Top videos
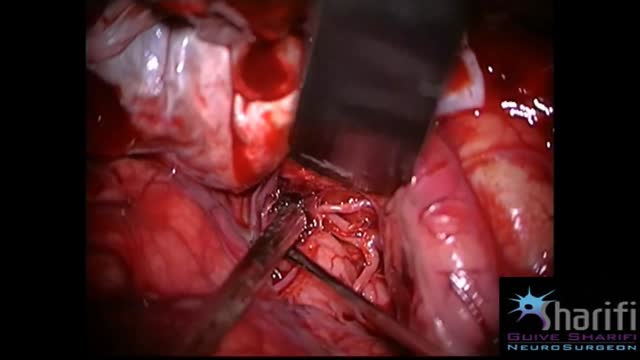
The goal of surgical clipping is to isolate an aneurysm from the normal circulation without blocking off any small perforating arteries nearby. Under general anesthesia, an opening is made in the skull, called a craniotomy. The brain is gently retracted to locate the aneurysm. A small clip is placed across the base, or neck, of the aneurysm to block the normal blood flow from entering. The clip works like a tiny coil-spring clothespin, in which the blades of the clip remain tightly closed until pressure is applied to open the blades. Clips are made of titanium and remain on the artery permanently.
Facial Tenderness
1. Ask the patient to tell you if these maneuvers causes excessive discomfort or pain. ++
2. Press upward under both eyebrows with your thumbs.
3. Press upward under both maxilla with your thumbs.
4. Excessive discomfort on one side or significant pain suggests sinusitis.
Sinus Trans illumination 1. Darken the room as much as possible. ++
2. Place a bright otoscope or other point light source on the maxilla.
3. Ask the patient to open their mouth and look for an orange glow on the hard palate.
4. A decreased or absent glow suggests that the sinus is filled with something other than air.
Temporomandibular Joint 1. Place the tips of your index fingers directly in front of the tragus of each ear. ++
2. Ask the patient to open and close their mouth.
3. Note any decreased range of motion, tenderness, or swelling.

Bone marrow biopsy and bone marrow aspiration are procedures to collect and examine bone marrow — the spongy tissue inside some of your larger bones. Bone marrow biopsy and aspiration can show whether your bone marrow is healthy and making normal amounts of blood cells. Doctors use these procedures to diagnose and monitor blood and marrow diseases, including some cancers, as well as fevers of unknown origin. Bone marrow has a fluid portion and a more solid portion. In bone marrow biopsy, your doctor uses a needle to withdraw a sample of the solid portion. In bone marrow aspiration, a needle is used to withdraw a sample of the fluid portion.

Learn about electromagnetic navigation diagnostic bronchoscopy, a new technology used to diagnose small lung cancer tumors as small as a pencil eraser before they have the chance to spread. Cleveland Clinic physician Dr. Thomas Gildea demonstrates how this endobronchial ultrasound procedure, which involves using a small camera probe inserted thru the nose into the lungs, allows doctors to reach possible cancer in the lungs that they could never reliably get to before

An excellent video demonstrating how a laparoscopy is performed to evaluate the uterus (note a small fibroid appearing as a bulge in the uterus), fallopian tubes and ovaries. Blue dye is injected into the uterus, entering the fallopian tubes and spilling from the end of the tubes into the abdominal cavity, confirming that both tubes are open