Top videos
The hepatitis E virus, responsible for major epidemics of viral hepatitis in subtropical and tropical countries, was cloned only 7 years ago.1 Hepatitis E was found to belong to the family of Caliciviridae, which includes the Norwalk virus—a common cause of gastroenteritis in humans—and consists of a single, plus-strand RNA genome of approximately 7.2 kb without an envelope (Fig. 1). The virus contains at least three open reading frames encoding viral proteins against which antibodies are made on exposure. These antibodies, especially those against the capsid protein derived from the second open reading frame2 and a protein of unknown function derived from the third open reading frame, are detected by currently available serologic assays. Retrospective studies on stored sera of past epidemics of viral hepatitis in Mexico, Africa, Afghanistan, Pakistan, India, Bangladesh, Burma, Nepal, and Borneo have revealed that all were caused by strains of hepatitis E. In addition, hepatitis E was found to be responsible for the hepatitis epidemic in the southern part of Xinjiang, China, in which 120,000 persons became infected between September 1986 and April 1988.3 Hepatitis E predominantly affects young adults (15 to 40 years old). The symptoms of hepatitis E are similar to those of hepatitis A. Frequently, a prodrome consisting of anorexia, nausea, low-grade fever, and right upper abdominal pain is present 3 to 7 days before jaundice develops. Aminotransferase levels peak (usually between 1,000 and 2,000 U/L) near the onset of symptoms; bilirubin levels (10 to 20 mg/dL) peak later. Jaundice usually resolves after 1 to 2 weeks. In about 10% of cases, the disease is fulminant—especially in pregnant women, among whom mortality rates as high as 20% due to hemorrhagic and thrombotic complications have been reported. No evidence has suggested that hepatitis E can cause chronic infection. Transmission is by the fecal-oral route, predominantly through fecally contaminated drinking water supplies. In addition, however, preliminary reports have suggested transmission of the hepatitis E virus through blood transfusions. Volunteer studies confirmed the presence of the virus in serum and feces before and during clinical disease.4 The virus is shed into feces approximately 1 week before symptoms develop. The incubation period varies from 2 to 9 weeks (mean duration, approximately 45 days). Until now, a few reports had described symptomatic hepatitis E acquired in Europe;5, 6 all patients with symptomatic hepatitis E in the United States were travelers returning from Mexico, Africa, or the Far East, in whom hepatitis E developed after their return home.7 In this issue of the Mayo Clinic Proceedings (pages 1133 to 1136), Kwo and associates describe a case of hepatitis E in a man who had not left the United States during the previous 10 years. Specific serologic tests for hepatitis E virus IgG (enzyme immunoassays and a fluorescent antibody blocking assay) and IgM8 (US strain-specific enzyme-linked immunosorbent assay with use of synthetic polypeptides deduced from the viral genome, as shown in Figure 1), developed at Abbott Laboratories (IgG and IgM) as well as at the Centers for Disease Control and Prevention (IgG), were used to prove that the patient indeed had acute hepatitis E. Researchers at Abbott Laboratories have prepared a report that describes most of the viral genome in this patient (Fig. I).8 Their results are interesting because this strain from the United States differs considerably from hepatitis E strains isolated in Mexico, Burma, Pakistan, or China. Furthermore, the sequence of the US strain is highly homologous (98% and 94% homology at the amino acid level to the second and third open reading frames, respectively) to a recently isolated hepatitis E strain from American swine.9 This finding suggests that, in the United States, hepatitis E is a zoonosis with the swine population as one of its hosts. This relationship would confirm earlier studies in Asia, where swine were also found to carry variants of the hepatitis E virus.10 Why are these two recent discoveries important for medicine in the United States? First, other sporadic, locally acquired cases of acute hepatitis may be caused by hepatitis E. Second, these back-to-back discoveries strongly suggest that a common natural host for hepatitis E is present in countries with more moderate climates. Because swine do not seem to experience any symptoms associated with infection and because symptoms in humans can be minor or absent, we now may also have an explanation for the 1 to 2% of positive hepatitis E serologic results in blood donors in the United States,11 Netherlands,12 and Italy,6 countries with large swine staples. Clearly, more research needs to be done to confirm this hypothesis. Third, in countries with more moderate climates, hepatitis E may often result in a subclinical infection. Is this variation in manifestation due to less virulent strains, and do sequence variations determine virulence? Fourth, swine may be used as an animal model for study of the disease as well as vaccine development.
