Top videos
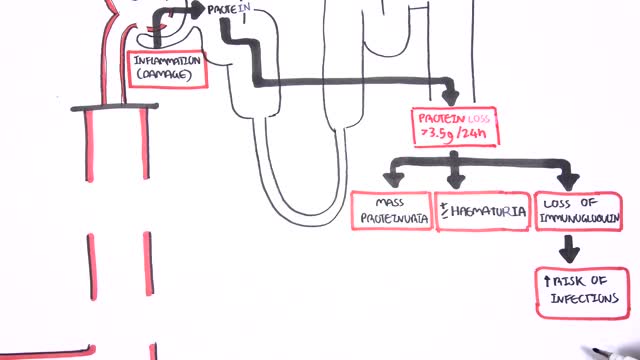
Nephrotic syndrome is a kidney disorder that causes your body to excrete too much protein in your urine. Nephrotic syndrome is usually caused by damage to the clusters of small blood vessels in your kidneys that filter waste and excess water from your blood. Nephrotic syndrome causes swelling (edema), particularly in your feet and ankles, and increases the risk of other health problems. Treatment for nephrotic syndrome includes treating the underlying condition that's causing it and taking medications. Nephrotic syndrome can increase your risk of infections and blood clots. Your doctor may recommend medications and dietary changes to prevent these and other complications of nephrotic syndrome.

The DASH diet is a lifelong approach to healthy eating that's designed to help treat or prevent high blood pressure (hypertension). The DASH diet encourages you to reduce the sodium in your diet and eat a variety of foods rich in nutrients that help lower blood pressure, such as potassium, calcium and magnesium.
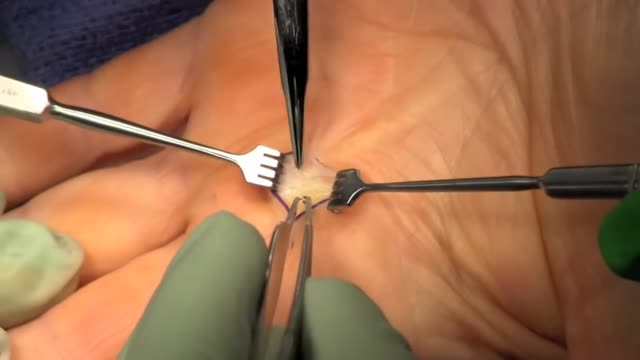
Trigger finger, also known as stenosing tenosynovitis (stuh-NO-sing ten-o-sin-o-VIE-tis), is a condition in which one of your fingers gets stuck in a bent position. Your finger may straighten with a snap — like a trigger being pulled and released. Trigger finger occurs when inflammation narrows the space within the sheath that surrounds the tendon in the affected finger. If trigger finger is severe, your finger may become locked in a bent position. People whose work or hobbies require repetitive gripping actions are at higher risk of developing trigger finger. The condition is also more common in women and in anyone with diabetes. Treatment of trigger finger varies depending on the severity.
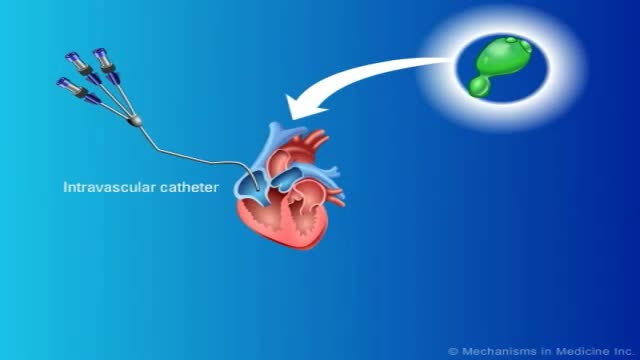
Fungal infections in bone marrow transplant patients. PURPOSE OF REVIEW: Invasive fungal infections have become the leading infectious cause of death in recipients of hematopoietic cell transplantation. Several factors have led to a renaissance in the study of invasive fungal infections.
