Top videos
Bronchiectasis is an abnormal dilation of the proximal and medium-sized bronchi (>2 mm in diameter) caused by weakening or destruction of the muscular and elastic components of the bronchial walls. Affected areas may show a variety of changes, including transmural inflammation, edema, scarring, and ulceration, among other findings. Distal lung parenchyma may also be damaged secondary to persistent microbial infection and frequent postobstructive pneumonia. Bronchiectasis can be congenital but is most often acquired.[9] Congenital bronchiectasis usually affects infants and children. These cases result from developmental arrest of the bronchial tree. Acquired forms occur in adults and older children and require an infectious insult, impairment of drainage, airway obstruction, and/or a defect in host defense. The tissue is also damaged in part by the host response of neutrophilic proteases, inflammatory cytokines, nitric oxide, and oxygen radicals. This results in damage to the muscular and elastic components of the bronchial wall. Additionally, peribronchial alveolar tissue may be damaged, resulting in diffuse peribronchial fibrosis.[12] The result is abnormal bronchial dilatation with bronchial wall destruction and transmural inflammation. The most important functional finding of altered airway anatomy is severely impaired clearance of secretions from the bronchial tree. Impaired clearance of secretions causes colonization and infection with pathogenic organisms, contributing to the purulent expectoration commonly observed in patients with bronchiectasis. The result is further bronchial damage and a vicious cycle of bronchial damage, bronchial dilation, impaired clearance of secretions, recurrent infection, and more bronchial damage
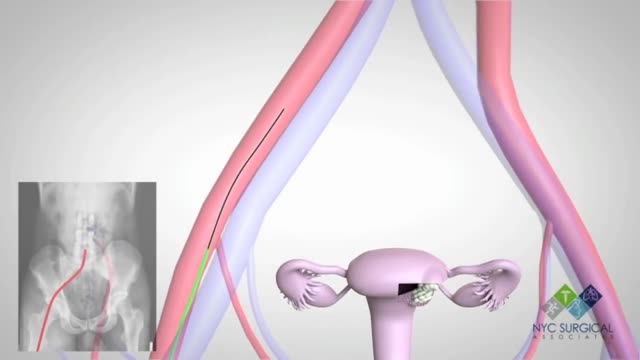
There's no single best approach to uterine fibroid treatment — many treatment options exist. If you have symptoms, talk with your doctor about options for symptom relief. Watchful waiting Many women with uterine fibroids experience no signs or symptoms, or only mildly annoying signs and symptoms that they can live with. If that's the case for you, watchful waiting could be the best option. Fibroids aren't cancerous. They rarely interfere with pregnancy. They usually grow slowly — or not at all — and tend to shrink after menopause, when levels of reproductive hormones drop. Medications Medications for uterine fibroids target hormones that regulate your menstrual cycle, treating symptoms such as heavy menstrual bleeding and pelvic pressure. They don't eliminate fibroids, but may shrink them. Medications include: Gonadotropin-releasing hormone (Gn-RH) agonists. Medications called Gn-RH agonists (Lupron, Synarel, others) treat fibroids by blocking the production of estrogen and progesterone, putting you into a temporary postmenopausal state. As a result, menstruation stops, fibroids shrink and anemia often improves. Your doctor may prescribe a Gn-RH agonist to shrink the size of your fibroids before a planned surgery. Many women have significant hot flashes while using Gn-RH agonists. Gn-RH agonists typically are used for no more than three to six months because symptoms return when the medication is stopped and long-term use can cause loss of bone. Progestin-releasing intrauterine device (IUD). A progestin-releasing IUD can relieve heavy bleeding caused by fibroids. A progestin-releasing IUD provides symptom relief only and doesn't shrink fibroids or make them disappear. It also prevents pregnancy. Tranexamic acid (Lysteda). This nonhormonal medication is taken to ease heavy menstrual periods. It's taken only on heavy bleeding days. Other medications. Your doctor might recommend other medications. For example, oral contraceptives or progestins can help control menstrual bleeding, but they don't reduce fibroid size. Nonsteroidal anti-inflammatory drugs (NSAIDs), which are not hormonal medications, may be effective in relieving pain related to fibroids, but they don't reduce bleeding caused by fibroids. Your doctor may also suggest that you take vitamins and iron if you have heavy menstrual bleeding and anemia
This video is available for instant download licensing here: https://www.alilamedicalmedia.....com/-/galleries/all-
©Alila Medical Media. All rights reserved.
