Top videos

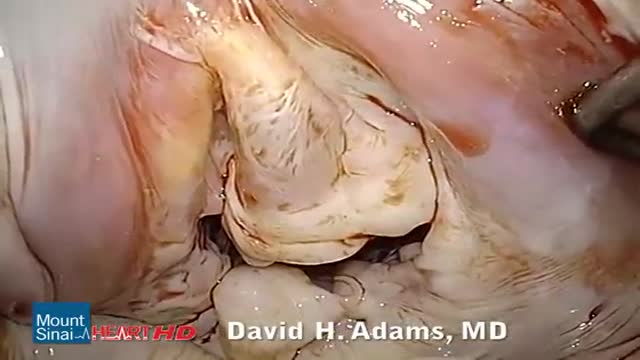
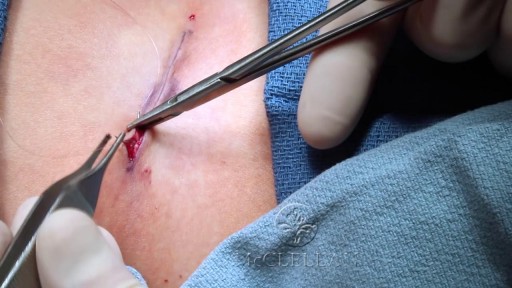
Microsurgical bipolar cautery tonsillectomy compares favorably with traditional techniques in terms of intraoperative bleeding, postoperative pain, otalgia, and hemorrhage. This technique combines the hemostatic advantage of cautery dissection, the excellent visualization achieved by a microscope, and, with the use of a video, greatly improves the physician's ability to teach how to perform a tonsillectomy.

Hemodialysis is the process of cleaning the patient’s blood outside the body. Learn more about this renal replacement therapy option.
Read more: http://www.freseniusmedicalcar....e.com/en/patients-fa
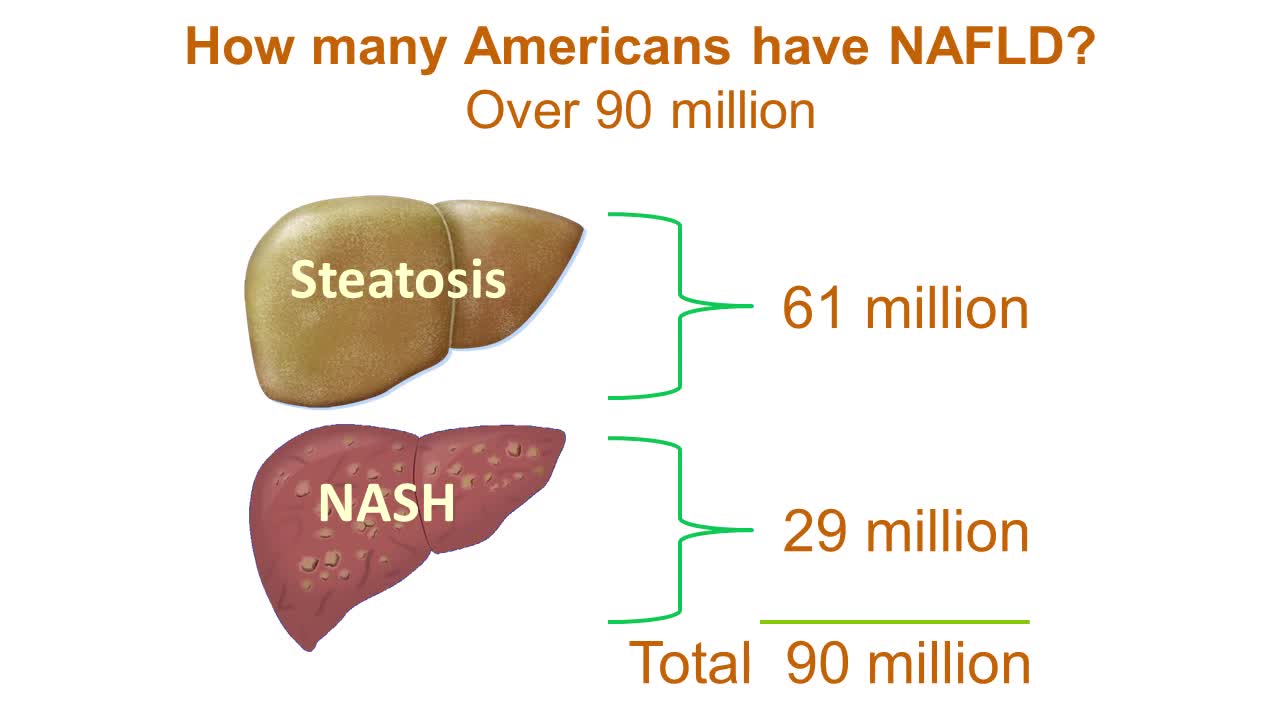
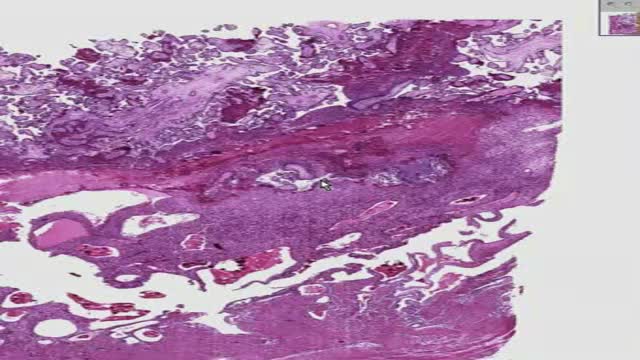
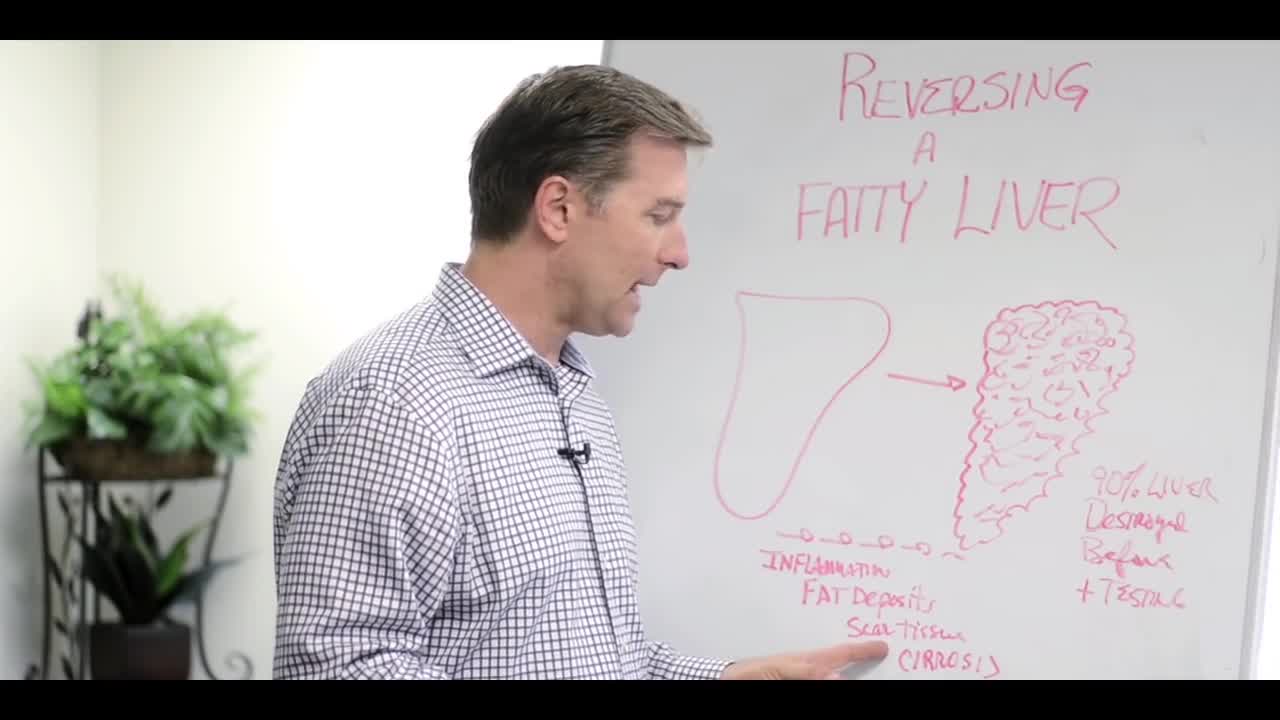
Nonalcoholic fatty liver disease is an umbrella term for a range of liver conditions affecting people who drink little to no alcohol. As the name implies, the main characteristic of nonalcoholic fatty liver disease is too much fat stored in liver cells. Nonalcoholic steatohepatitis, a potentially serious form of the disease, is marked by liver inflammation, which may progress to scarring and irreversible damage. This damage is similar to the damage caused by heavy alcohol use. At its most severe, nonalcoholic steatohepatitis can progress to cirrhosis and liver failure Nonalcoholic fatty liver disease is increasingly common around the world, especially in Western nations. In the United States, it is the most common form of chronic liver disease, affecting an estimated 80 to 100 million people. Nonalcoholic fatty liver disease occurs in every age group