Top videos

She is a twenty years young female presented with large cystic swelling in anterior aspect of neck. The swelling was of size 6cmx 6cm x5 cm ,tense tender, cystic just above sternal nutch.This was diagnosed as large neck abscess ./nRepeated aspiration done but the swelling reappeared. So Incision & Drainage planned under local anaesthesia./nPatient in supine position. Surgery part painted and draped. Local anaesthesia 2% xylocaine with adrenaline used for field block.After giving local anaesthesia, I used a no 11 blade for stab incision at the most prominent part of the swelling, where skin was thin and fluctuation present./nPus drained form that opening. Little dilatation of opening to be done with artery forceps or sinus forceps. Complete pus drainage to be ensured.Little finger can be introduced inside the pus cavity to ensure proper drainage of pus. The cavity I use to clean with a gauge piece. If necessary curette biopsy can be taken from the wall of the cavity.These wounds usually need daily proper dressing for faster healing.
In dark or dim light, the pupil dilates to allow more light into the eye to improve vision. Normal pupil size tends to range between 2.0 and 5.0 millimeters, depending on the lighting. The younger you are, the larger your pupils tend to be.

Curious about physiotherapy or wanting to know how to properly perform an exercise? Check us out on Social Media! Facebook: https://www.facebook.com/striveptandperformance/ Instagram: https://www.instagram.com/striveptandperf/ Twitter: https://twitter.com/StrivePTandPerf Blog: http://www.strivept.ca/blog
The best way to make condoms work as well as possible is to use them correctly every single time you have vaginal, oral, and anal sex. That means wearing it the whole time, from start to finish. Make sure the condom is rolled on your penis the right way before there’s any skin-to-skin genital contact. Read more about how to use condoms correctly.
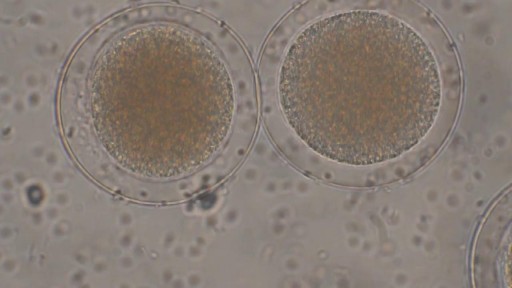
Sperm Meets Egg: Weeks 1 to 3 of Pregnancy. Something magical is about to happen! Watch as the ovulation process occurs, and then millions of sperm swim upstream on a quest to fertilize an egg. Your due date is calculated from the first day of your last menstrual period
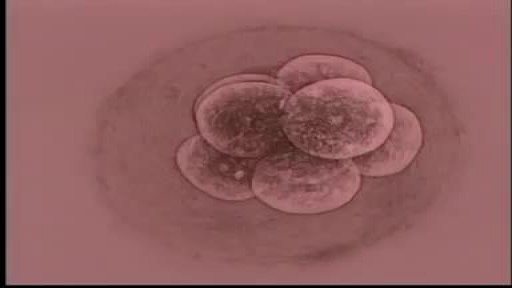
Almost all the cells in your body were produced by mitosis. The only exception is sperm or eggs which are produced by a different type of cell division called meiosis. During fertilization the sperm and egg unite to form a single cell called the zygote which contains chromosomes from both the sperm and egg.

Curious about physiotherapy or wanting to know how to properly perform an exercise? Check us out on Social Media! Facebook: https://www.facebook.com/striveptandperformance/ Instagram: https://www.instagram.com/striveptandperf/ Twitter: https://twitter.com/StrivePTandPerf Blog: http://www.strivept.ca/blog

There can be a number of psychological triggers that cause nightmares in adults. For example, anxiety and depression can cause adult nightmares. Post-traumatic stress disorder (PTSD) also commonly causes people to experience chronic, recurrent nightmares. Nightmares in adults can be caused by certain sleep disorders
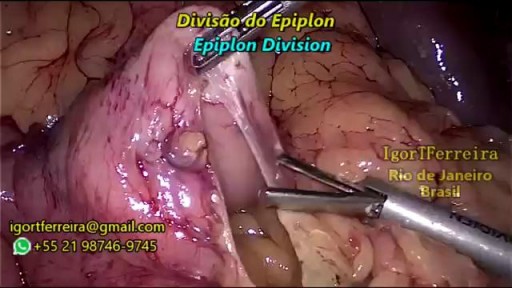
a sleeve gastrectomy with very few edditing. During the start 3 smal spleen perforations caused by Veres Needle were identified, caused by a giant spleen undentified on pre operatory ultrasound. They were controled with gauze compression and at the end of the surgery surgicel was placed and no complications were observed. Patient discharged 3 days after the surgery.

A ventricular assist device (VAD) — also known as a mechanical circulatory support device — is an implantable mechanical pump that helps pump blood from the lower chambers of your heart (the ventricles) to the rest of your body. A VAD is used in people who have weakened hearts or heart failure. Although a VAD can be placed in the left, right or both ventricles of your heart, it is most frequently used in the left ventricle. When placed in the left ventricle it is called a left ventricular assist device (LVAD). You may have a VAD implanted while you wait for a heart transplant or for your heart to become strong enough to effectively pump blood on its own. Your doctor may also recommend having a VAD implanted as a long-term treatment if you have heart failure and you're not a good candidate for a heart transplant.

Is it possible to prevent cytomegalovirus infection? Is there a CMV vaccine? Cytomegalovirus (CMV) infection facts CMV is a common virus in the same family as herpesvirus, and it can infect anyone. CMV is spread by direct contact of body fluids, such as saliva, blood, urine, semen, vaginal fluids, and breast milk. Thus breastfeeding, blood transfusions, organ transplants, and sexual contact are possible modes of transmission. Most healthy people do not experience any symptoms when infected with CMV, and it does not pose a serious health concern. A majority of adults have antibodies consistent with past infection. Most healthy children and adults who do have symptoms will recover from CMV infection without complications and do not require antiviral treatment.