Top videos
Dialysis lecture 1. Dialysis Study: EXPERT NOTES for DHA, Bonent, CHT, B.Sc in Dialysis, Diploma in Dialysis https://amzn.eu/d/35Ui1kT
2. Dialysis Study : Q & A: MCQs, Fill in the blanks, True or False https://amzn.eu/d/gGn8u73
1. Dialysis Study :EXPERT NOTES for DHA, Bonent, CHT, B.Sc in Dialysis, Diploma in Dialysis, Naseha Helal.
https://play.google.com/store/....books/details?id=D_7
2. Dialysis Study: Q & A MCQ https://play.google.com/store/....books/details?id=T_3
Whatsapp
https://chat.whatsapp.com/DKCHbgsNwXS1wd7xI31tpr
Telegram
https://t.me/dialysislife PRINCIPLE OF dialysis
https://youtu.be/cfOm0aFmbe8
Dialysis machine alarms
https://youtu.be/-1A1INyDEOg
DDS dialysis disequilibrium syndrome
https://youtu.be/8AqVFiBOkIc
Peritoneal Dialysis
https://youtu.be/iHPPadGmsv0
Itching
https://youtu.be/T83Wm3HHU4M
What is CRRT
https://youtu.be/jPgFnoSEBMU
LVH
https://youtu.be/ZhFL3Z6LHeA
Sorbent dialysis
https://youtu.be/-rie5dC_FkY
RO Water
https://youtu.be/3jlEsK4Lg_I
Carbon filter RO water
https://youtu.be/mJrgtjNafQw
Hemoperfusion
https://youtu.be/UkbBm8rm9Ww
AV fistula or Dialysis fistula
https://youtu.be/uDbyfqCkCbo
Dialysis MCQ
https://youtu.be/zmOj0BL6jVY
AVF cannulation
https://youtu.be/PyqMcHA07zY
Complications of AV fistula
https://youtu.be/a_CXIvuOO_s
Blood clotting during Dialysis
https://youtu.be/9hYNepiO2o8
Muscle crapms
https://youtu.be/09s07Eiqr2k
Hepatitis C
https://youtu.be/qdNj_GhmnSE
Dialysis procedure
https://youtu.be/u1mGqXO5pzQ
Hypotension
https://youtu.be/4EVPmWTSyN8
Heparin free dialysis
https://youtu.be/rFqAn7HcWwM
Plasmapheresis
https://youtu.be/kbgsjjs9krg
Isolated ultrafiltration
https://youtu.be/xp5I5--uWb0
High flux dialyzer
https://youtu.be/gCNsErn1HHM
Urea and Creatinine
https://youtu.be/Id9AIySMQ6c
Practical RO water demo
https://youtu.be/2pXKGMDNS84
Sodium profiling
https://youtu.be/bE_DcBXNB5g
Peritoneal Dialysis
https://youtu.be/vtK6VZsi8AY
Air embolism
https://youtu.be/WJE-xqnQfd8
Dialysate
https://youtu.be/z_nb43bcWsM
How to stop Bleed from fistula
https://youtu.be/N_inLKPhPUc
Dialysis short form
https://youtu.be/3BqB-gODb5o
Dialyzer reprocessing
https://youtu.be/XelfkKsndlc
Dialysis catheter
https://youtu.be/V7y90m4xlv8
How to set KT/V
https://youtu.be/hWXjU8VTQdk
Mircera injection
https://youtu.be/STtd3I3EijA
Dialysis procedure
https://youtu.be/MIdhIgcKRZ8
Dialysis in snake bite poison
https://youtu.be/niA9RI38jyY
Uf profiling
https://youtu.be/wyjpFjD5Hi0
Heparin dose
https://youtu.be/kB56MkzHIQ0
Hyperkalemia
https://youtu.be/1rWWNlcAuio
Change bandages of leaking fistula
https://youtu.be/_0cebWWdjM8
AvF needle
https://youtu.be/GvUxbXxftTk
Polycystic kidney disease
https://youtu.be/IhsMbHFXZG8
Nephrotic syndrome
https://youtu.be/FEEOsIrXxV8
Diabetic nephropathy
https://youtu.be/v-FBIQ7MA4k
Hemodialysis permanent access
https://youtu.be/_YrwxwiR0f8
Sex and dialysis
https://youtu.be/vvl8UT8lK4k
Albumin and dialysis
https://youtu.be/yzG7yD45Nwg
Does Knee Replacement Surgery Meet Patient Expectations? In this video, I discuss knee replacement surgery or total knee arthroplasty expectations. A recent study reported that 1 in 4 patients who underwent knee replacement did not have their expectations met. The video reviews the differences in outcomes and satisfaction levels between satisfied and unsatisfied patients and identifies the key expectations that must be met for patients to be satisfied after knee replacement.
