Top videos
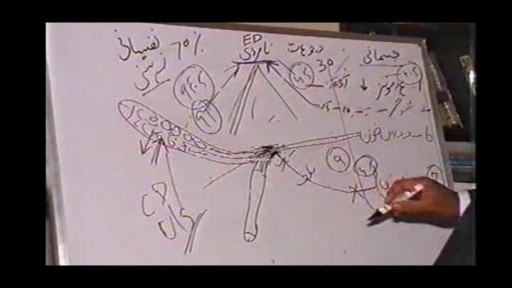
Is Dropping a disease, Is Flow of Thin Semen a disease 5 جریان، کچی منی کوئی بیماری ہے All Solution of Male Disorder Male Infertility Diagnostic and Treatment Re-Slim Care Latest Technology in Pakistan Dr. Aslam Naveed is a well known sexologist in Pakistan. He has treated more than 1 Lac patients since last 30 years of clinical Practice in sexology, he knows how to help the people facing sexual disorders. Contact: 02134965050, 03432821919 www.sexologistpakistan.com https://www.facebook.com/menssexcareclinic/ https://youtu.be/_fRbtwWtLoE Part 1 https://youtu.be/S17bCnwCLuI Part 2 https://youtu.be/CPAXxkdz7mM Part 3 https://youtu.be/Jgn6VT7s2G8 Part 4 https://youtu.be/fylxbK4azvs Part 5 https://youtu.be/Zb8TcdgJ7Io Part 6 https://youtu.be/0wbDDNAwsmo Part 7 https://youtu.be/gHDmwfsMgTw Part 8 https://youtu.be/IasXoRKUlV4 Part 9 ADDRESS: Men’s Care Modern Hospital, Opposite, Safari Park, University Road, Karachi, Pakistan.
Peripheral Vascular Examination OSCE - Clinical Skills - Dr Gill
In the cardiovascular examination, particularly in the case of an OSCE station, we conclude the examination often by stating that the examiner would want to perform:
- An ECG
- Check full blood count
- and "do a peripheral vascular examination
In this video, we demonstrate that oft-talked about, but comparatively less common examination.
Starting off, with the examination of the hands, the radial, brachial and carotid pulses. before moving down to assess for a AAA, checking the femoral and popliteal pulses, before wrapping up around the ankle with the posterior tibial and dorsalis pedis pulses
For completeness, the cardiovascular examination is demonstrated here
https://www.youtube.com/watch?v=ECs9O5zl6XQ&t=2s
#PeripheralVascular #ClinicalSkills #DrGill
