Top videos

The journey of egg and sperm. There are a lot of casualties (deaths) among the sperm as they swim toward the egg. First, many get lost in the maze of a woman's uterus where they also have to contend with acidic vaginal secretions.
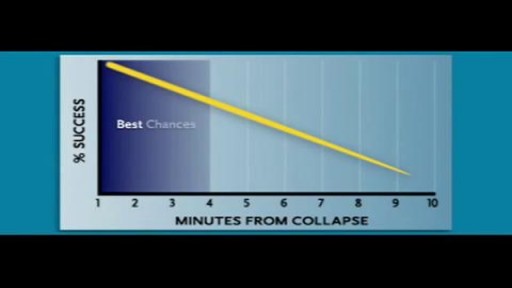
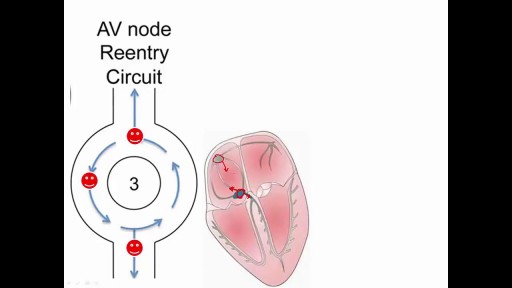
Cardiac arrest usually results from an electrical disturbance in the heart. It's not the same as a heart attack. The main symptom is loss of consciousness and unresponsiveness. This medical emergency needs immediate CPR or use of a defibrillator. Hospital care includes drugs, an implantable device, or other procedures.
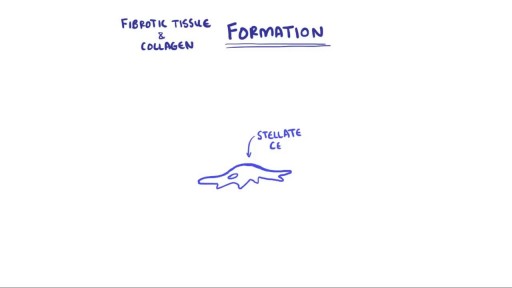
Hepatitis and chronic alcohol abuse are frequent causes. Liver damage caused by cirrhosis can't be undone, but further damage can be limited. Initially patients may experience fatigue, weakness, and weight loss. During later stages, patients may develop jaundice (yellowing of the skin), gastrointestinal bleeding, abdominal swelling, and confusion. Treatments focus on the underlying cause. In advanced cases, a liver transplant may be needed.
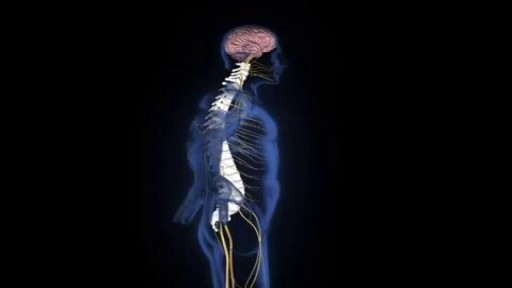
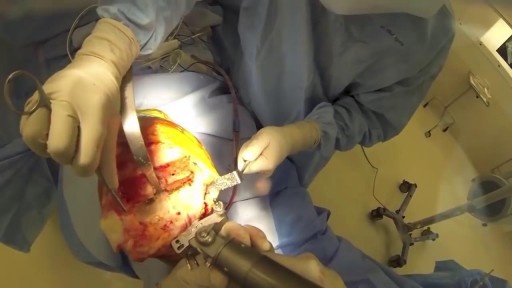
An estimated 12,500 spinal cord injuries occur in the U.S. every year, leaving the injured people, their friends, and their family, to cope with the aftermath of the catastrophe. For many, navigating the challenges of the health care system can feel a bit like going to medical school. Suddenly you're learning a veritable cornucopia of new terms, and may be spending endless hours Googling spinal cord anatomy to fill in the gaps in your knowledge. An educated patient is better equipped to advocate for his or her needs and interests. An education in spinal cord anatomy helps you understand what your doctor is saying, ask intelligent questions, and detect medical errors before they endanger your health.

Eating a high-protein breakfast has been shown to reduce cravings and calorie intake throughout the day (16, 17). Avoid sugary drinks and fruit juice. These are the most fattening things you can put into your body, and avoiding them can help you lose weight (18, 19). Drink water a half hour before meals.
Water is an essential nutrient for the body, as the body loses water through perspiration, breathing, bowel movements, and in urine. Water must be consumed regularly to maintain a sufficient level. Water has many vital functions in the body, including… Serving as a lubricant. Water is a main component of saliva, which helps moisten food making it easier to swallow. Water also helps lubricate joints, reducing friction and inflammation. Water is important in body temperature regulation. When body heat rises, such as during strenuous activities, the body starts to sweat to cool itself. And sweat is made up almost entirely of water.

Tinnitus (TIN-ih-tus) is the perception of noise or ringing in the ears. A common problem, tinnitus affects about 1 in 5 people. Tinnitus isn't a condition itself — it's a symptom of an underlying condition, such as age-related hearing loss, ear injury or a circulatory system disorder

For more information please visit: https://www.yalemedicine.org/c....onditions/acl-injury
Serious injuries, by and large, cause a lot of swelling in the knee. Especially in younger patients. Now, someone could be arthritic and they overdo it going for a big long hike and they get some swelling the next day. But rapid onset of swelling, it's like hard to make out where your kneecap is, is a pretty big cardinal sign that there's something serious that's happened to your knee. Rapid onset swelling is usually due to blood in the joint. "A meniscus that really tears and flips in the front. You tear your quad or your patellar tendon, your kneecap dislocates, you tear a little blood vessel, your ACL tears, a piece of cartilage in bone gets knocked off and causes bleeding. So a lot of the really significant injuries, people get rapid onset swelling within three to four hours and they should seek attention There's always exceptions to rules, but if your knee looks like a grapefruit, you should go get it checked.