Top videos

The journey of egg and sperm. There are a lot of casualties (deaths) among the sperm as they swim toward the egg. First, many get lost in the maze of a woman's uterus where they also have to contend with acidic vaginal secretions.
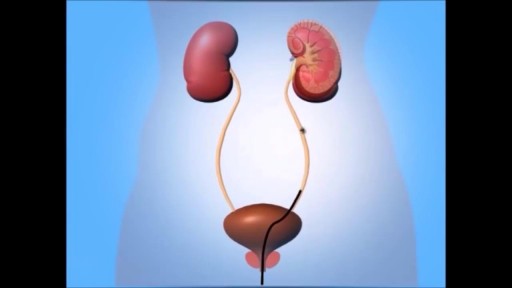
A ureteroscopy is an examination or procedure using a ureteroscope. A ureteroscope, like a cystoscope, is an instrument for examining the inside of the urinary tract. The urologist can insert small instruments through the cystoscope to treat problems in the urethra and bladder or perform a biopsy. For a ureteroscopy, the urologist passes the ureteroscope through the bladder and into a ureter.

Throughout your life, your skin will change constantly, for better or worse. In fact, your skin will regenerate itself approximately every 27 days. Proper skin care is essential to maintaining the health and vitality of this protective organ.
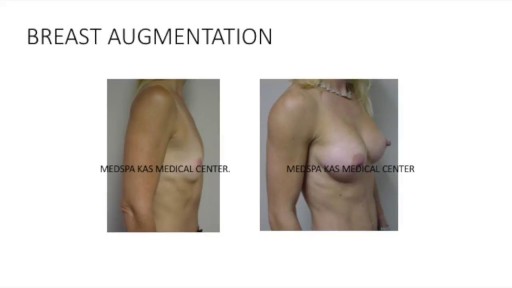
This is a complete video of breast augmentation procedure with implants also includes some before after photographs of breast augmentation surgery by Dr. Ajaya Kashyap at MedSpa Clinic, Delhi, India. source: https://www.youtube.com/watch?v=tRg3RkvCvOE Get more information: www.bestbreastsurgeryindia.com Get more information: www.themedspa.us Email at: info@themedspa.us Call/WhatsApp on:+91-9818369662, 9958221983/82/81

Several options are available to remove spider veins — thin red lines or weblike networks of blood vessels that appear on your legs and feet. Spider veins are usually harmless, though they can sometimes cause aching, burning or pain, especially when you've been standing for long periods. If you have symptoms or are concerned about the appearance of spider veins, treatment options include: Sclerotherapy. In this procedure, your doctor injects the veins with a solution that scars and closes those veins, causing the blood to reroute through healthier veins. In a few weeks, treated spider veins fade. Although the same vein may need to be injected more than once, sclerotherapy is usually effective if done correctly. Sclerotherapy doesn't require anesthesia and can be done in your doctor's office. Side effects include swelling, itching and skin color changes in the treated area. Laser surgery. Laser surgery works by sending strong bursts of light into the vein that make the vein slowly fade and disappear. No incisions or needles are used. The treatment is often less effective than sclerotherapy, particularly for larger veins. Side effects may include redness, bruising, itching, swelling and permanent skin tone changes. After treatment, blood vessels fade over several months, but they may not disappear completely. Also, new spider veins can develop in the same area.

4000 Grafts Hair Transplant Surgery Result after 7months by Dr. Ariganesh Chandrasegaran (MD, PGI Chandigarh) at DermaClinix. DermaClinix is known for the best hair transplant in Chennai as well as across India. Dramatic transformation by our flagship patented procedure B.E.S.T. (Bio-Enhanced Simultaneous Transplant Technique) FUE which helps in achieving almost complete survival with early and natural looking results. Book Your Free Consultation: +91 8939636222, 04428282606. More at https://www.hairtransplantchennai.org
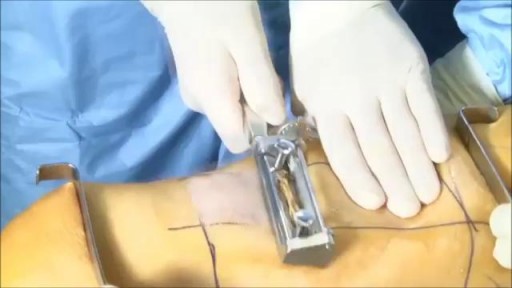
kin grafting is a type of graft surgery involving the transplantation of skin. The transplanted tissue is called a skin graft. Skin grafting is often used to treat: Extensive wounding or trauma Burns Areas of extensive skin loss due to infection such as necrotizing fasciitis or purpura fulminans[2] Specific surgeries that may require skin grafts for healing to occur - most commonly removal of skin cancers Skin grafts are often employed after serious injuries when some of the body's skin is damaged. Surgical removal (excision or debridement) of the damaged skin is followed by skin grafting. The grafting serves two purposes: reduce the course of treatment needed (and time in the hospital), and improve the function and appearance of the area of the body which receives the skin graft.
Home Remedies For Acid Reflux, Ginger For Acid Reflux, Heartburn After Gallbladder Removal --- http://heartburn-acid-reflux.info-pro.co --- Stop using Pepto Bismol until you read the following… There is BREAKING scientific news reporting that many of America’s most popular antacids – both the ones you buy at the drug store and the ones you need prescriptions for… Are linked to more than a dozen forms of potentially DEADLY cancers. Click this link now to get the full story and see if you’re at risk. You’ll find out about a “just discovered” alternative to antacids…. Something that can permanently cure even the worst cases of acid reflux in as little few days, and that doesn’t require any pills or medications. Click Here: http://heartburn-acid-reflux.info-pro.co