https://pubmed.ncbi.nlm.nih.gov/36740633/
► Things my patients have found helpful:
Please note that I get a lot of requests and questions about what equipment is ‘best’ for treating a variety of conditions. The following is not meant to be an exhaustive or definitive list. Please use it as a starting point. If you have questions, please discuss with your healthcare provider. With that said, I have tried a number of the products below, but not all. I have included some based on positive feedback from many of my patients. As an Amazon Associate, Dr Peng earns from qualifying purchases. If you purchase any product using the below affiliate links, you are helping Dr Peng maintain this channel.
*Soft Tissue & Rehab*
Theragun: https://amzn.to/4363zJG
Massage ball: https://amzn.to/40BUC9f
Foam roller: https://amzn.to/4324E5c
Stretching strap: https://amzn.to/3U9a2iQ
TENS unit: https://amzn.to/3mcCqnI
Heating pad: https://amzn.to/40VidSc
Resistance bands: https://amzn.to/3nFyb4C
*Braces & Supports*
Hinged knee brace: https://amzn.to/3U6oyrH
Neoprene knee sleeve: https://amzn.to/3Zzhsgt
Volar wrist brace: https://amzn.to/3KawW55
Thumb spica brace: https://amzn.to/3nHj9vl
Ankle lace up brace: https://amzn.to/3m6iR0u
Tennis/Golfer’s elbow brace: https://amzn.to/3ZEGgE1
Superfeet orthotic inserts: https://amzn.to/436tRf5
*Recommended Textbooks & Resources*
The Trigger Point Manual: https://amzn.to/4340cTt
Trigger Point Wall Charts: https://amzn.to/3zrinVR
► Be Active. Live Healthy. Subscribe for more free videos like this: https://www.youtube.com/channe....l/UCL5eiGK1f0A-DecaB
► ABOUT ME
Jeffrey Peng MD is a nonoperative orthopedist and sports medicine specialist. He created a YouTube channel and blog to translate cutting edge medical knowledge and clinical research to benefit all those looking to live an active and healthy lifestyle. He focuses on maximizing non-surgical treatments for sports injuries and orthopedic conditions. He specializes in using orthobiologics and ultrasound guided minimally invasive techniques to treat osteoarthritis, tendinopathies, and musculoskeletal disorders.
Dr. Peng is board certified in sports medicine and family medicine. He completed residency with the Stanford family medicine residency program and completed his sports medicine training with the Stanford primary care sports medicine fellowship in San Jose. He is an active faculty member for both programs and is excited about training the next generation of physicians.
Dr. Peng’s sports medicine clinic is located in Campbell, California.
Twitter: @JeffreyPengMD; https://twitter.com/JeffreyPengMD
Website: https://www.jeffreypengmd.com/
► Disclaimer
My content reflects my own opinion and does not represent the views or opinions of my employers or hospital systems I am affiliated with. They are meant for educational purposes only. They do not substitute for the medical advice of a physician. Always seek the advice of your physician with any questions you may have regarding your health.