Support us on Patreon and get FREE downloads and other great rewards: patreon.com/AlilaMedicalMedia
All images/videos by Alila Medical Media are for information purposes ONLY and are NOT intended to replace professional medical advice, diagnosis or treatment. Always seek the advice of a qualified healthcare provider with any questions you may have regarding a medical condition.
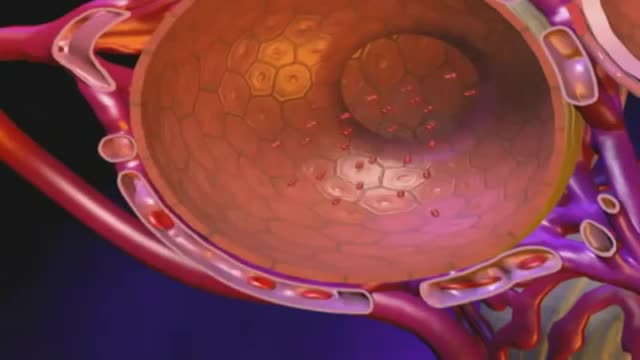
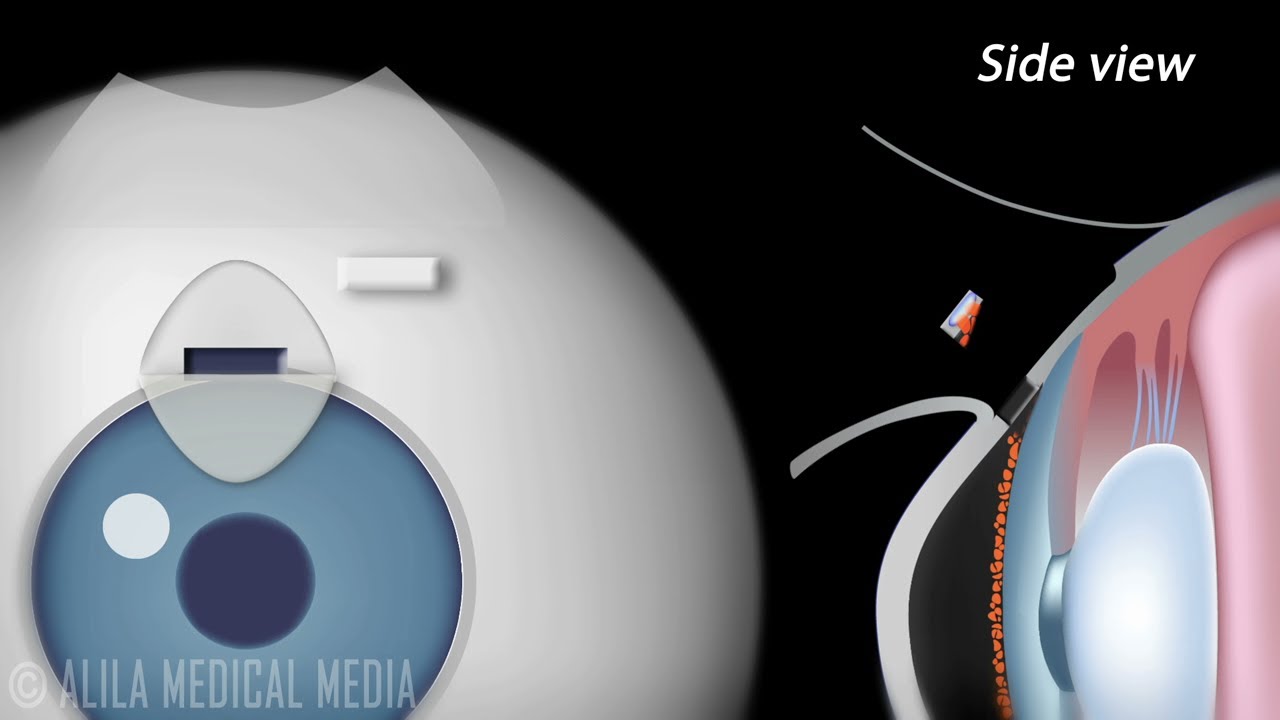
Trabeculectomy, also called Filtration Surgery, is a surgical procedure performed for treatment of glaucoma. The treatment involves removing part of the trabecular meshwork and creating a new escape route for the aqueous humor. When successful, it allows the aqueous fluid to drain from the eye into an area underneath the conjunctiva where it is subsequently absorbed by the body's circulatory system or filtered into tears.
