Top videos

While an anal abscess is an infection within one or more of the anal spaces, an anal fistula (Choice B) is a tunneling between the anus or rectum and another epithelial lined space (eg, the skin overlying the drainage site). Fifty percent of patients with anal abscesses will go on to develop a chronic fistula from the involved anal gland to the overlying skin. Patients with fistulas typically present with an anal abscess that persists after incision and drainage, or with a pustule-like lesion in the perianal or ischiorectal area that continually drains. Surgical repair is usually necessary to eliminate the fistula while preserving fecal continence.

Macrobiopsy of breast lesions is a complicated procedure when performed with vacuum assisted biopsy tools. The Spirotome is a hand-held needle set that doesn’t need capital investment, is ready to use and provides tissue samples of high quality in substantial amounts. In this way quantitative molecular biology is possible with one tissue sample. The Coramate is an automated version of this direct and frontal technology

Candida Albicans is more than just yeast- for most people, it's already mutated into a more aggressive fungal form that eats holes through the intestinal tract causing many of todays health problems like food allergies, autoimmune disorders, Crohn's disease, IBS, low energy and many more aggressive diseases. People need to know what it is and what to do about it.

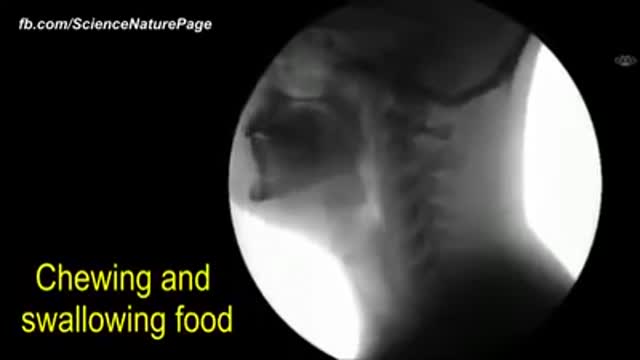
A deep cut on the palm side of your fingers, hand, wrist, or forearm can damage your flexor tendons, which are the tissues that help control movement in your hand. A flexor tendon injury can make it impossible to bend your fingers or thumb.

A parasitic twin (also known as an asymmetrical or unequal conjoined twin) is the result of the processes that produce vanishing twins and conjoined twins, and may represent a continuum between the two. Parasitic twins occur when a twin embryo begins developing in utero, but the pair does not fully separate, and one embryo maintains dominant development at the expense of the other. Unlike conjoined twins, one ceases development during gestation and is vestigial to a mostly fully-formed, otherwise healthy individual twin. The undeveloped twin is defined as parasitic, rather than conjoined, because it is incompletely formed or wholly dependent on the body functions of the complete fetus. The independent twin is called the autosite.

Dr. Horacio Asbun, Mayo Clinic in Florida, explains the Whipple procedure using this animated graphic of a pancreas. Cancer of the pancreas affects 45,000 people every year in the U.S., and it is the fourth leading cause of cancer-related deaths. The five-year overall survival rate if a tumor is detected early and surgically removed is 22 percent, versus 6 percent without early detection and surgery. To learn more, visit http://mayocl.in/2zk7FDi.
This video in Spanish/español: https://www.youtube.com/watch?v=N_zWboNMKWk

High Quality Surgical videos and uncut stories ▶ https://surgeoncut.com