Top videos

an incision made on the back of the lower leg starting just above the heel bone. After the surgeon finds the two ends of the ruptured tendon, these ends are sewn together with sutures. The incision is then closed. Another repair method makes a small incision on the back of the lower leg at the site of the rupture.

The timing of the nausea or vomiting can indicate the cause. When appearing shortly after a meal, nausea or vomiting may be caused by food poisoning, gastritis (inflammation of the stomach lining), an ulcer, or bulimia. Nausea or vomiting one to eight hours after a meal may also indicate food poisoning.

The examination consists of three portions: Inspection, Palpation, and Synthesis of data from these techniques In addition to palpating for size, also note the gland texture, mobility, tenderness and the presence of nodules. Inspection Inspection: Anterior Approach The patient should be seated or standing in a comfortable position with the neck in a neutral or slightly extended position. Cross-lighting increases shadows, improving the detection of masses. To enhance visualization of the thyroid, you can: Extending the neck, which stretches overlying tissues Have the patient swallow a sip of water, watching for the upward movement of the thyroid gland. quicktime video 251KB video demo from Return to the Bedside Inspection: Lateral Approach After completing anterior inspection of the thyroid, observe the neck from the side. Estimate the smooth, straight contour from the cricoid cartilage to the suprasternal notch. Measure any prominence beyond this imagined contour, using a ruler placed in the area of prominence. Palpation Note: There is no data comparing palpation using the anterior approach to the posterior approach so examiners should use the approach that they find most comfortable. Palpation: Anterior Approach placement of hands for palpatation of thyroid in anterior approach The patient is examined in the seated or standing position. Attempt to locate the thyroid isthmus by palpating between the cricoid cartilage and the suprasternal notch. Use one hand to slightly retract the sternocleidomastoid muscle while using the other to palpate the thyroid. Have the patient swallow a sip of water as you palpate, feeling for the upward movement of the thyroid gland. quicktime video 454KB video demo from Return to the Bedside. Palpation: Posterior Approach placement of hands for palpatation of thyroid in posterior approach The patient is examined in the seated or standing position. Standing behind the patient, attempt to locate the thyroid isthmus by palpating between the cricoid cartilage and the suprasternal notch. Move your hands laterally to try to feel under the sternocleidomstoids for the fullness of the thyroid. Have the patient swallow a sip of water as you palpate, feeling for the upward movement of the thyroid gland.
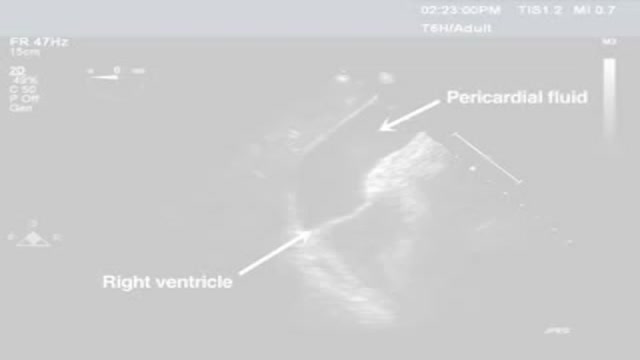
Pericardiocentesis is the aspiration of fluid from the pericardial space that surrounds the heart. This procedure can be life saving in patients with cardiac tamponade, even when it complicates acute type A aortic dissection and when cardiothoracic surgery is not available. [1] Cardiac tamponade is a time sensitive, life-threatening condition that requires prompt diagnosis and management. Historically, the diagnosis of cardiac tamponade has been based on clinical findings. Claude Beck, a cardiovascular surgeon, described 2 triads of clinical findings that he found associated with acute and chronic cardiac tamponade. The first of these triads consisted of hypotension, an increased venous pressure, and a quiet heart. It has come to be recognized as Beck's triad, a collection of findings most commonly produced by acute intrapericardial hemorrhage. Subsequent studies have shown that these classic findings are observed in only a minority of patients with cardiac tamponade. [2] The detection of pericardial fluid has been facilitated by the development and continued improvement of echocardiography. [3] Cardiac ultrasound is now accepted as the criterion standard imaging modality for the assessment of pericardial effusions and the dynamic findings consistent with cardiac tamponade. With echocardiography, the location of the effusion can be identified, the size can be estimated (small, medium, or large), and the hemodynamic effects can be examined by assessing for abnormal septal motion, right atrial or right ventricular inversion, and decreased respiratory variation of the diameter of the inferior vena cava.
Digoxin is derived from the leaves of a digitalis plant. Digoxin helps make the heart beat stronger and with a more regular rhythm. Digoxin is also used to treat atrial fibrillation, a heart rhythm disorder of the atria (the upper chambers of the heart that allow blood to flow into the heart).