Train with some of the region’s very best pediatric general surgeons — in a two-year, pediatric surgical fellowship training program at Nemours/Alfred I. duPont Hospital for Children. Our hospital’s Division of Pediatric Surgery is offering this program in affiliation with Sidney Kimmel Medical College at Thomas Jefferson University .
The goal of the fellowship is to give individuals who have completed an accredited general surgery residency advanced knowledge and training in the management and surgical treatment of newborns, infants and children.
Our Fellowship Program
This fellowship will help you prepare for certification by the American Board of Surgery, and is accredited by the Accreditation Council for Graduate Medical Education (ACGME).
The Pediatric Surgery Fellowship aims to:
train a well-rounded, empathetic, safe pediatric surgeon who is confident managing all aspects of the surgical care of children.
steward our fellow in quality improvement projects and methodology, and provide research opportunities.
provide a rigorous didactic curriculum for our fellow utilizing 360 degree feedback.
cultivate opportunities for our fellow to educate residents and students.
encourage our fellow to collaborate across specialties.
develop our fellow’s presentation skills during M&M conferences and multi-disciplinary educational meetings.
The program features the full participation of all nine of the pediatric surgical division’s full-time faculty members. Each of these physicians will contribute greatly to your education. Your training will include operating room and outpatient clinic experience, as well as bedside evaluation of children. You’ll also play a role in the organization of formal teaching conferences, held weekly. Formal rotations will be spent on Pediatric Urology, PICU and Neonatology during the first 12 months. The last year will be spent entirely on the Pediatric Surgical Service.
The majority of your inpatient consultative time will take place at Nemours/Alfred I. duPont Hospital for Children, a freestanding children’s hospital in Wilmington, Del. The hospital:
is nationally ranked by U.S. News & World Report in eight pediatric specialties
recently opened expansion with 260 beds
performs more than 2,800 inpatient and 9,300 outpatient surgical procedures each year in our operating rooms
has an on-site delivery center for newborns with complex congenital anomalies
receives more than 50,000 annual visits in our Emergency Department (ED)
is accredited by The American College of Surgeons as a Level One Pediatric Trauma Center
is accredited by the Commission on Accreditation of Rehabilitation Facilities (CARF)
Visit https://www.nemours.org/educat....ion/gme/fellowships/ to learn more.
As a pediatric surgeon at NewYork-Presbyterian/Weill Cornell Medical Center, Dr. Nitsana Spigland treats newborns, children, teens, and young adults requiring surgical interventions. She specializes in antenatal counseling and newborn congenital malformations.
Learn more about Dr. Spigland at: https://www.nyp.org/physician/nspigland.
Histological features and cellular biology of exocrine glands. This video is a part of our Histology Video Course (https://youtube.com/playlist?l....ist=PLnr1l7WuQdDynxT
Additional YouTube Content
Biochemistry videos: https://youtube.com/playlist?l....ist=PLnr1l7WuQdDzCUC
Anatomy Videos: https://youtube.com/playlist?l....ist=PLnr1l7WuQdDz2dK
DaVinci Cases Videos: https://youtube.com/playlist?l....ist=PLnr1l7WuQdDyJUl
The DaVinci Hour Podcast: https://youtube.com/playlist?l....ist=PLnr1l7WuQdDwSm9
DaVinci Academy Website: https://www.dviacademy.com/
http://www.nucleushealth.com/ - This 3D medical animation depicts two operations, called craniotomy and craniectomy, in which the skull is opened to access the brain. The normal anatomy of the skull and tissues surrounding the brain are shown, including arteries and veins. The animation lists the common reasons for these procedures, and briefly introduces intracranial pressure.
Video ID: ANH13109
Transcript:
Your doctor may recommend a craniotomy or a craniectomy procedure to treat a number of different brain diseases, injuries, or conditions.
