Top videos
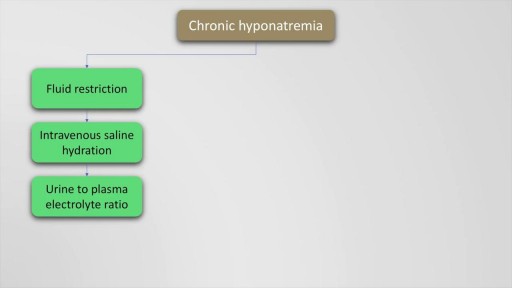
Hyponatremia is defined as a serum sodium of less than 135 Meq per litre and occurs in upto 22 % of hospitalised patients. The causes of hyponatremia may be understood based on the pre-existing volume status of the patient which may either be hypovolemic, euvolemic or hypervolemic hyponatremia. This presentation discusses in detail, the causes of these underlying conditions. Also mentioned are the clinical features and management options and therapeutic sodium targets in patients with hyponatremia. Drugs such as demeclocycline and vaptans (Tolvaptan, Conivaptan) are also mentioned as management options which may be used on a case to case basis. Finally, the all important targets of sodium correction over 24 hours are also mentioned, along with a practical formula for calculation of sodium deficit which is explained with an example.
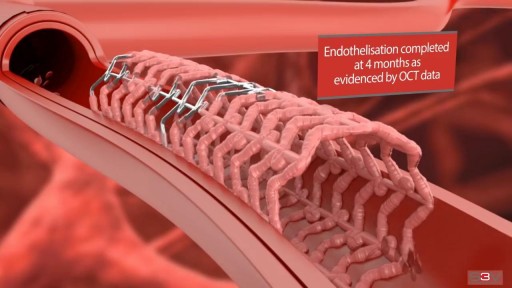
Angioplasty is a procedure to restore blood flow through the artery. You have angioplasty in a hospital. The doctor threads a thin tube through a blood vessel in the arm or groin up to the involved site in the artery. The tube has a tiny balloon on the end.
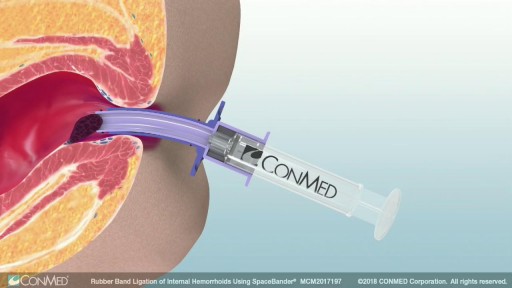
Rubber band ligation is a procedure in which the hemorrhoid is tied off at its base with rubber bands, cutting off the blood flow to the hemorrhoid. This treatment is only for internal hemorrhoids. To do this procedure, a doctor inserts a viewing instrument (anoscope) into the anus. The hemorrhoid is grasped with an instrument, and a device places a rubber band around the base of the hemorrhoid. The hemorrhoid then shrinks and dies and, in about a week, falls off. A scar will form in place of the hemorrhoid, holding nearby veins so they don't bulge into the anal canal. The procedure is done in a doctor's office. You will be asked whether the rubber bands feel too tight. If the bands are extremely painful, a medicine may be injected into the banded hemorrhoids to numb them. After the procedure, you may feel pain and have a sensation of fullness in the lower abdomen. Or you may feel as if you need to have a bowel movement. Treatment is limited to 1 to 2 hemorrhoids at a time if done in the doctor's office. Several hemorrhoids may be treated at one time if the person has general anesthesia. Additional areas may be treated at 4- to 6-week intervals.