What Causes Ulcers? No single cause has been found for ulcers. However, it is now clear that an ulcer is the end result of an imbalance between digestive fluids in the stomach and duodenum. Most ulcers are caused by an infection with a type of bacteria called Helicobacter pylori (H. pylori). Factors that can increase your risk for ulcers include: Use of painkillers called nonsteroidal anti-inflammatory drugs (NSAIDs), such as aspirin, naproxen (Aleve, Anaprox, Naprosyn, and others), ibuprofen (Motrin, Advil, some types of Midol, and others), and many others available by prescription; even safety-coated aspirin and aspirin in powered form can frequently cause ulcers. Excess acid production from gastrinomas, tumors of the acid producing cells of the stomach that increases acid output (seen in Zollinger-Ellison syndrome) Excessive drinking of alcohol Smoking or chewing tobacco Serious illness Radiation treatment to the area What Are the Symptoms of an Ulcer? An ulcer may or may not have symptoms. When symptoms occur, they may include: A gnawing or burning pain in the middle or upper stomach between meals or at night Bloating Heartburn Nausea or vomiting In severe cases, symptoms can include: Dark or black stool (due to bleeding) Vomiting blood (that can look like "coffee-grounds") Weight loss Severe pain in the mid to upper abdomen
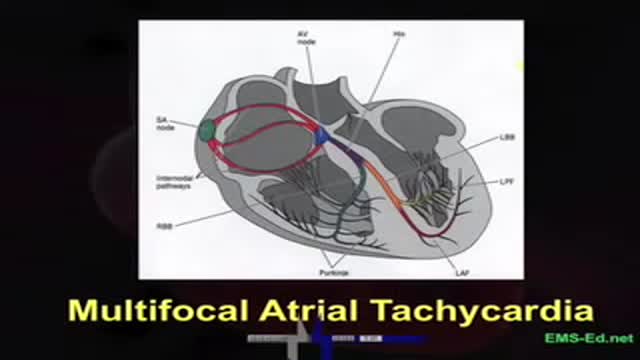
EKG Interpretation Part 3
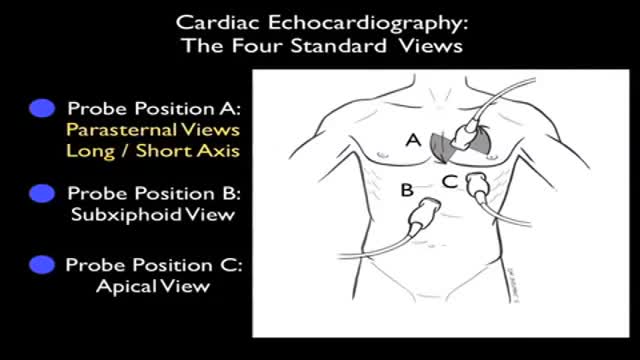
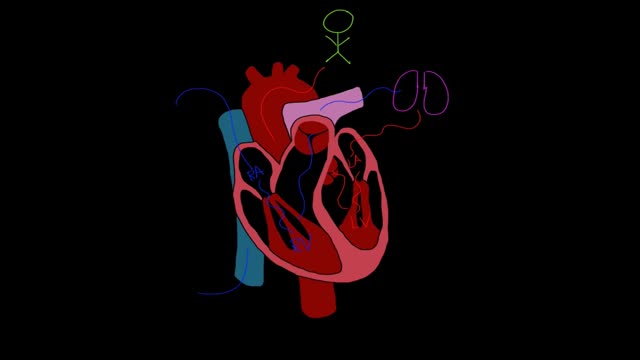
Ultrasound of Heart
Heart failure, sometimes known as congestive heart failure, occurs when your heart muscle doesn't pump blood as well as it should. Certain conditions, such as narrowed arteries in your heart (coronary artery disease) or high blood pressure, gradually leave your heart too weak or stiff to fill and pump efficiently. Not all conditions that lead to heart failure can be reversed, but treatments can improve the signs and symptoms of heart failure and help you live longer. Lifestyle changes — such as exercising, reducing salt in your diet, managing stress and losing weight — can improve your quality of life. One way to prevent heart failure is to control conditions that cause heart failure, such as coronary artery disease, high blood pressure, diabetes or obesity.