but especially in people in their 40s and 50s who are at high risk of heart disease because of such risk factors as obesity and type 2 diabetes. The condition is also closely linked to metabolic syndrome, which is a cluster of abnormalities including increased abdominal fat, poor ability to use the hormone insulin, high blood pressure and high blood levels of triglycerides, a type of fat. Nonalcoholic fatty liver disease care at Mayo Clinic Request an Appointment at Mayo Clinic Symptoms & causes Aug. 23, 2016 Print Share on: Facebook Twitter References Related Magnetic resonance elastography Nonalcoholic fatty liver disease Overview Symptoms & causes Diagnosis & treatment Diagnosis Treatment Departments & specialties Expertise & rankings Locations, travel & lodging Clinical trials Research Costs & insurance Preparing for your appointment Self-management More about In-Depth Multimedia Resources News from Mayo Clinic Advertisement

Cathy covers hemodialysis, including nursing care before, during, and after the procedure. Peritoneal dialysis, including nursing associated with the procedure. Key complications of hemodialysis, including disequilibrium syndrome and hypotension. Peritonitis, which is a key complication of peritoneal dialysis. Post-op nursing care and patient teaching associated with a kidney transplant.
Our Medical-Surgical video tutorial series is taught by Cathy Parkes BSN, RN, CWCN, PHN and intended to help RN and PN nursing students study for their nursing school exams, including the ATI, HESI and NCLEX.
#NCLEX #KidneyTransplant #HESI #Kaplan #ATI #NursingSchool #NursingStudent #Nurse #RN #PN #Education #LVN #LPN #Renal #Hemodialysis
0:00 What to Expect