Your skull is made of bone and serves as a hard, protective covering for your brain. Just inside your skull, three layers of tissue, called meninges, surround your brain. The thick, outermost layer is the dura mater. The middle tissue layer is the arachnoid mater and the innermost layer is the pia mater. Between the arachnoid mater and the pia mater is the subarachnoid space, which contains blood vessels and a clear fluid called cerebrospinal fluid. Blood vessels, called bridging veins, connect the surface of your brain with the dura mater. Other blood vessels, called cerebral arteries, bring blood to your brain.
Inside your skull, normal brain function requires a delicate balance of pressure between the blood in your blood vessels, the cerebrospinal fluid that surrounds your brain, and your brain tissue. This is called normal intracranial pressure. Increased intracranial pressure may result from: brain tumors, head injuries, problems with your blood vessels, or infections in your brain or spinal cord. These conditions put pressure on your brain and may cause it to swell or change shape inside your skull, which can lead to serious brain injury.
Your doctor may recommend a craniotomy to remove: abnormal brain tissue, such as a brain tumor, a sample of tissue by biopsy, a blood clot, called a hematoma, excess cerebrospinal fluid, or pus from an infection, called an abscess.
A craniotomy may also be done to: relieve brain swelling,
stop bleeding, called a hemorrhage, repair abnormal blood vessels, repair skull fractures, or repair damaged meninges.
Finally, a craniotomy may also be done to: treat brain conditions, such as epilepsy, deliver medication to your brain, or implant a medical device, such as a deep brain stimulator.
The most common reason for a craniotomy is to remove a brain tumor.
#Craniotomy #Craniectomy #BrainSurgery
Ever considered getting laser eye surgery, but didn’t know how it worked? Allow us to help!
There are three different main types of laser eye surgery: LASIK, SMILE, and Surface Laser Treatments, and each can be explained pretty easily.
LASIK uses two lasers to open up a thin flap on the surface of the cornea, and then reshapes the cornea underneath. The flap is then placed back over the reshaped cornea, and heals independently with time.
SMILE uses one laser to reshape the cornea through a small, self-healing hole.
And Surface Eye Treatments remove the clear skin over the eye, to then reshape the cornea underneath with - you guessed it - a laser!
Each person's knee is different. This is why UC San Diego Health offers several surgical options for knee replacements to tailor care to each person's injury and health. Each surgical approach has benefits for the right surgical candidate. Our surgeons can discuss what option is most appropriate for each person.
To learn more about knee replacement options at UC San Diego Health, visit:
https://health.ucsd.edu/specia....lties/orthopedics/jo
Francis Gonzales, MD, is a board-certified orthopedic surgeon who specializes in adult hip and knee joint replacement surgery. Learn more about Dr. Gonzales: https://providers.ucsd.edu/det....ails/11935/orthopedi
UC San Diego Health is repeatedly ranked among the nation's best in orthopedic care by U.S. News & World Report. We are also a Blue Distinction Center recognized for our treatment expertise and better overall patient results for knee replacement, as well as a designated Center of Excellence for orthopedic care by Optum. This means you'll receive expert, safe and cost-effective care.
UC San Diego Health's orthopedic surgeons are the first and only in San Diego to offer customized knee replacements with the ROSA knee system — for a faster recovery and more natural feeling knee. Talk to one of our surgeons about whether a ROSA knee replacement is right for you. https://health.ucsd.edu/specia....lties/orthopedics/jo#a
Devi Shetty, founder of Narayana Health in India, reflects on the remarkable fact that, after 26 years of operation, the cost of heart surgery at Narayana Health has come down dramatically, and shares some of the strategies used to maintain high quality with low patient cost.
Learn more about the Creating Emerging Markets Project and explore its many compelling interviews: https://www.hbs.edu/creating-e....merging-markets/Page
#anatomy #histology #bytesizemed
✨If you would like my help studying about cartilage, you can check out my long-form video linked at the bottom of the screen.
💫 For more videos like this, subscribe to my channel, Byte Size Med.