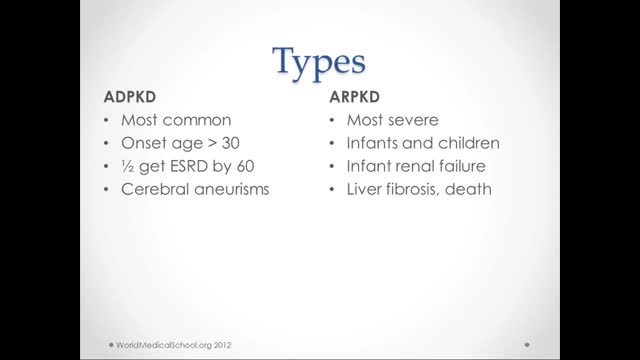
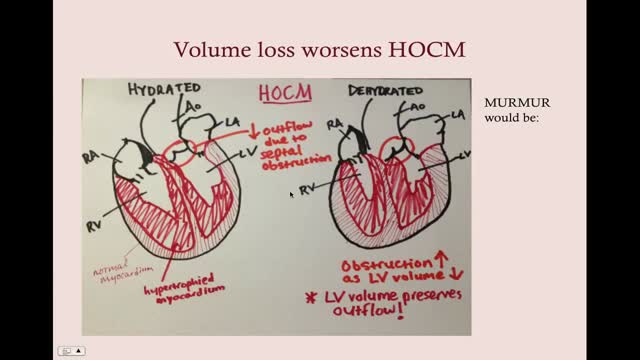
What is polycystic kidney disease? Polycystic kidney disease (also called PKD) causes numerous cysts to grow in the kidneys. These cysts are filled with fluid. If too many cysts grow or if they get too big, the kidneys can become damaged. PKD cysts can slowly replace much of the kidneys, reducing kidney function and leading to kidney failure. How common is PKD? In the United States about 600,000 people have PKD. It is the fourth leading cause of kidney failure. It is found in all races and occurs equally in men and women. It causes about 5% of all kidney failure. What other organs besides the kidney are affected by PKD? PKD can affect other organs besides the kidney. People with PKD may have cysts in their liver, pancreas, spleen, ovaries, and large bowel. Cysts in these organs usually do not cause serious problems, but can in some people. PKD can also affect the brain or heart. If PKD affects the brain, it can cause an aneurysm. An aneurysm is a bulging blood vessel that can burst, resulting in a stroke or even death. If PKD affects the heart, the valves can become floppy, resulting in a heart murmur in some patients. What are the clues that someone has PKD? Most people do not develop symptoms until they are 30 to 40 years old. The first noticeable signs and symptoms may include: Back or side pain An increase in the size of the abdomen Blood in the urine Frequent bladder or kidney infections High blood pressure High blood pressure is the most common sign of PKD. Occasionally, patients may develop headaches related to high blood pressure or their doctors may detect high blood pressure during a routine physical exam. Because high blood pressure can cause kidney damage, it is very important to treat it. In fact, treatment of high blood pressure can help slow or even prevent kidney failure. Fluttering or pounding in the chest About 25% of PKD patients have a so-called floppy valve in the heart, and may experience a fluttering or pounding in the chest as well as chest pain. These symptoms almost always disappear on their own but may be the first hint that someone has PKD. How is PKD diagnosed? Ultrasound is the most reliable, inexpensive and non-invasive