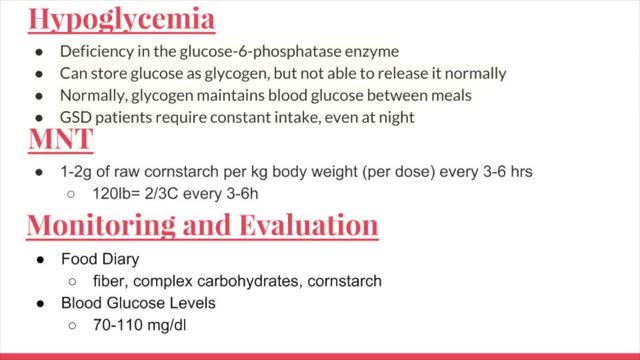
Glycogen storage disease (GSD, also glycogenosis and dextrinosis) is the result of defects in the processing of glycogen synthesis or breakdown within muscles, liver, and other cell types. GSD has two classes of cause: genetic and acquired.
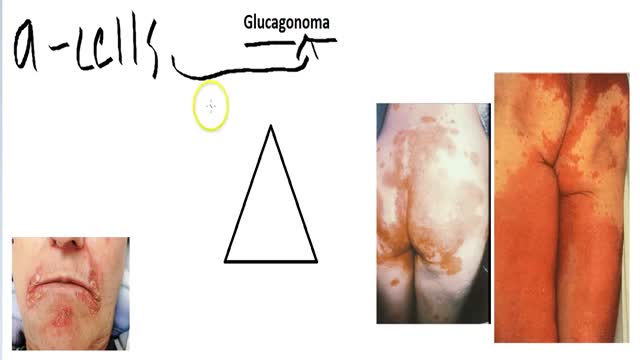
A glucagonoma is a rare tumor of the alpha cells of the pancreas that results in the overproduction of the hormone glucagon. Alpha cell tumors are commonly associated with glucagonoma syndrome, though similar symptoms are present in cases of pseudoglucagonoma syndrome in the absence of a glucagon-secreting tumor.
Alendronate Sodium is used for the following diseases and conditions: osteoporosis, and osteogenesis imperfecta. Alendronate Sodium improves the patient's condition by performing the following functions: slowing down the bone loss and helps to keep the bones strong and less likely to break. Side effects are possible with Alendronate Sodium, but do not always occur. Some of the side effects may be rare but serious. Consult your doctor if you observe any side effects, especially if they do not go away. Alendronate Sodium may cause the following side-effects: stomach pain, constipation, diarrhea, gas, nausea, and jaw pain
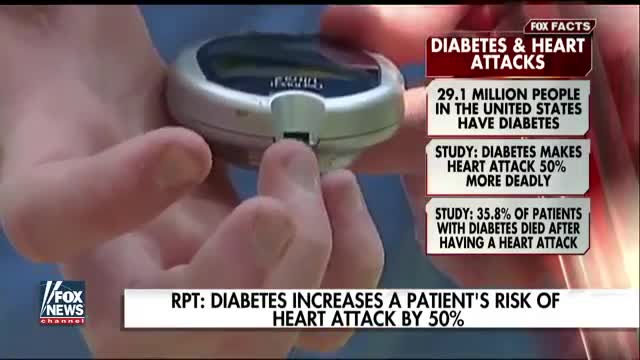
A silent heart attack is a heart attack that has few, if any, symptoms. You may have never had any symptoms to warn you that you've developed a heart problem, such as chest pain or shortness of breath. Having diabetes or prediabetes puts you at increased risk for heart disease and stroke. You can lower your risk by keeping your blood glucose (also called blood sugar), blood pressure, and blood cholesterol close to the recommended target numbersthe levels suggested by diabetes experts for good health. (

The "Get up and go" test is most commonly used to assess postural stability. In this test, the physician instructs the patient to stand up from a chair without assistance, walk a short distance, turn around, return, and sit down again. If the patient is unsteady or has difficulties during the test, further evaluation is necessary.