A cataract is a clouding of the lens in the eye that affects vision. Most cataracts are related to aging. Cataracts are very common in older people. By age 80, more than half of all Americans either have a cataract or have had cataract surgery. A cataract can occur in either or both eyes. It cannot spread from one eye to the other.

An ICD is a battery-powered device placed under the skin that keeps track of your heart rate. Thin wires connect the ICD to your heart. If an abnormal heart rhythm is detected the device will deliver an electric shock to restore a normal heartbeat if your heart is beating chaotically and much too fast.
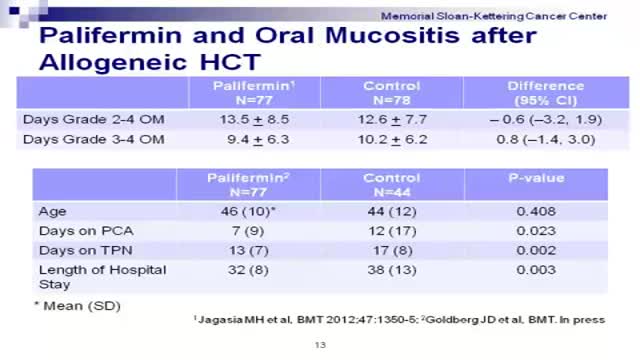
Graft-versus-host disease (GVHD) is a common complication after an allogeneic transplant, a transplant in which cells from a family member, unrelated donor or cord blood unit are used. In GVHD, the immune cells from the donated marrow or cord blood (the graft) attack the body of the transplant patient (the host).
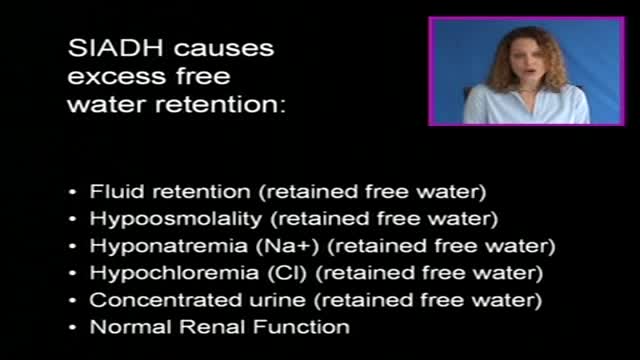
The syndrome of inappropriate antidiuretic hormone (ADH) secretion (SIADH) is defined by the hyponatremia and hypo-osmolality resulting from inappropriate, continued secretion or action of the hormone despite normal or increased plasma volume, which results in impaired water excretion.
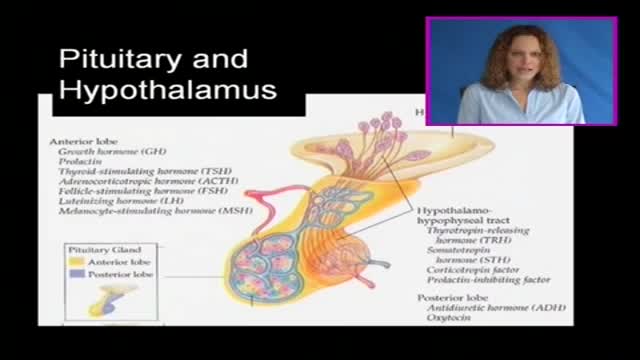
The pituitary gland is often portrayed as the "master gland" of the body. Such praise is justified in the sense that the anterior and posterior pituitary secrete a battery of hormones that collectively influence all cells and affect virtually all physiologic processes. The pituitary gland may be king, but the power behind the throne is clearly the hypothalamus. As alluded to