way to diagnose PKD. If someone at risk for PKD is older than 40 years and has a normal ultrasound of the kidneys, he or she probably does not have PKD. Occasionally, a CT scan (computed tomography scan) and MRI (magnetic resonance imaging) may detect smaller cysts that cannot be found by an ultrasound. MRI is used to measure and monitor volume and growth of kidneys and cysts. In some situations, genetic testing might also be done. This involves a blood test that checks for abnormal genes that cause the disease. Genetic testing is not recommended for everyone. The test is costly, and it also fails to detect PKD in about 15% of people who have it. However, genetic testing can be useful when a person: has an uncertain diagnosis based on imaging tests has a family history of PKD and wants to donate a kidney is younger than 30-years old with a family history of PKD and a negative ultrasound, and is planning to start a family
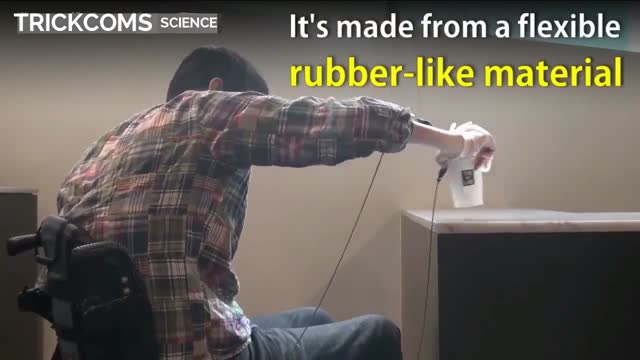
Robot helps disabled patients regain control of their hands 1
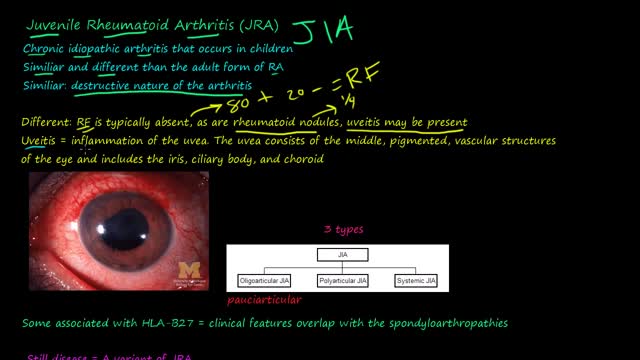
Juvenile rheumatoid arthritis, also known as juvenile idiopathic arthritis, is the most common type of arthritis in children under the age of 17. Juvenile rheumatoid arthritis causes persistent joint pain, swelling and stiffness. Some children may experience symptoms for only a few months, while others have symptoms for the rest of their lives. Some types of juvenile rheumatoid arthritis can cause serious complications, such as growth problems and eye inflammation. Treatment of juvenile rheumatoid arthritis focuses on controlling pain, improving function and preventing joint damage.
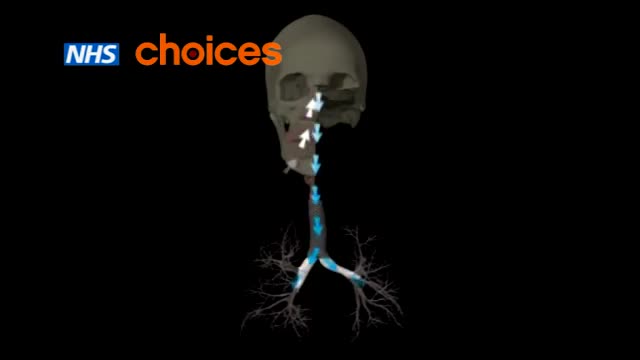
Asthma is a condition in which your airways narrow and swell and produce extra mucus. This can make breathing difficult and trigger coughing, wheezing and shortness of breath. For some people, asthma is a minor nuisance. For others, it can be a major problem that interferes with daily activities and may lead to a life-threatening asthma attack. Asthma can't be cured, but its symptoms can be controlled. Because asthma often changes over time, it's important that you work with your doctor to track your signs and symptoms and adjust treatment as needed.
