Top videos
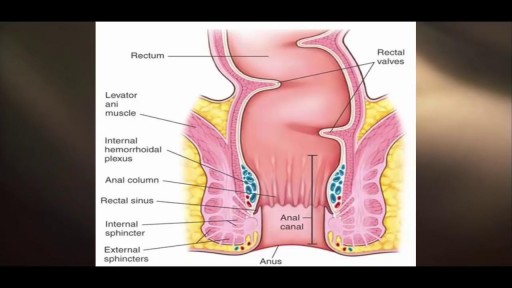
Rectal bleeding can refer to any blood that passes from your anus, although rectal bleeding is usually assumed to refer to bleeding from your lower colon or rectum. Your rectum makes up the last few inches of your large intestine. Rectal bleeding may show up as blood in your stool, on the toilet paper or in the toilet bowl. Blood that results from rectal bleeding can range in color from bright red to dark maroon to a dark, tarry color.
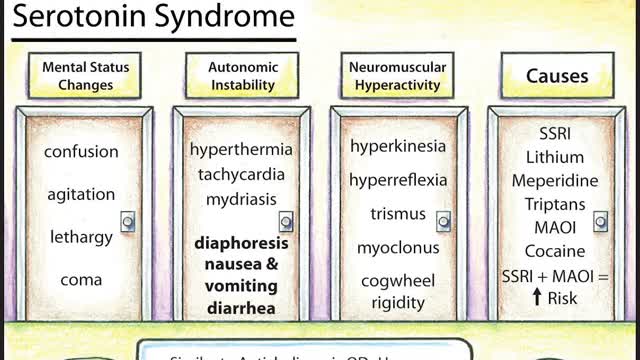
Symptoms of serotonin syndrome include a classic triad of mental status changes (eg, anxiety, delirium, confusion, restlessness), autonomic dysregulation (eg, diaphoresis, tachycardia, hypertension, hyperthermia, diarrhea, mydriasis), and neuromuscular hyperactivity (eg, hyperreflexia, tremor, rigidity, myoclonus, ocular clonus). Serotonin syndrome is clinically diagnosed and laboratory tests are used to rule out other etiologies. It usually occurs due to inadvertent interactions between drugs, therapeutic use of multiple serotonergic agents, or serotonergic medication overdose. Treatment involves discontinuation of serotonergic drugs, supportive measures, and sedation with benzodiazepines. In severe cases, a serotonin antagonist (cyproheptadine) may be used.

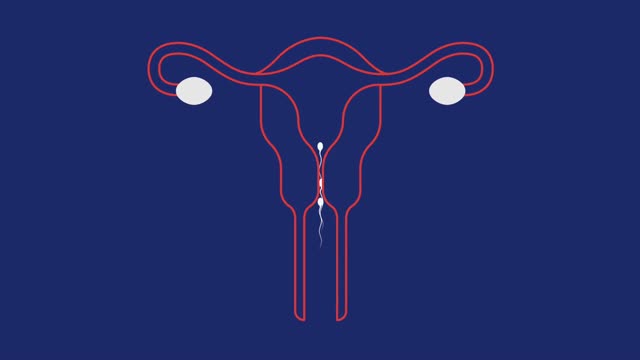
The fuel for the process leading to orgasm is testosterone, a hormone produced in steady supply by the testicles. The testicles also make millions of sperm each day, which mature and then are mixed with whitish, protein-rich fluids. These fluids nourish and support the sperm so they can live after ejaculation for a limited time. This mixture of fluid and sperm, known as semen, is what is moved through the urethra and out the penis during orgasm.
Pharyngitis is caused by swelling in the back of the throat (pharynx) between the tonsils and the voice box (larynx). Most sore throats are caused by colds, the flu, coxsackie virus or mono (mononucleosis). Bacteria that can cause pharyngitis in some cases: Strep throat is caused by group A streptococcus.

With ECT, electrodes are placed on the patient's scalp and a finely controlled electric current is applied while the patient is under general anesthesia. The current causes a brief seizure in the brain. ECT is one of the fastest ways to relieve symptoms in severely depressed or suicidal patients.

Body Restorations will do an “Early Assessment” when you come in for physiotherapy; this allows therapists to identify the more complicated cases quickly and get started with treatment right away. If you are feeling pain now, it is best that you seek treatment as soon as possible. Research has proven that people who seek treatment for their pain immediately have less of a chance of it becoming an issue later own. Early intervention is always the best option. Visit - https://stalbertphysiotherapy.com/contact/

Multiple sclerosis causes many different symptoms, including vision loss, pain, fatigue, and impaired coordination. The symptoms, severity, and duration can vary from person to person. Some people may be symptom free most of their lives, while others can have severe chronic symptoms that never go away. Physical therapy and medications that suppress the immune system can help with symptoms and slow disease progression.