0:31 Hemodialysis
2:06 Nursing Care
2:47 Peritoneal Dialysis
3:23 Nursing Care
4:09 Dialysis Complications
4:19 Disequilibrium Syndrome
4:55 Hypotension
5:26 Peritonitis
5:57 Kidney Transplant
6:17 Nursing Care
6:40 Signs and Symptoms
6:51 Patient Teaching
7:17 Quiz Time!
8:27 Bloopers
🚨Head over to our interactive study guide and index ANYTIME and find out exactly which card we’re referencing. https://bit.ly/MedSurgIndex
🚨 Reminder: shipping deadlines are looming 👀
🎁 Regular Shipping: Order by Friday, December 15
🚀 Expedited Shipping: Order by Monday, December 18
🔍 Still searching for last-minute gifts? Consider a Level Up RN Gift Card! 💌 It’s not only a thoughtful present but also the perfect way to share treasures like Pharmacology Flashcards OR digital treasures like Flashables Digital Nursing Flashcards & the Level Up RN membership. Give the gift of knowledge this holiday season! 🧠⚡️💖 bit.ly/LevelUpRNGC
🚪 Access our Cram Courses, Quizzes and Videos all in one ad free space with Level Up RN Membership https://bit.ly/LevelUpRNMembership
Want more ways to MASTER Medical-Surgical Nursing? Check out our flashcards, review games, videos, tips & more!
👇👇👇👇👇👇👇👇👇👇
👉 https://bit.ly/AllMedSurg 👈
☝️👆☝️👆☝️👆☝️👆☝️👆
This is your one-stop-shop for materials to help you LEARN & REVIEW so you can PASS Nursing School.
🤔🤔🤔 DO YOU WANT TO PASS your classes, proctored exams and the NCLEX? 🤔🤔🤔 Our resources are the best you can buy. They are built with a single goal: help you pass with no fluff. Everything you need, and nothing you don’t. Don’t take our word for it, though! Check out our hundreds of ⭐️⭐️⭐️⭐️⭐️ reviews from nurses who passed their exams and the NCLEX with Level Up RN.