men health,women health,organ devloping ,female problems soultion,
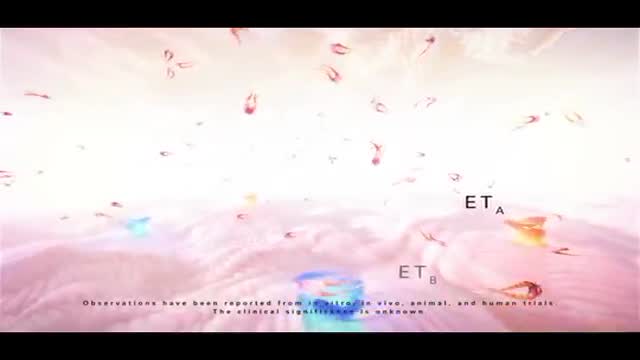
Pulmonary hypertension is a type of high blood pressure that affects the arteries in your lungs and the right side of your heart. In one form of pulmonary hypertension, tiny arteries in your lungs, called pulmonary arterioles, and capillaries become narrowed, blocked or destroyed. This makes it harder for blood to flow through your lungs, and raises pressure within your lungs' arteries. As the pressure builds, your heart's lower right chamber (right ventricle) must work harder to pump blood through your lungs, eventually causing your heart muscle to weaken and fail. Some forms of pulmonary hypertension are serious conditions that become progressively worse and are sometimes fatal. Although some forms of pulmonary hypertension aren't curable, treatment can help lessen symptoms and improve your quality of life. Pulmonary hypertension care at Mayo Clinic
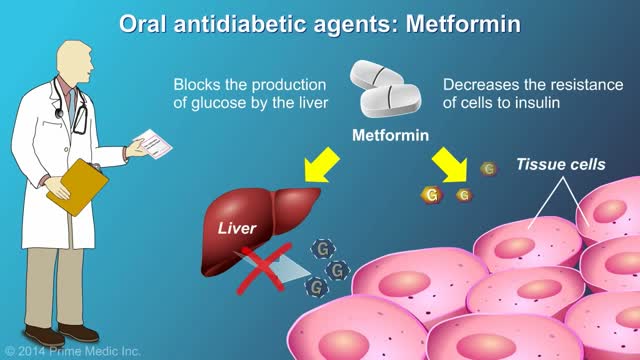
protecting the body from damage caused by hyperglycemia cannot be overstated. In the United States, 57.9% of diabetic patients have one or more diabetes complications, and 14.3% have three or more.1 Strict glycemic control is the primary method of reducing the development and progression of microvascular complications, such as retinopathy, nephropathy, and neuropathy. Aggressive treatment of dyslipidemia and hypertension decreases macrovascular complications.2-4 Glycemic Control There are two primary techniques available for physicians to assess the quality of a patient’s glycemic control: self-monitoring of blood glucose (SMBG) and interval measurement of hemoglobin A1c (HbA1c).
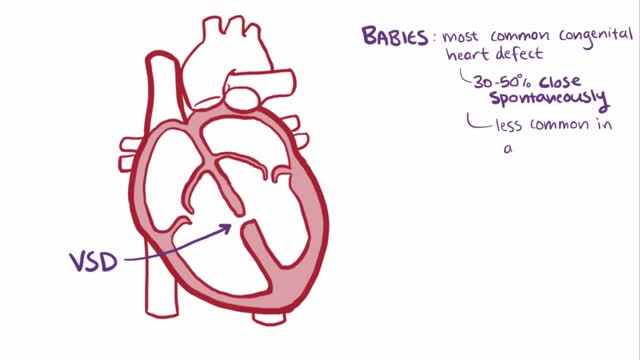
A ventricular septal defect (VSD), a hole in the heart, is a common heart defect that's present at birth (congenital). The hole occurs in the wall that separates the heart's lower chambers (septum) and allows blood to pass from the left to the right side of the heart. The oxygen-rich blood then gets pumped back to the lungs instead of out to the body, causing the heart to work harder. A small ventricular septal defect may cause no problems, and many small VSDs close on their own. Larger VSDs need surgical repair early in life to prevent complications.