In this procedure:
- A conjunctival pocket is created and maybe treated with Mitomycin or other antimetabolites for a few minutes. These drugs are used to prevent scarring of the operation site. Scarring, if occurs, may clog the new drainage canal, and is therefore the major reason the procedure may fail.
- A half thickness flap is then made in the sclera and is dissected all the way to the clear cornea.
- A block of scleral tissue including part of the trabecular meshwork and Schlemm's canal is then removed to make a hole into the anterior chamber of the eye.
- As the iris may plug up this hole from the inside, a piece of the iris maybe removed at this time. This is called iridectomy.
- The scleral flap is then sutured loosely back in place. These sutures can be released gradually during a couple of weeks after surgery. This allows adjustment of the aqueous flow in order to achieve target pressure and to avoid the complication of having a too low intraocular pressure.
- The conjunctiva is sewn back in place to cover the area.
After surgery, aqueous humor drains into a filtering area called a "bleb" under the conjunctiva. Since the surgery is usually performed near the top of the eye, the bleb can easily be concealed behind the upper eyelid.
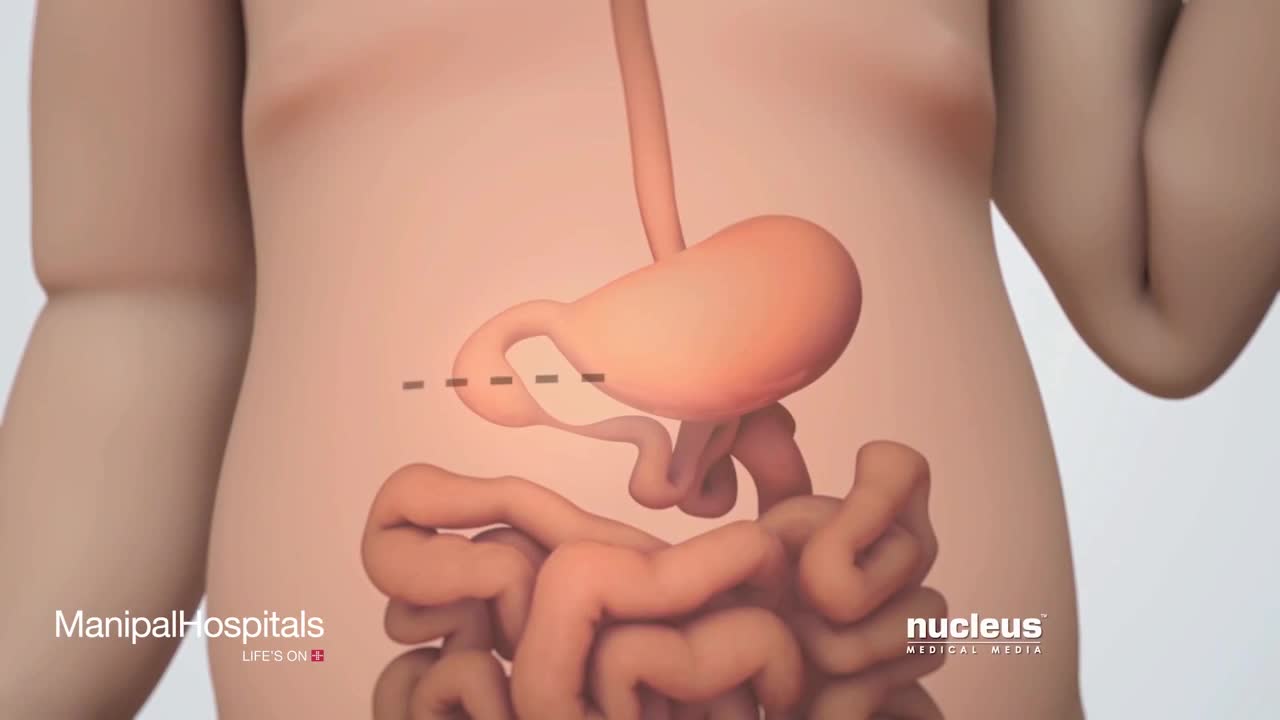
Duodenal atresia, also known as duodenojejunal atresia, is the congenital absence or complete closure of a portion of the lumen of the duodenum. It causes increased levels of amniotic fluid during pregnancy (polyhydramnios) and intestinal obstruction in newborn babies.

http://www.nucleushealth.com/ - This 3D medical animation shows the cause and laparoscopic treatment of a ventral incisional hernia. If you have had abdominal surgery in the past, a ventral incisional hernia may appear at the site of your surgical scar. Your intestine may push through a weakened spot in the tissue between your abdominal muscles creating a bulge beneath your skin. If your hernia is not repaired, complications may occur.