📚Factual References & for Further Reading:
- DiFiore's Atlas of Histology
- Junqueira's Basic Histology
- Gartner's Concise Histology
- Openstax Anatomy and Physiology
https://openstax.org/details/b....ooks/anatomy-and-phy
- Openstax Biology
https://openstax.org/details/books/biology-2e
(The last two are links to open-source references. They are NOT affiliate links)
🌤 Note:
These are just a collection of my notes. So use them the way you would use borrowed notes from a friend. 📝
The images in this video are hand-drawn for illustration and explanation only.✍️ Hence, they may not be anatomically accurate. I am just one person making these videos. If there are any errors, that is unintentional. I try super hard to avoid them. Please let me know if you find any, so it gets clarified for other viewers. Science constantly evolves and changes. New discoveries are made everyday. So some of the information in these videos may become outdated. If you notice that, please let me know so I can update them.
⚡️Disclaimer:
These videos are NOT a substitute for a medical textbook. Textbooks are written by experts (which I do not claim to be), edited, proofread and referenced. Please use them.
The information has been sourced from multiple references as mentioned above. I draw all the pictures myself. But if I have inadvertently infringed on any copyright, that is completely unintentional. I only make these videos to impart education. If I have accidentally violated copyright in any way, do let me know so I can make the necessary changes or give credit to anyone who is owed the same.
These videos are NOT intended for patient education. They are NOT a substitute for diagnosis and treatment by a licensed medical professional. Always seek the advice of a qualified health care provider for any questions you may have regarding any medical condition, so that they can address your individual needs.
🔅They are ONLY meant to help students of medicine and health sciences with studying, and should be used for just that purpose and absolutely nothing else.
Byte Size Med. All Rights Reserved.
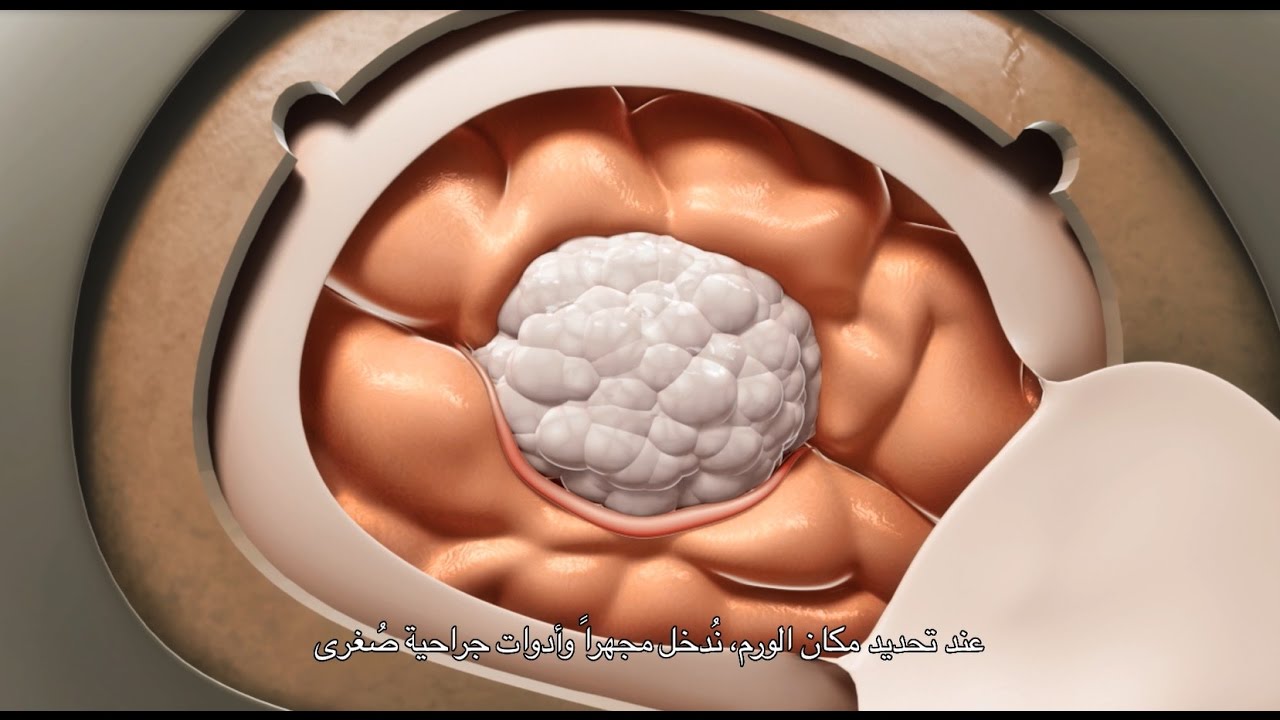
This video demonstrate Bilateral Salpingectomy for a patient suffering from hematosalpinx of one side and Hydrosalpinx other side in which one IVF has failed. Laparoscopic salpingectomy. In this less-invasive procedure, the surgeon makes 1-3 small incisions in the lower abdomen, and inserts a laparoscope into the pelvis through one of the incisions. The camera at the end of the laparoscope guides the surgeon through the procedure. The fallopian tube tissue is then removed. For more information https://www.laparoscopyhospital.com/
For more information please contact:
World Laparoscopy Hospital
Cyber City, Gurugram, NCR DELHI
INDIA 122002
Phone & WhatsApp: +919811416838, + 91 9999677788