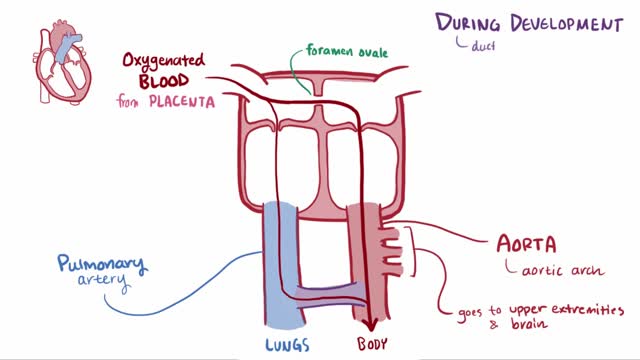
Patent ductus arteriosus (PDA) is a persistent opening between two major blood vessels leading from the heart. The opening, called the ductus arteriosus, is a normal part of a baby's circulatory system before birth that usually closes shortly after birth. If it remains open, however, it's called a patent ductus arteriosus. A small patent ductus arteriosus often doesn't cause problems and might never need treatment. However, a large patent ductus arteriosus left untreated can allow poorly oxygenated blood to flow in the wrong direction, weakening the heart muscle and causing heart failure and other complications. Treatment options for a patent ductus arteriosus include monitoring, medications and closure by cardiac catheterization or surgery.
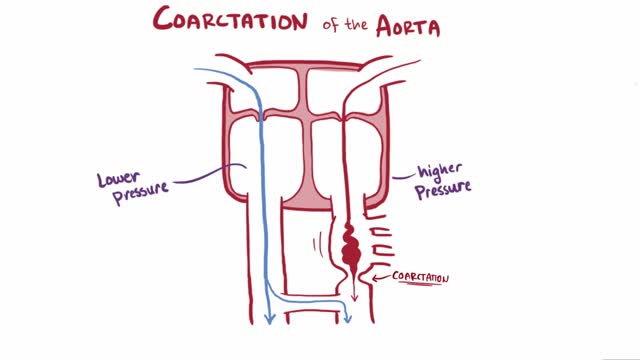
Coarctation of the aorta (CoA[1][2] or CoAo), also called aortic narrowing, is a congenital condition whereby the aorta is narrow, usually in the area where the ductus arteriosus (ligamentum arteriosum after regression) inserts. The word “coarctation” means narrowing. Coarctations are most common in the aortic arch. The arch may be small in babies with coarctations. Other heart defects may also occur when coarctation is present, typically occurring on the left side of the heart. When a patient has a coarctation, the left ventricle has to work harder. Since the aorta is narrowed, the left ventricle must generate a much higher pressure than normal in order to force enough blood through the aorta to deliver blood to the lower part of the body. If the narrowing is severe enough, the left ventricle may not be strong enough to push blood through the coarctation, thus resulting in lack of blood to the lower half of the body. Physiologically its complete form is manifested as interrupted aortic arch
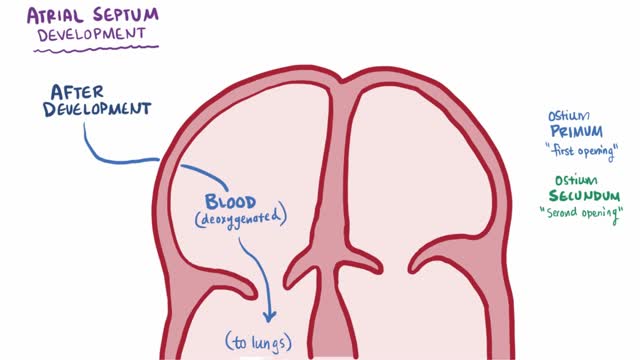
An atrial septal defect (ASD) is a hole in the wall between the two upper chambers of your heart (atria). The condition is present from birth (congenital). Small atrial septal defects may close on their own during infancy or early childhood. Large and long-standing atrial septal defects can damage your heart and lungs. Small defects may never cause a problem and may be found incidentally. An adult who has had an undetected atrial septal defect for decades may have a shortened life span from heart failure or high blood pressure that affects the arteries in the lungs (pulmonary hypertension). Surgery may be necessary to repair atrial septal defects to prevent complications.
