Top videos

Multiple sclerosis causes many different symptoms, including vision loss, pain, fatigue, and impaired coordination. The symptoms, severity, and duration can vary from person to person. Some people may be symptom free most of their lives, while others can have severe chronic symptoms that never go away. Physical therapy and medications that suppress the immune system can help with symptoms and slow disease progression.

A VCUG (Voiding Cystourethrogram) is a test that looks at how well your child's kidneys, ureters and bladder are working. Your child's kidneys make urine. The urine flows from the kidneys through thin tubes (called ureters) into your child's bladder.
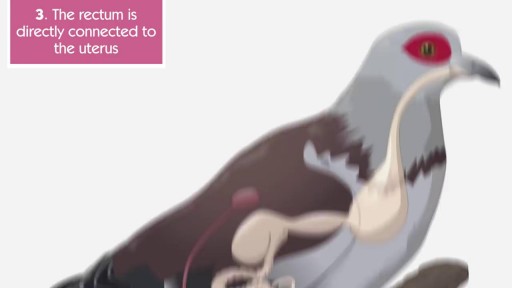
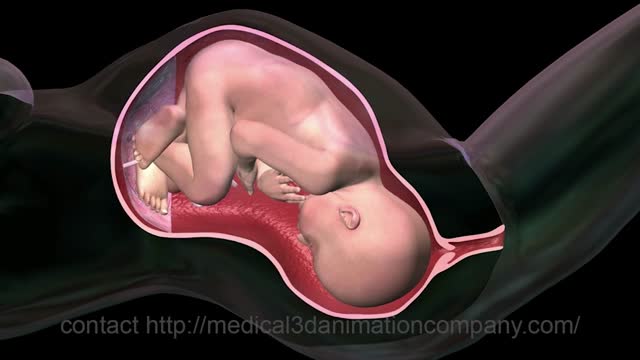
The anus is close to the vagina and sometimes it’s hard to say what’s going on inside the body. Is it possible to get pregnant from anal sex? The answer is yes and this video explains the circumstances. Please protect yourselves and stay curious.

The fuel for the process leading to orgasm is testosterone, a hormone produced in steady supply by the testicles. The testicles also make millions of sperm each day, which mature and then are mixed with whitish, protein-rich fluids. These fluids nourish and support the sperm so they can live after ejaculation for a limited time. This mixture of fluid and sperm, known as semen, is what is moved through the urethra and out the penis during orgasm.
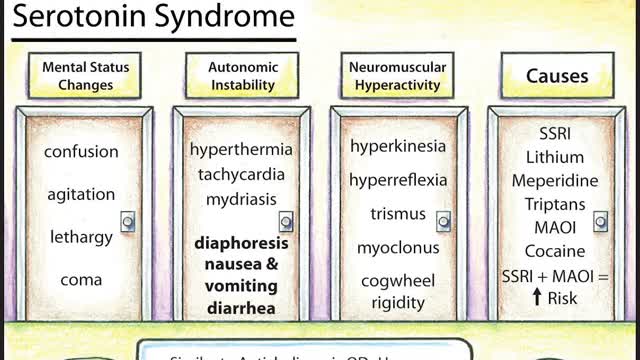
Symptoms of serotonin syndrome include a classic triad of mental status changes (eg, anxiety, delirium, confusion, restlessness), autonomic dysregulation (eg, diaphoresis, tachycardia, hypertension, hyperthermia, diarrhea, mydriasis), and neuromuscular hyperactivity (eg, hyperreflexia, tremor, rigidity, myoclonus, ocular clonus). Serotonin syndrome is clinically diagnosed and laboratory tests are used to rule out other etiologies. It usually occurs due to inadvertent interactions between drugs, therapeutic use of multiple serotonergic agents, or serotonergic medication overdose. Treatment involves discontinuation of serotonergic drugs, supportive measures, and sedation with benzodiazepines. In severe cases, a serotonin antagonist (cyproheptadine) may be used.
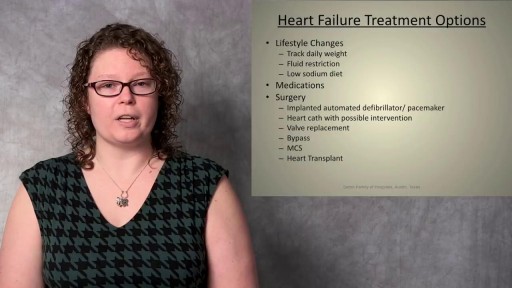
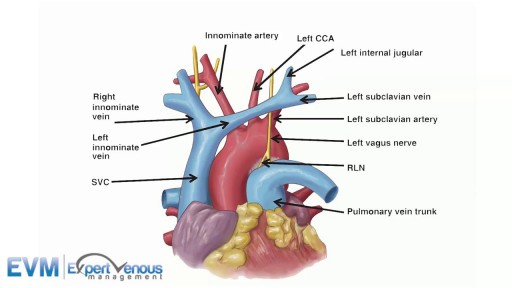
Although individual surgeons and centers employ different methods to insert a left ventricular assist device (LVAD), the fundamental concepts remain true for all. That is, most devices use the apex of the left ventricle (LV) as the inflow site to the pump, which subsequently gives off an outflow graft to the aorta, thus bypassing the ailing LV. Currently available devices do not differ significantly with regard to general implantation technique. The sequence of implantation can vary also from patient to patient, depending on the particular situation. In some cases, concomitant procedures may be performed in conjunction with LVAD implantation without adversely affecting outcome.

Traditionally, the appendix is removed through an incision in the right lower abdominal wall. In most laparoscopic appendectomies, surgeons operate through 3 small incisions (each ¼ to ½ inch) while watching an enlarged image of the patient's internal organs on a television monitor.
Pharyngitis is caused by swelling in the back of the throat (pharynx) between the tonsils and the voice box (larynx). Most sore throats are caused by colds, the flu, coxsackie virus or mono (mononucleosis). Bacteria that can cause pharyngitis in some cases: Strep throat is caused by group A streptococcus.