This video demonstrates Laparoscopic Cholecystectomy Fully Explained Skin-to-Skin Video with Near Infrared Cholangiography performed by Dr R K Mishra at World Laparoscopy Hospital. A laparoscopic cholecystectomy is a minimally invasive surgical procedure that involves removing the gallbladder. It is typically performed using small incisions in the abdomen, through which a laparoscope (a thin tube with a camera and light) and surgical instruments are inserted. The surgeon uses the laparoscope to visualize the inside of the abdomen and to guide the instruments in removing the gallbladder.
Near-infrared cholangiography is a technique that uses a special camera and fluorescent dye to visualize the bile ducts during surgery. The dye is injected into the cystic duct (the tube that connects the gallbladder to the bile ducts) and the camera detects the fluorescence emitted by the dye, allowing the surgeon to see the bile ducts more clearly.
The combination of laparoscopic cholecystectomy and near-infrared cholangiography has become a standard of care in many hospitals and surgical centers. It allows for a more precise and efficient surgery, reducing the risk of complications such as bile duct injury.
The use of indocyanine green (ICG) with near-infrared imaging during laparoscopic cholecystectomy has several advantages. Here are some of them:
Better visualization of the biliary anatomy: ICG with near-infrared imaging allows for better visualization of the biliary anatomy during surgery. This helps the surgeon identify important structures, such as the cystic duct and the common bile duct, and avoid injuring them.
Reduced risk of bile duct injury: With better visualization of the biliary anatomy, the risk of bile duct injury during surgery is reduced. Bile duct injury is a serious complication that can occur during laparoscopic cholecystectomy and can lead to long-term health problems.
Improved surgical precision: ICG with near-infrared imaging also improves surgical precision. The surgeon can better see the tissues and structures being operated on, which can help reduce the risk of bleeding and other complications.
Shorter operating time: The use of ICG with near-infrared imaging can shorten the operating time for laparoscopic cholecystectomy. This is because the surgeon can more quickly and accurately identify the biliary anatomy, which can help streamline the surgery.
Overall, the use of ICG with near-infrared imaging is a valuable tool in laparoscopic cholecystectomy that can improve surgical outcomes and reduce the risk of complications.
Like any surgical procedure, laparoscopic cholecystectomy (gallbladder removal) has potential complications. Here are some of the most common ones:
Bleeding: Bleeding during or after the surgery is a possible complication of laparoscopic cholecystectomy. Most cases are minor and can be easily controlled, but in rare cases, significant bleeding may require a blood transfusion or even additional surgery.