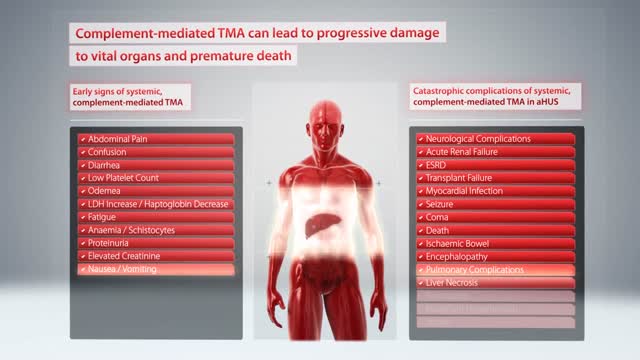
Hemolytic-uremic syndrome (or haemolytic-uraemic syndrome), abbreviated HUS, is a disease characterized by hemolytic anemia (anemia caused by destruction of red blood cells), acute kidney failure (uremia), and a low platelet count (thrombocytopenia).
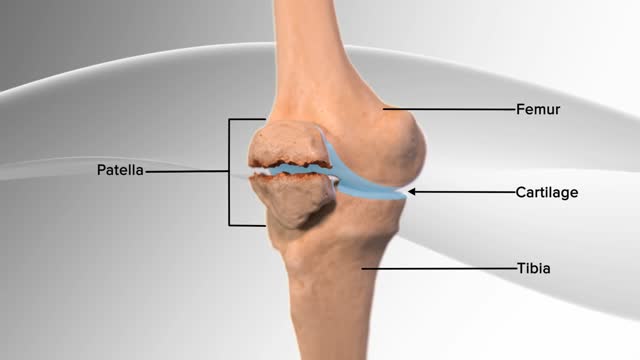
In this knee procedure, the patella is being repaired. The patella is a small, floating bone that glides over the thighbone. It connects the muscles of the thigh to the shinbone, helping the knee to move. The egg‐shell type covering on the underside of the patella and front of the femur allows for smooth motion of the knee.
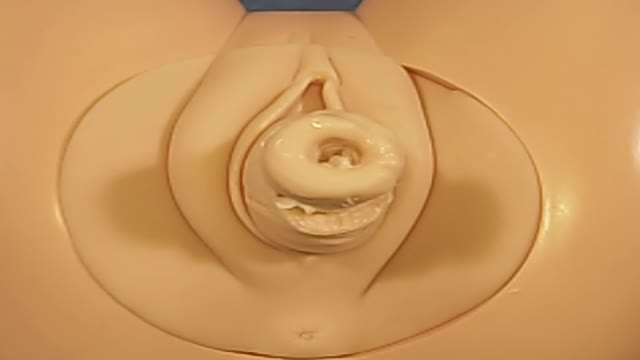
Cerclage is indicated in a patient with a history of painless cervical dilation and a second trimester loss. It is also indicated in a patient with a history of preterm birth and a short cervix found on ultrasound between 16-24 weeks gestation. Cerclage placement occurs after the first trimester in case the pregnancy is genetically abnormal and would likely result in a first trimester loss.

-Traumatic amputation of a body part requires rapid transport of the appendage, which should be wrapped in a saline-moistened gauze, placed in a plastic bag, and transported in a container filled with ice mixed with either saline or sterile water to best preserve the body part and attempt replantation.
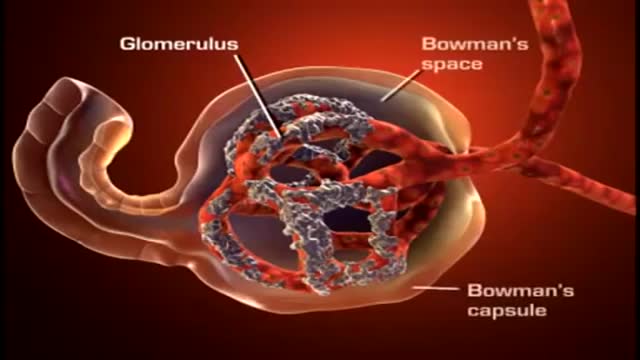
A nephron (from Greek νεφρός (nephros) meaning "kidney") is the basic structural and functional unit of the kidney. Its chief function is to regulate the concentration of water and soluble substances like sodium salts by filtering the blood, reabsorbing what is needed and excreting the rest as urine.
Eyelid surgery, or blepharoplasty, is a surgical procedure to improve the appearance of the eyelids. Surgery can be performed on either the upper and lower lids, or both. Whether you want to improve your appearance or are experiencing functional problems with your eyelids, eyelid surgery can rejuvenate the area surrounding your eyes.