright Medical Evolution Knee implant. This demonstrations does not include soft tissue.

Dr. James Wall performs a bilateral inguinial hernia repair surgical procedure.
Featured:
James Wall, MD
Assistant Professor of Surgery, Pediatric Surgery
Assistant Professor of Bioengineering (By Courtesy)
Lucile Salter Packard Children's Hospital
Micaela Esquivel, MD
Chief Resident of General Surgery