Infection: Any surgical procedure carries a risk of infection. After laparoscopic cholecystectomy, there is a risk of infection at the site of the incisions or within the abdomen. Symptoms may include fever, pain, redness, or drainage from the incision sites.
Bile leakage: In some cases, a small amount of bile may leak from the bile ducts into the abdominal cavity after gallbladder removal. This can cause abdominal pain, fever, and sometimes requires further surgery or treatment.
Injury to nearby organs: During the surgery, there is a small risk of unintentional injury to nearby organs such as the liver, intestines, or bile ducts. This can cause additional complications and may require further treatment.
Adverse reactions to anesthesia: As with any surgery requiring general anesthesia, there is a small risk of adverse reactions to the anesthesia, such as an allergic reaction, respiratory problems, or heart complications.
Most patients recover without complications following a laparoscopic cholecystectomy, but it is important to discuss any concerns or questions with your surgeon beforehand.
Contact us
World Laparoscopy Hospital
Cyber City, Gurugram, NCR Delhi
INDIA : +919811416838
World Laparoscopy Training Institute
Bld.No: 27, DHCC, Dubai
UAE : +971525857874
World Laparoscopy Training Institute
8320 Inv Dr, Tallahassee, Florida
USA : +1 321 250 7653
Regenerate response
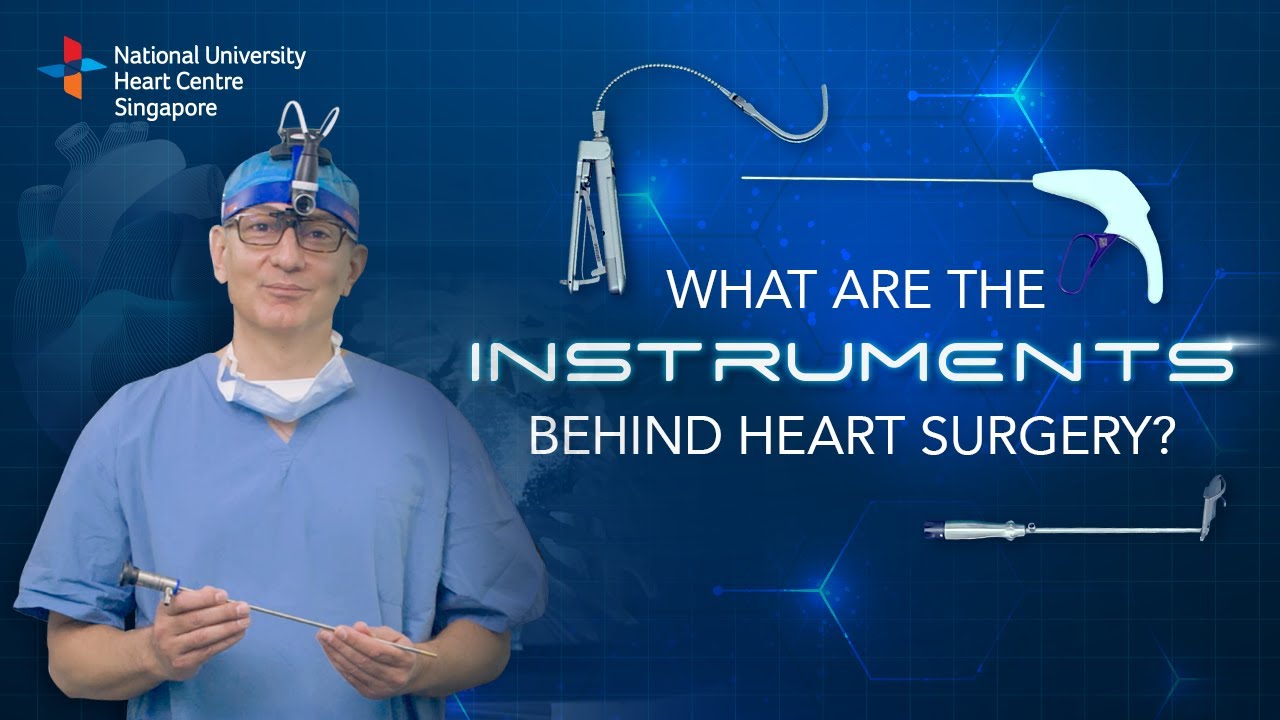
Instruments at work, innovation at play. 🔍
Watch on to discover the behind-the-scenes instruments utilised by our NUHCS cardiac surgery expert, A/Prof Theodoros Kofidis, Head of NUHCS' Department of Cardiac, Thoracic & Vascular Surgery (CTVS), for keyhole heart operations. 🔑
To find out more about Minimally Invasive Heart Surgery @ NUHCS, visit: https://[a]www.nuhcs.com.sg%2FOur-Services%2FSpecialties%2FPages%2FMinimally-Invasive-Cardiac-Surgery-Programme.aspx[/a]
Connect with us:
Instagram: @nuhcsofficial
Facebook: www.facebook.com/nuhcs
Website: www.nuhcs.com.sg
LinkedIn: www.linkedin.com/company/nuhcs
To make an appointment with the NUHCS Heart Clinic, email us at appointment@nuhs.edu.sg