Dilated cardiomyopathy is a disease of the heart muscle, usually starting in your heart's main pumping chamber (left ventricle). The ventricle stretches and thins (dilates) and can't pump blood as well as a healthy heart can. The term "cardiomyopathy" is a general term that refers to the abnormality of the heart muscle itself. Dilated cardiomyopathy might not cause symptoms, but for some people it can be life-threatening. A common cause of heart failure — the heart's inability to supply the body with enough blood — dilated cardiomyopathy can also contribute to irregular heartbeats (arrhythmias), blood clots or sudden death. The condition affects people of all ages, including infants and children, but is most common in men ages 20 to 60.
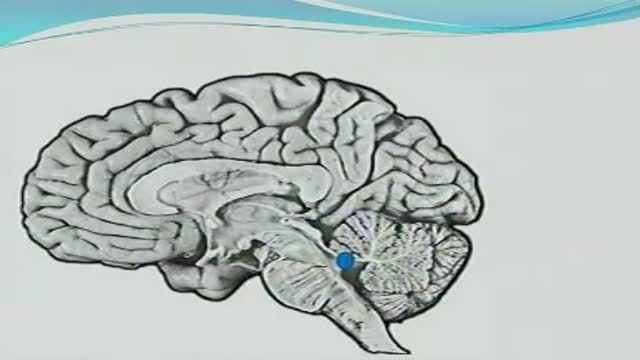
Friedreich's ataxia is an inherited disease that damages your nervous system. The damage affects your spinal cord and the nerves that control muscle movement in your arms and legs. Symptoms usually begin between the ages of 5 and 15. The main symptom is ataxia, which means trouble coordinating movements. Specific symptoms include Difficulty walking Muscle weakness Speech problems Involuntary eye movements Scoliosis (curving of the spine to one side) Heart palpitations, from the heart disease which can happen along with Friedreich's ataxia People with Friedreich's ataxia usually need a wheelchair 15 to 20 years after symptoms first appear. In severe cases, people become incapacitated. There is no cure. You can treat symptoms with medicines, braces, surgery, and physical therapy.
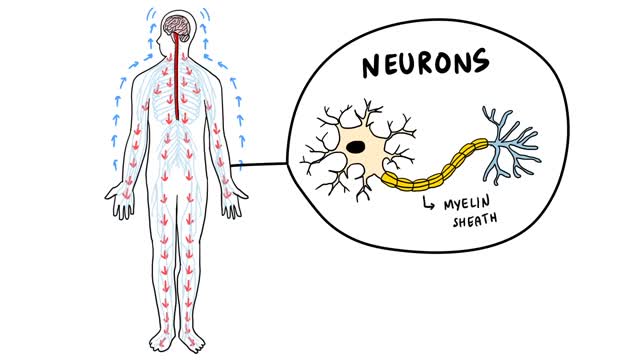
Guillain-Barre (gee-YAH-buh-RAY) syndrome is a rare disorder in which your body's immune system attacks your nerves. Weakness and tingling in your extremities are usually the first symptoms. These sensations can quickly spread, eventually paralyzing your whole body. In its most severe form Guillain-Barre syndrome is a medical emergency. Most people with the condition must be hospitalized to receive treatment. The exact cause of Guillain-Barre syndrome is unknown. But it is often preceded by an infectious illness such as a respiratory infection or the stomach flu. There's no known cure for Guillain-Barre syndrome, but several treatments can ease symptoms and reduce the duration of the illness. Most people recover from Guillain-Barre syndrome, though some may experience lingering effects from it, such as weakness, numbness or fatigue.
Guillain-Barre syndrome is a rare disorder in which your body's immune system attacks your nerves. Weakness and tingling in your extremities are usually the first symptoms. These sensations can quickly spread, eventually paralyzing your whole body. In its most severe form Guillain-Barre syndrome is a medical emergency. Most people with the condition must be hospitalized to receive treatment. The exact cause of Guillain-Barre syndrome is unknown. But it is often preceded by an infectious illness such as a respiratory infection or the stomach flu. There's no known cure for Guillain-Barre syndrome, but several treatments can ease symptoms and reduce the duration of the illness. Most people recover from Guillain-Barre syndrome, though some may experience lingering effects from it, such as weakness, numbness or fatigue.