Top videos
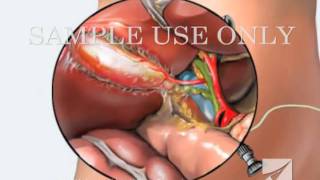
This medical animation shows laparoscopically assisted gallbladder removal surgery, or cholecystectomy. The animation begins by showing the normal anatomy of the liver and gallbladder. Over time, gallstones form within the gallbladder, blocking the cystic duct, and causing the gallbladder to become enlarged and inflamed. The procedure, sometimes called a "lap-chole", begins with the insertion of four trocar devices, which allow the physician to see inside the abdomen without making a large incision. Air is added to the abdominal cavity to make it easier to see the gall bladder. Next, we see a view through the laparascope, showing two surgical instruments grasping the gallbladder while a third severs the cystic duct. After the gallbladder is removed, the camera pans around to show that the cystic artery and vein, have already been clipped to prevent bleeding.
Item #ANIM026
The venipuncture procedure is complex, requiring both knowledge and skill to perform. Each phlebotomist generally establishes a routine that is comfortable for her or him. Several essential steps are required for every successful collection procedure: Identify the patient. Assess the patient's physical disposition (i.e. diet, exercise, stress, basal state). Check the requisition form for requested tests, patient information, and any special requirements. Select a suitable site for venipuncture. Prepare the equipment, the patient and the puncture site. Perform the venipuncture. Collect the sample in the appropriate container. Recognize complications associated with the phlebotomy procedure. Assess the need for sample recollection and/or rejection. Label the collection tubes at the bedside or drawing area. Promptly send the specimens with the requisition to the laboratory.

An untreated hepatic abscess is nearly uniformly fatal as a result of complications that include sepsis, empyema, or peritonitis from rupture into the pleural or peritoneal spaces, and retroperitoneal extension. Treatment should include drainage, either percutaneous or surgical. Antibiotic therapy as a sole treatment modality is not routinely advocated, though it has been successful in a few reported cases. It may be the only alternative in patients too ill to undergo invasive procedures or in those with multiple abscesses not amenable to percutaneous or surgical drainage. In these instances, patients are likely to require many months of antimicrobial therapy with serial imaging and close monitoring for associated complications.

Handal Plastic Surgery at the Sanctuary Surgery Center is the leading cosmetic surgery center of the Southeast Florida region, providing excellent consultation, surgery, and post operative services. Headed by Doctor Arthur G. Handal, top plastic & cosmetic surgeon in Boca Raton, the professional staff of the Sanctuary Surgery Center offers the best in patient care.

Vasculitis is an inflammation of your blood vessels. It causes changes in the walls of blood vessels, including thickening, weakening, narrowing and scarring. These changes restrict blood flow, resulting in organ and tissue damage. There are many types of vasculitis, and most of them are rare. Vasculitis might affect just one organ, such as your skin, or it may involve several. The condition can be short term (acute) or long lasting (chronic). Vasculitis can affect anyone, though some types are more common among certain groups. Depending on the type you have, you may improve without treatment. Or you will need medications to control the inflammation and prevent flare-ups. Vasculitis is also known as angiitis and arteritis.
This video: Multiple myeloma is a cancer that forms in a type of white blood cell called a plasma cell. Plasma cells help you fight infections by making antibodies that recognize and attack germs. Multiple myeloma causes cancer cells to accumulate in the bone marrow, where they crowd out healthy blood cells. Rather than produce helpful antibodies, the cancer cells produce abnormal proteins that can cause kidney problems. Treatment for multiple myeloma isn't always necessary. If you're not experiencing signs and symptoms, you may not require treatment. If signs and symptoms develop, a number of treatments can help control your multiple myeloma.