#NUHCS #cardiacsurgery #heartsurgery #keyholesurgery #minimallyinvasive
💪 Get our Knee Resilience program here: https://e3rehab.com/programs/r....esilience/knee-resil
In this video, I will walk you through a comprehensive rehab program for the most commonly injured knee ligament - the MCL.
💪 PROGRAMS: https://e3rehab.com/programs/
📩 MAILING LIST (exclusive deals, offers, and information): https://e3rehab.com/newsletter/
🏆 COACHING: https://e3rehab.com/coaching/
📝 ARTICLES: https://e3rehab.com/articles/
👕 APPAREL: https://e3rehab.com/clothing/
🎧 PODCAST: https://open.spotify.com/show/....5ZbaI145Bk94Guq7olMJ
AFFILIATES:
👟 Vivo Barefoot: Get 15% off all shoes! - https://www.vivobarefoot.com/e3rehab
📓 MASS (Monthly Research Review): http://bit.ly/E3MASS
📚 CSMi: https://humacnorm.com/e3rehab
🏋️ GYM EQUIPMENT: https://e3rehab.com/affiliates/
Follow Us:
YOUTUBE: https://www.youtube.com/@e3reh....ab?sub_confirmation=
INSTAGRAM: https://www.instagram.com/e3rehab
TWITTER: https://twitter.com/E3Rehab
FACEBOOK: https://www.facebook.com/e3rehab
TIKTOK: https://www.tiktok.com/@e3rehab
Intro (0:00)
Anatomy & Function (0:08)
Classification (1:11)
Treatment Options (1:46)
Bracing (3:30)
Rehab Overview (4:28)
Early Stage (5:27)
Mid-Stage(8:50)
Late Stage/Return to Sport (21:14)
Programming (22:13)
Summary (23:47)
---
Disclaimer: The information presented is not intended as medical advice or to be a substitute for medical counseling but intended for entertainment purposes only. If you are experiencing pain, please seek the appropriate healthcare professional.
A craniotomy may be performed to treat brain tumors, blood clots, aneurysms, skull fractures, foreign objects, swelling of the brain, stroke or infection.
Be sure to have your teenager checked for hernias as they may be malevolent, Dr. Honaker gives us some insight as to why this is an important thing to have done.
Christopher J. Rapuano, MD, Director of the Cornea Service at Wills Eye Institute describes his surgical approach of a Combined Penetrating Keratoplasty (PK) and Cataract Surgery





![Histology of Exocrine Gland [Epithelium 7 of 7]](https://i.ytimg.com/vi/NkU7YJ7eYd0/maxresdefault.jpg)