Top videos
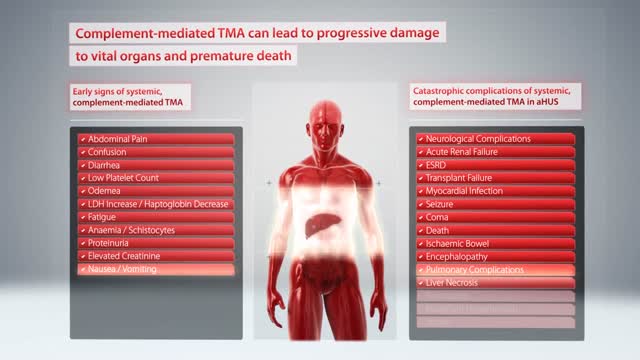
Hemolytic-uremic syndrome (or haemolytic-uraemic syndrome), abbreviated HUS, is a disease characterized by hemolytic anemia (anemia caused by destruction of red blood cells), acute kidney failure (uremia), and a low platelet count (thrombocytopenia).
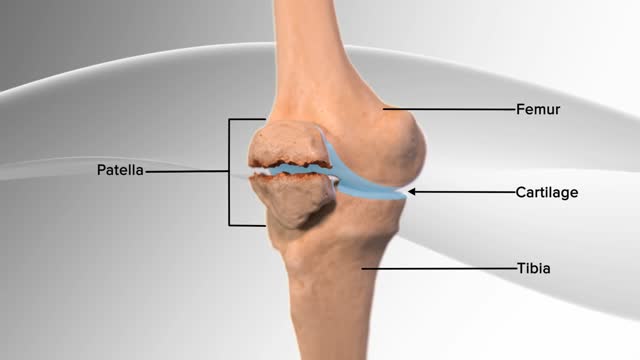
In this knee procedure, the patella is being repaired. The patella is a small, floating bone that glides over the thighbone. It connects the muscles of the thigh to the shinbone, helping the knee to move. The egg‐shell type covering on the underside of the patella and front of the femur allows for smooth motion of the knee.
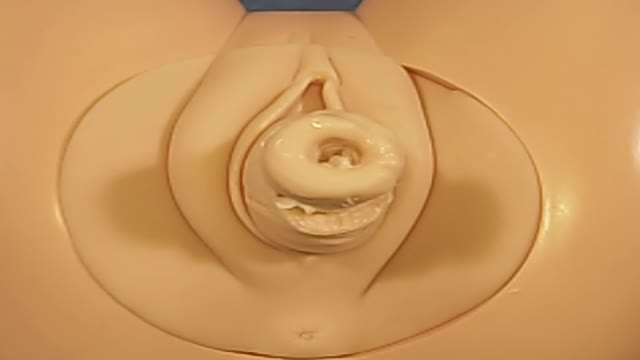
Cerclage is indicated in a patient with a history of painless cervical dilation and a second trimester loss. It is also indicated in a patient with a history of preterm birth and a short cervix found on ultrasound between 16-24 weeks gestation. Cerclage placement occurs after the first trimester in case the pregnancy is genetically abnormal and would likely result in a first trimester loss.

-Traumatic amputation of a body part requires rapid transport of the appendage, which should be wrapped in a saline-moistened gauze, placed in a plastic bag, and transported in a container filled with ice mixed with either saline or sterile water to best preserve the body part and attempt replantation.
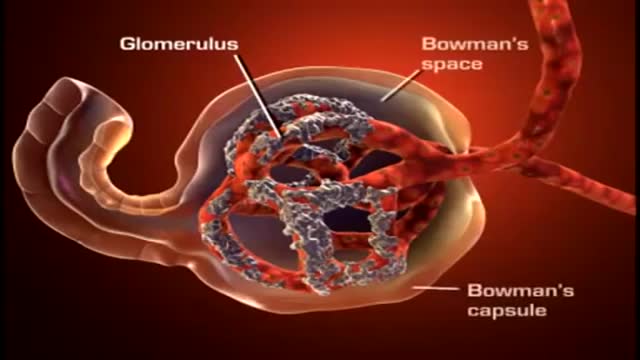
A nephron (from Greek νεφρός (nephros) meaning "kidney") is the basic structural and functional unit of the kidney. Its chief function is to regulate the concentration of water and soluble substances like sodium salts by filtering the blood, reabsorbing what is needed and excreting the rest as urine.
Eyelid surgery, or blepharoplasty, is a surgical procedure to improve the appearance of the eyelids. Surgery can be performed on either the upper and lower lids, or both. Whether you want to improve your appearance or are experiencing functional problems with your eyelids, eyelid surgery can rejuvenate the area surrounding your eyes.

The spine is made flexible by discs located between each vertebra and ligaments made of tough elastic fibers which hold the vertebrae together. The spine gives the body stability and protects the spinal cord which is located in a narrow canal that runs through the center of each vertebra.
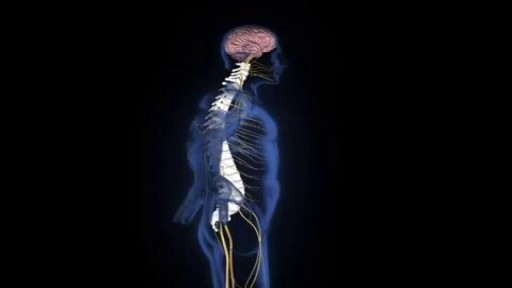
An estimated 12,500 spinal cord injuries occur in the U.S. every year, leaving the injured people, their friends, and their family, to cope with the aftermath of the catastrophe. For many, navigating the challenges of the health care system can feel a bit like going to medical school. Suddenly you're learning a veritable cornucopia of new terms, and may be spending endless hours Googling spinal cord anatomy to fill in the gaps in your knowledge. An educated patient is better equipped to advocate for his or her needs and interests. An education in spinal cord anatomy helps you understand what your doctor is saying, ask intelligent questions, and detect medical errors before they endanger your health.