Bone fractures are generally caused by injury, such as a fall, car accident, or sports injury, however, bone fractures can also be caused by osteoporosis. If you have a bone fracture, you must get immediate medical attention and keep the fracture immobilized until you can get help. After the fracture has been immobilized, you can then begin natural remedies to help heal broken bones fast.
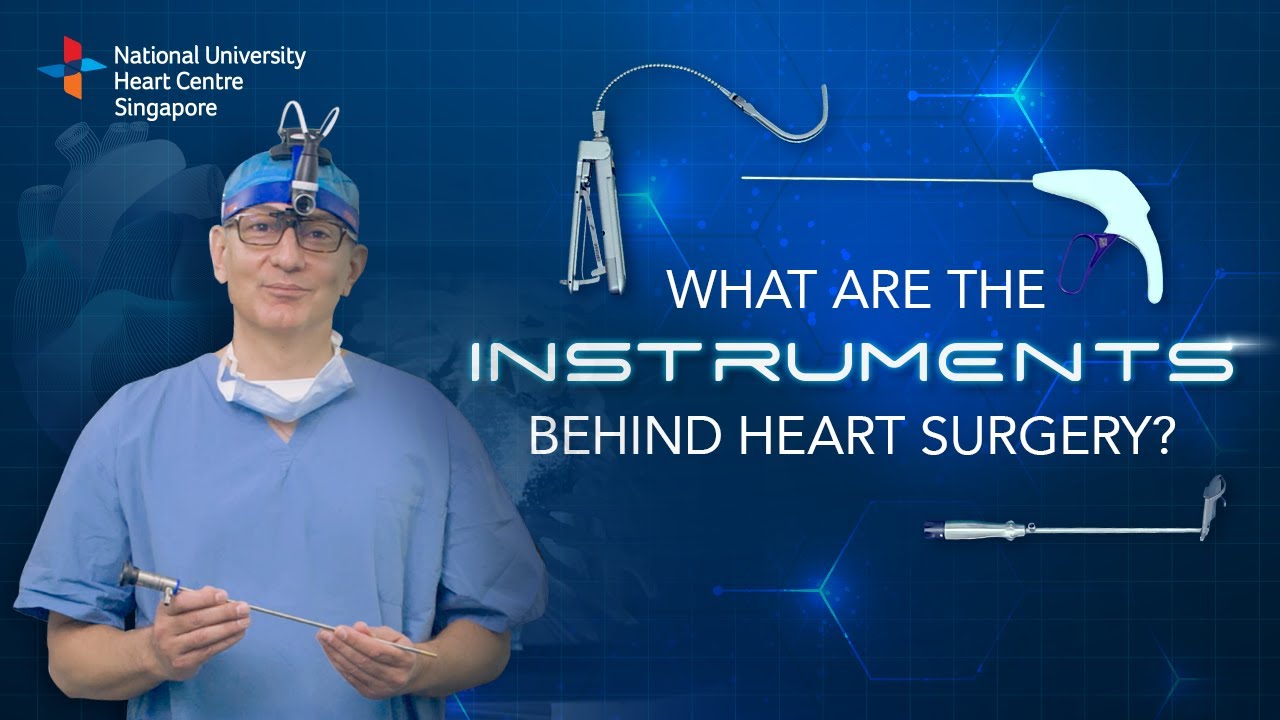
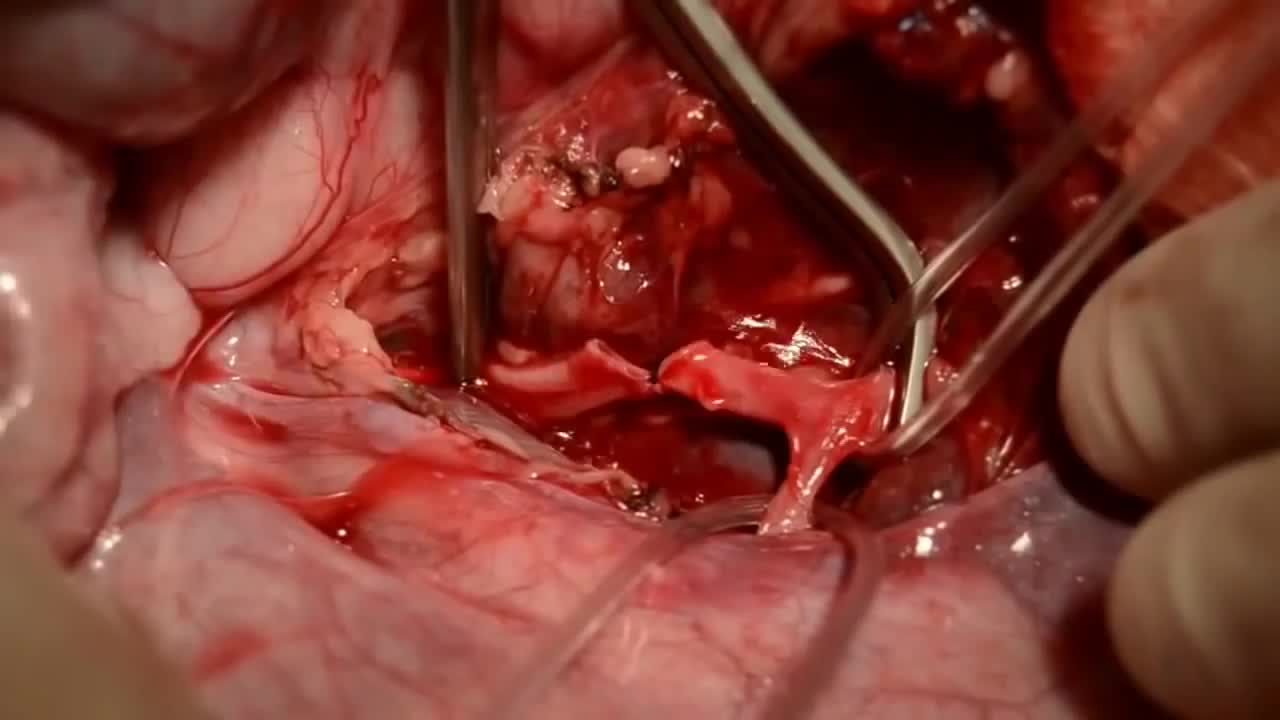
Instruments at work, innovation at play. 🔍
Watch on to discover the behind-the-scenes instruments utilised by our NUHCS cardiac surgery expert, A/Prof Theodoros Kofidis, Head of NUHCS' Department of Cardiac, Thoracic & Vascular Surgery (CTVS), for keyhole heart operations. 🔑
To find out more about Minimally Invasive Heart Surgery @ NUHCS, visit: https://[a]www.nuhcs.com.sg%2FOur-Services%2FSpecialties%2FPages%2FMinimally-Invasive-Cardiac-Surgery-Programme.aspx[/a]
Connect with us:
Instagram: @nuhcsofficial
Facebook: www.facebook.com/nuhcs
Website: www.nuhcs.com.sg
LinkedIn: www.linkedin.com/company/nuhcs
To make an appointment with the NUHCS Heart Clinic, email us at appointment@nuhs.edu.sg
#NUHCS #cardiacsurgery #heartsurgery #keyholesurgery #minimallyinvasive
All Solution of Male Disorder Male Infertility Diagnostic and Treatment Re-Slim Care Latest Technology in Pakistan Dr. Aslam Naveed is a well known sexologist in Pakistan. He has treated more than 1 Lac patients since last 30 years of clinical Practice in sexology, he knows how to help the people facing sexual disorders. Contact: 02134965050, 03432821919, 0345-8314663 http://www.sexologistpakistan.com/ https://www.facebook.com/menssexcareclinic/ https://www.youtube.com/channel/UCagSSgdEgQJWl_xfFM12BwA https://twitter.com/bettersexcare https://www.instagram.com/dr.aslamnaveed/ ADDRESS: Men’s Care Modern Hospital, Opposite, Safari Park, University Road, Karachi, Pakistan.