#VentralHernia #VentralIncisionalHernia #IncisionalHernia
ANH11053

The thyroid gland lies in the midline of the anterior neck, just caudal to the thyroid cartilage. To inspect the thyroid gland, the examiner stands in front of the patient. The examiner asks the seated patient to dorsiflex (extend) the neck and swallow a sip of water. Minor enlargement of the gland may only become apparent on inspection in this position. Palpation of the thyroid gland is typically performed with the examiner standing behind the patient. Both lobes and the isthmus of the thyroid gland should be palpated for any nodules or diffuse enlargement. Mobility of the thyroid gland with swallowing should be assessed with palpation. Nodules arising from the thyroid gland typically move with swallowing. A hard, fixed thyroid gland could indicate malignancy. If a central nodule is identified, the patient is asked to protrude the tongue. Upward movement of the central nodule on protrusion of the tongue indicates a thyroglossal cyst. Auscultation is performed at the superior poles of bilateral lobes as this is where the superior thyroid artery is most superficial and bifurcates into its terminal branches. A bilateral bruit over the superior poles suggests Graves disease. Examination of the thyroid gland is completed by palpating the regional cervical lymph nodes for any enlargement.
Subscribe to AMBOSS YouTube for the latest clinical examination videos, medical student interviews, study tips and tricks, and live webinars!
Free 5 Day Trial: https://go.amboss.com/amboss-YT
Instagram: https://www.instagram.com/amboss_med/
Facebook: https://www.facebook.com/AMBOSS.Med/
Twitter: https://twitter.com/ambossmed
Blog: https://blog.amboss.com/us
#AMBOSSMed #ClinicalExamination #USMLE

Gallbladder cancer is cancer that begins in the gallbladder. Your gallbladder is a small, pear-shaped organ on the right side of your abdomen, just beneath your liver. The gallbladder stores bile, a digestive fluid produced by your liver. Gallbladder cancer is uncommon. When gallbladder cancer is discovered at its earliest stages, the chance for a cure is very good. But most gallbladder cancers are discovered at a late stage, when the prognosis is often very poor. Gallbladder cancer is difficult to diagnose because it often causes no specific signs or symptoms. Also, the relatively hidden nature of the gallbladder makes it easier for gallbladder cancer to grow without being detected. Symptoms ShareTweet Aug. 07, 2014 References Products and Services Book: Mayo Clinic on Digestive Health Give today to find cancer cures for tomorrow See also Abdominal pain Can you recommend a diet after gallbladder removal? Chemo Targets Chemotherapy Chemotherapy and hair loss: What to expect during treatment Chemotherapy and sex: Is sexual activity OK during treatment? Chemotherapy nausea and vomiting: Prevention is best defense Show more Advertisement Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission. Advertising & Sponsorship PolicyOpportunitiesAd Choices Mayo Clinic Store Check out these best-sellers and special offers on books and newsletters from Mayo Clinic. NEW! – The Mayo Clinic Diet, Second Edition Relief for America's epidemic of indigestion Keeping your bones healthy and strong Manage blood pressure for better health The Mayo Clinic Diet Online
All Solution of Male Disorder Male Infertility Diagnostic and Treatment Re-Slim Care Latest Technology in Pakistan Dr. Aslam Naveed is a well known sexologist in Pakistan. He has treated more than 1 Lac patients since last 30 years of clinical Practice in sexology, he knows how to help the people facing sexual disorders. Contact: 02134965050, 03432821919, 0345-8314663 http://www.sexologistpakistan.com/ https://www.facebook.com/menssexcareclinic/ https://www.youtube.com/channel/UCagSSgdEgQJWl_xfFM12BwA https://twitter.com/bettersexcare https://www.instagram.com/dr.aslamnaveed/ ADDRESS: Men’s Care Modern Hospital, Opposite, Safari Park, University Road, Karachi, Pakistan.

Brachytherapy or localized radiation treatment can be used in certain patients with breast cancer. Depending on tumor size and other factor, physicians may use APBI or accelerated partial breast irradiation. Dr. Elizabeth Tapen, a radiation oncologist, reviews brachytherapy for breast cancer.
Angioplasty is a procedure to restore blood flow through the artery. You have angioplasty in a hospital. The doctor threads a thin tube through a blood vessel in the arm or groin up to the involved site in the artery. The tube has a tiny balloon on the end.