🗂️ Our Ultimate Nursing School Survival kit is your number 1 resource to get through nursing school and to pass the NCLEX. Whether you're just starting school or you’re already prepping for the NCLEX, this bundle of flashcards is the best you can buy. It covers all the information you need to know to pass all your exams and it has FREE shipping!
➡️ https://bit.ly/TUNSSK ⬅️
L👀king for EVEN MORE resources to survive Nursing School? Make your Nursing School experience your own! Life’s difficult enough—learning shouldn’t be.
🪅 Games https://nursesquad.com
💻 Digital resources https://bit.ly/NursingStudyCourses
📅 Organizational tools https://bit.ly/OrganizingSchool
✨Want perks? Join our channel!
https://youtube.com/leveluprn/join
🏷 Head to https://leveluprn.com/specials for all our latest deals!🥳️
📧 LOOKING FOR FREE RESOURCES TO HELP WITH YOUR EXAMS? Get exclusive tips, latest video releases and more delivered to your email!
➡️ https://leveluprn.com/signup ⬅️
⚕ 👩 LEVEL UP NURSE SQUAD 👩⚕️
All of the nurses at Level Up RN are here to help! Cathy Parkes started helping her fellow classmates back when she was in nursing school, tutoring so they could pass their exams and graduate. After she got her BSN and started working as an RN at Scripps Encinitas Hospital, she started this YouTube channel to help nursing students around the world. Since then she has built a team of top-notch dedicated nurses and nurse educators who are focused on improving nursing education and supporting career advancement for nurses everywhere. With flashcards, videos, courses, organizational tools and more, we are singularly focused on helping students and nurses Level Up on their exams and nursing careers.
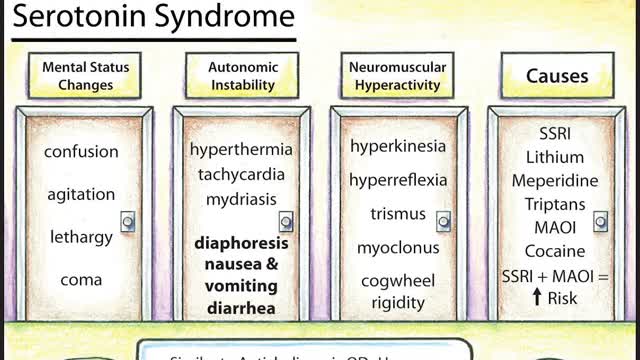
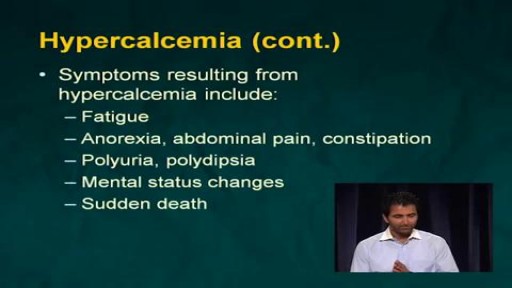
Symptoms of serotonin syndrome include a classic triad of mental status changes (eg, anxiety, delirium, confusion, restlessness), autonomic dysregulation (eg, diaphoresis, tachycardia, hypertension, hyperthermia, diarrhea, mydriasis), and neuromuscular hyperactivity (eg, hyperreflexia, tremor, rigidity, myoclonus, ocular clonus). Serotonin syndrome is clinically diagnosed and laboratory tests are used to rule out other etiologies. It usually occurs due to inadvertent interactions between drugs, therapeutic use of multiple serotonergic agents, or serotonergic medication overdose. Treatment involves discontinuation of serotonergic drugs, supportive measures, and sedation with benzodiazepines. In severe cases, a serotonin antagonist (cyproheptadine) may be used.
A cervical biopsy is a procedure that is sometimes done on women during an exam called a colposcopy to remove cervical tissue for examination. It is also called a punch biopsy. It is usually performed when a Pap smear result is either inconclusive or abnormal and a doctor wants to screen further for any cervical dysplasia or cervical cancer.
Symptoms of liver failure include vomiting, diarrhea and fatigue as well as the symptoms from stage 3. While the progression from cirrhosis to failure can take years, the damage is irreversible and leads to eventual death. The key to treating liver disease is to diagnose the condition as early as possible.