http://endyourdepression.plus101.com ---Depression Alternative Medicine Remedies. Learn more about your own, unique depression symptoms and pin-point exactly which type of depression you are suffering from. Accurately discover what is causing your depression... and why it keeps coming back no matter which drugs you take or which treatments you try. Uncover the simple methods that allow you to switch your mind away from depression and towards real happiness. Gain real insight into why most depression treatments only make your symptoms worse. Depression Alternative Medicine Remedies depressive major disorder symptoms signs medication treatment clinical causes anxiety teen help hurts self test medicine antidepression types anxiety severe

Body Restorations will do an “Early Assessment” when you come in for physiotherapy; this allows therapists to identify the more complicated cases quickly and get started with treatment right away. If you are feeling pain now, it is best that you seek treatment as soon as possible. Research has proven that people who seek treatment for their pain immediately have less of a chance of it becoming an issue later own. Early intervention is always the best option. Visit - https://stalbertphysiotherapy.com/contact/

Hernia symptoms test diagnosis and surgery - This lecture explains about hernia symptoms, diagnosis and surgery to cure hernia disease. Stay tuned to this video lecture to get answer of the following questions -
what is hernia disease?
hernia symptoms?
hernia test?
hernia diagnosis?
hernia treatment?
Specifically the hernia surgery is explained in this video. So stay tuned to this video to more about hernia repair and details about hernia symptoms and diagnosis.
Watch this video lecture if you have hernia and want to know about hernia surgery and hernia operation related information.
For more information, log on to-
http://[a]www.shomusbiology.com%2F[/a]
Get Shomu's Biology DVD set here-
http://[a]www.shomusbiology.com%2F[/a]dvd-store/
Download the study materials here-
http://shomusbiology.com/bio-materials.html
Remember Shomu’s Biology is created to spread the knowledge of life science and biology by sharing all this free biology lectures video and animation presented by Suman Bhattacharjee in YouTube. All these tutorials are brought to you for free. Please subscribe to our channel so that we can grow together. You can check for any of the following services from Shomu’s Biology-
Buy Shomu’s Biology lecture DVD set- [a]www.shomusbiology.com%2Fdvd-store[/a]
Shomu’s Biology assignment services – [a]www.shomusbiology.com%2Fassignment[/a] -help
Join Online coaching for CSIR NET exam – [a]www.shomusbiology.com%2Fnet-coaching[/a]
We are social. Find us on different sites here-
Our Website – www.shomusbiology.com
Facebook page- https://www.facebook.com/ShomusBiology/
Twitter - https://twitter.com/shomusbiology
SlideShare- www.slideshare.net/shomusbiology
Google plus- https://plus.google.com/113648584982732129198
LinkedIn - https://www.linkedin.com/in/su....man-bhattacharjee-2a
Youtube- https://www.youtube.com/user/TheFunsuman
Thank you for watching the health tutorial video on Hernia symptoms test diagnosis and surgery.

A Beautiful Smile at Lake Pointe is Sugar Land premier dentistry practice. Dr. Lance Jue has been serving patients' preventive, restorative and cosmetic dental needs here in Sugar Land for over 19 years. Book an appointment online now with Dr. Lance Jue
Throughout the body, there are several points at which blood vessels unite. The junctions are termed anastomoses. In the simplest sense, an anastomosis is any connection (made surgically or occurring naturally) between tube-like structures. Naturally occurring arterial anastomoses provide an alternative blood supply to target areas in cases where the primary arterial pathway is obstructed. They are most abundant in regions of the body where the blood supply may can be easily damaged or blocked (such as the joints or intestines). This article focuses on the arterial anastomotic networks of the upper limb.
If you're pregnant, you're likely paying extra close attention to your body. If you happen to feel a cramp you may worry that it is a sign of a miscarriage. While the first trimester is the most common time for miscarriages, there are other reasons for cramps. Whether it signals a miscarriage depends on when it occurs, the severity of the cramping, and whether you're experiencing other symptoms alongside it.