in the last section, some of the neurons within the hypothalamus - neurosecretory neurons - secrete hormones that strictly control secretion of hormones from the anterior pituitary. The hypothalamic hormones are referred to as releasing hormones and inhibiting hormones, reflecting their influence on anterior pituitary hormones.
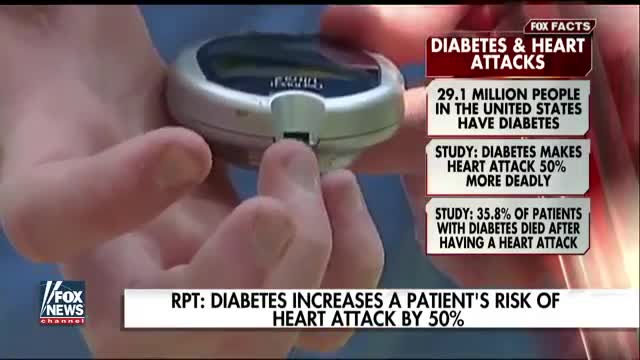
A silent heart attack is a heart attack that has few, if any, symptoms. You may have never had any symptoms to warn you that you've developed a heart problem, such as chest pain or shortness of breath. Having diabetes or prediabetes puts you at increased risk for heart disease and stroke. You can lower your risk by keeping your blood glucose (also called blood sugar), blood pressure, and blood cholesterol close to the recommended target numbersthe levels suggested by diabetes experts for good health. (
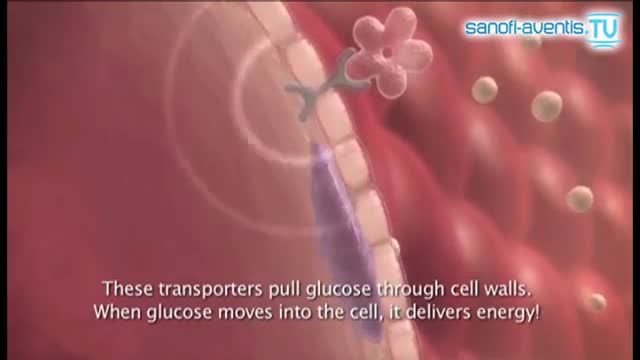
Insulin is a hormone made naturally in the pancreas that helps move sugar into the cells of your body. Your cells use the sugar as fuel to make energy. Without enough insulin, sugar stays in your bloodstream, raising your blood sugar. High blood sugar, or hyperglycemia, can lead to the signs and symptoms of diabetes:
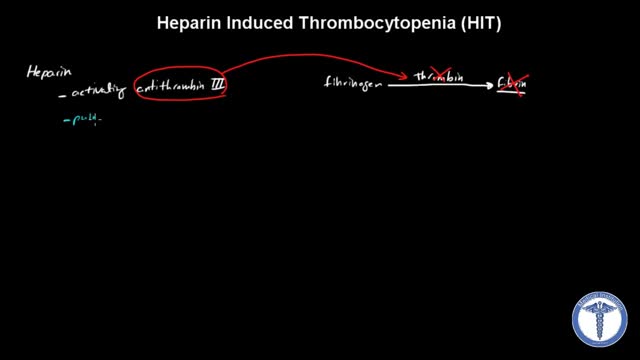
All forms of heparin (including low-molecular-weight heparin such as enoxaparin) must be stopped immediately in patients with suspected heparin-induced thrombocytopenia (HIT) while awaiting diagnostic confirmation. Patients with HIT remain at high risk of thrombosis even after discontinuation of heparin. Therefore, an alternate, rapidly acting, non-heparin anticoagulant such as direct thrombin inhibitor (eg, argatroban, bivalirudin) must be started immediately.