Top videos

As a pediatric surgeon at NewYork-Presbyterian/Weill Cornell Medical Center, Dr. Nitsana Spigland treats newborns, children, teens, and young adults requiring surgical interventions. She specializes in antenatal counseling and newborn congenital malformations.
Learn more about Dr. Spigland at: https://www.nyp.org/physician/nspigland.

Kendall Lee, M.D., describes deep brain stimulation surgery, and how it is is typically done with patients who remain awake, so neurological functions can be measured and maintained. For more information on deep brain stimulation, visit http://mayocl.in/2A09T80.

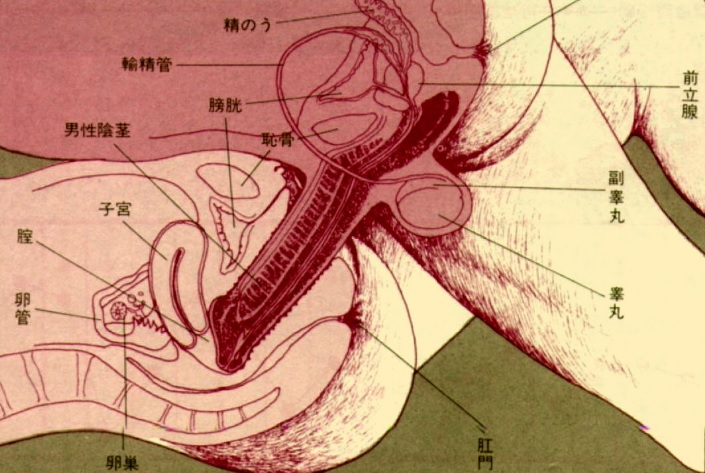
Inguinal hernia Diagram of an indirect, scrotal inguinal hernia ( median view from the left). Diagram of an indirect, scrotal inguinal hernia ( median view from the left). By far the most common hernias (up to 75% of all abdominal hernias) are the so-called inguinal hernias. For a thorough understanding of inguinal hernias, much insight is needed in the anatomy of the inguinal canal. Inguinal hernias are further divided into the more common indirect inguinal hernia (2/3, depicted here), in which the inguinal canal is entered via a congenital weakness at its entrance (the internal inguinal ring), and the direct inguinal hernia type (1/3), where the hernia contents push through a weak spot in the back wall of the inguinal canal. Inguinal hernias are more common in men than women while femoral hernias are more common in women.

There are lots of fallacies about the missionary position being the best position for getting pregnant. With the woman on her back and her partner on top, it is thought that gravity will assist the sperm to swim upwards towards the egg.

At URBN Dental, we offer the best dental services and highest quality care for your gum tissue health. Proper flossing techniques prevent your gum tissue from swelling, which often occurs from food and debris catching between your teeth. A routine dental cleaning every 6 months is recommended to maintain gum tissue health. Skipping bi annual checkups and improper flossing techniques often lead to periodontal disease which usually require a dental deep cleaning to undo tissue damage.
Forzest is FDA approved medicine, it is used bt men to improve erectile dysfunction dusring intercourse session with partner. for more information related side effects, dosage, etc kindly visit to http://www.medstorerx.com/forzest.aspx

A spontaneous vaginal delivery (SVD) occurs when a pregnant woman goes into labor with or without use of drugs or techniques to induce labor, and delivers her baby in the normal manner, without forceps, vacuum extraction, or a cesarean section. Assisted vaginal delivery (AVD) occurs when a pregnant woman goes into labor with or without the use of drugs or techniques to induce labor, and requires the use of special instruments such as forceps or a vacuum extractor to deliver her baby vaginally.
Liposuction surgery is used to reduce the extra fat from your body with the very safe surgical process but you must consult with your Surgeon first when deciding about using this surgery to meet your body fat needs.
Vaser Lipo was Rs. 65000 per region. Now at Rs. 50,000 per Region
Offer valid till 31st March only
Vaser Liposuction technology helps to reduce the healing time and increase effective skin contraction, giving you smooth, slim results. With Liposuction there are no stitches, only a single 1cm small incision giving you permanent large result.
For further information, are available visit our website:
http://www.imageclinic.org/liposuction.html
Your Query for Chat and call +91-9818369662, 9958221983 (WhatsApp)

Genital warts are soft growths that appear on the genitals. Genital warts are a sexually transmitted infection (STI) caused by certain strains of the human papillomavirus (HPV). These skin growths can cause pain, discomfort, and itching. They are especially dangerous for women because some types of HPV can also cause cancer of the cervix and vulva.