-The cremasteric reflex test is considered positive if there is elevation of the testis in response to stroking the upper inner thigh. This reaction is typically absent in testicular torsion and boys under the age of 6 months. Although not completely reliable in older boys and adults, an absent cremasteric reflex is highly suggestive of torsion. Patients with epididymitis usually have a normal cremasteric reflex, with pain and swelling isolated to
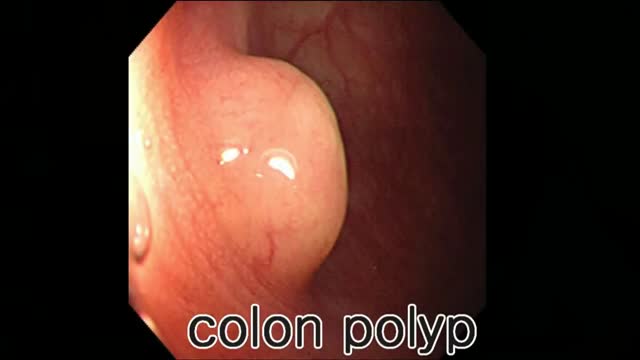
Colon polyp facts Colon polyps are growths on the inner lining of the colon and are very common. Colon polyps are important because they may be, or may become malignant (cancerous). They also are important because based on their size, number, and microscopic anatomy (histology); they can predict which patients are more likely to develop more polyps and colon cancer. Changes in the genetic material of cells lining the colon are the cause of polyps. There are different types of colon polyps with differing tendencies to become malignant and abilities to predict the development of more polyps and cancer. It is important to recognize families with members who have familial genetic conditions causing polyps because some of these conditions are associated with a very high incidence of colon cancer, and the cancer can be prevented or discovered early.
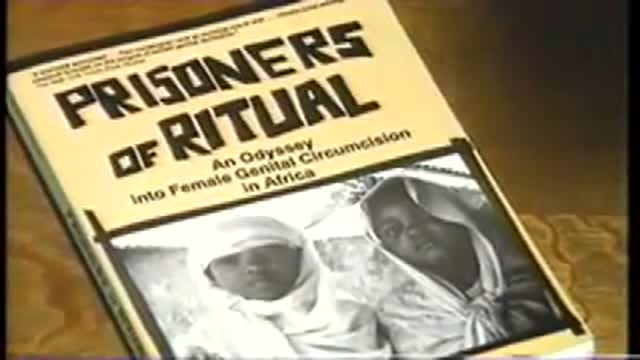
Acclaimed sexologist Hanny Lightfoot-Klein, author of several highly illuminating books on genital mutilation, discusses compromises in orgasm after male circumcision. Also commenting is cultural anthropologist James De Meo.From the groundbreaking documentary film, "Whose Body, Whose Rights?"

Function and Anatomy: The hip is a ball and socket type joint, formed by the articulation of the head of the femur with the pelvis. Normal range of motion includes: abduction 45 degrees, adduction 20-30 degrees, flexion 135 degrees, extension 30 degrees, internal and external rotation. Hip pathology can cause symptoms anywhere around the joint, though frequently pain is anterior and radiates to the groin region. Additionally, pathology outside of the hip can be referred to this region. History and exam obviously help in making these distinctions.

The pelvic floor or pelvic diaphragm is composed of muscle fibers of the levator ani, the coccygeus, and associated connective tissue which span the area underneath the pelvis. The pelvic diaphragm is a muscular partition formed by the levatores ani and coccygei, with which may be included the parietal pelvic fascia on their upper and lower aspects. The pelvic floor separates the pelvic cavity above from the perineal region (including perineum) below.
The right and left levator ani lie almost horizontally in the floor of the pelvis, separated by a narrow gap that transmits the urethra, vagina, and anal canal. The levator ani is usually considered in three parts: pubococcygeus, puborectalis, and iliococcygeus. The pubococcygeus, the main part of the levator, runs backward from the body of the pubis toward the coccyx and may be damaged during parturition. Some fibers are inserted into the prostate, urethra, and vagina. The right and left puborectalis unite behind the anorectal junction to form a muscular sling . Some regard them as a part of the sphincter ani externus. The iliococcygeus, the most posterior part of the levator ani, is often poorly developed.
The coccygeus, situated behind the levator ani and frequently tendinous as much as muscular, extends from the ischial spine to the lateral margin of the sacrum and coccyx.
The pelvic cavity of the true pelvis has the pelvic floor as its inferior border (and the pelvic brim as its superior border.) The perineum has the pelvic floor as its superior border.
Some sources do not consider “pelvic floor” and “pelvic diaphragm” to be identical, with the “diaphragm” consisting of only the levator ani and coccygeus, while the “floor” also includes the perineal membrane and deep perineal pouch. However, other sources include the fascia as part of the diaphragm. In practice, the two terms are often used interchangeably.
Inferiorly, the pelvic floor extends into the anal triangle.