Eating a high-protein breakfast has been shown to reduce cravings and calorie intake throughout the day (16, 17). Avoid sugary drinks and fruit juice. These are the most fattening things you can put into your body, and avoiding them can help you lose weight (18, 19). Drink water a half hour before meals.

Is it possible to prevent cytomegalovirus infection? Is there a CMV vaccine? Cytomegalovirus (CMV) infection facts CMV is a common virus in the same family as herpesvirus, and it can infect anyone. CMV is spread by direct contact of body fluids, such as saliva, blood, urine, semen, vaginal fluids, and breast milk. Thus breastfeeding, blood transfusions, organ transplants, and sexual contact are possible modes of transmission. Most healthy people do not experience any symptoms when infected with CMV, and it does not pose a serious health concern. A majority of adults have antibodies consistent with past infection. Most healthy children and adults who do have symptoms will recover from CMV infection without complications and do not require antiviral treatment.
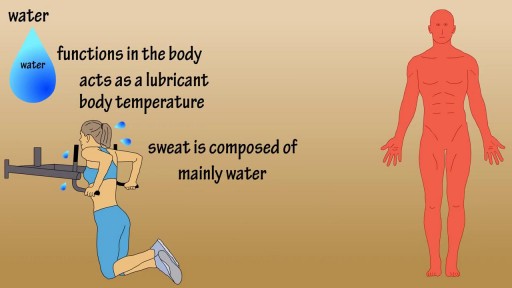
Water is an essential nutrient for the body, as the body loses water through perspiration, breathing, bowel movements, and in urine. Water must be consumed regularly to maintain a sufficient level. Water has many vital functions in the body, including… Serving as a lubricant. Water is a main component of saliva, which helps moisten food making it easier to swallow. Water also helps lubricate joints, reducing friction and inflammation. Water is important in body temperature regulation. When body heat rises, such as during strenuous activities, the body starts to sweat to cool itself. And sweat is made up almost entirely of water.
Like a fine whiskey barrel and wine cellar, cannabis also comes at its best when aged in a dark, cool place. Though there is no steadfast expiration date for cannabis, the method you use for preserving the cannabis makes a big difference in maintaining the buds’ freshness and potency. The question is, how do you store cannabis in a way that could extend its longevity while maintaining the vigor and freshness? Experts have described different methods. However, here are some time-proven methods that are easy and inexpensive and require very less equipment. Use air-tight glass containers to store the weed Use clean air-tight glass containers or jars to store cannabis. You can buy glass containers from any ordinary supermarket or hardware store. The tricky part is to make sure you do leave some air in the container while the air stored with cannabis isn’t in detrimental extent. Always leave 1/4 space at the top of the canister or container. Do not fill the containers to the brim with the buds. If you leave no air, then the buds will dry out. If you have too much air, the buds will get damp and moldy. Freeze your cannabis in a convenient temperature The best way to store your buds is in air-tight glass jars, in a cool and dark place under an ideal temperature between 60 and 70 degrees Fahrenheit. If you need to store a high volume of cannabis, you can freeze them after keeping them completely dry for a period of 4 weeks. On this note, you should know that you must not handle frozen buds until it becomes normal in room temperature as trichomes become brittle and can easily break off in freezing temperature. Refrigerate your cannabis (Not Recommended) Even if you use airtight jars, cannabis can grow mold in the fridge. So, you should avoid storing cannabis in the fridge. If you can’t help but doing it, make sure the weed is completely dry and put them in the back where the humidity and temperature don’t fluctuate. Plastic Baggies (Worst method!) Albeit this is very common among people who aren’t expert in handling cannabis, this is the worst of all storage methods. Cannabis gets brittle and dries out in plastic bags. It also loses its natural smell, and the potency deteriorates sharply. So, it should be avoided entirely or can be used for a short-term if there is no better alternative. Here are some things you should know while storing cannabis - Make sure cannabis has been cured for at least 4 weeks before putting them into long-term storage. Without proper curing before storage, the buds can lose their strength and smoothness. - Sunlight can stop the medicinal qualities of cannabis. Your cannabis, if stored correctly, can maintain its medicinal qualities for a few years. Exposure to Sun will turn your cannabis brown, no matter how you have stored it away. - Air-tight, nonporous glass jar are the best way for storing the buds for long term. You can use metal or plastic box/bag, but that could reduce the smell and taste after a while. - Avoid heat and middling temperature in the place where you store your buds. The ideal temperature is 60-70°F (15-21°C) or under 32°F (0°C). Extra heat, cold or middling temperature cause the cannabis potency to decrease. - Keep your cannabis away from any electronic devices or appliances that will expose the cannabis to heat. Keeping cannabis on top of a microwave, or near a laptop or mobile charge is a bad idea. Now, as you know that how to store cannabis properly and make it last for years, enjoy the best form of your weeds even it comes from the previous year. Do write to us in the comments section if you have any questions. Also, don’t forget to hit the subscribe button below. Visit OnlineMedicalCard.com now to get an MMJ recommendation online in less than 10 minutes.

Tinnitus (TIN-ih-tus) is the perception of noise or ringing in the ears. A common problem, tinnitus affects about 1 in 5 people. Tinnitus isn't a condition itself — it's a symptom of an underlying condition, such as age-related hearing loss, ear injury or a circulatory system disorder