Top videos

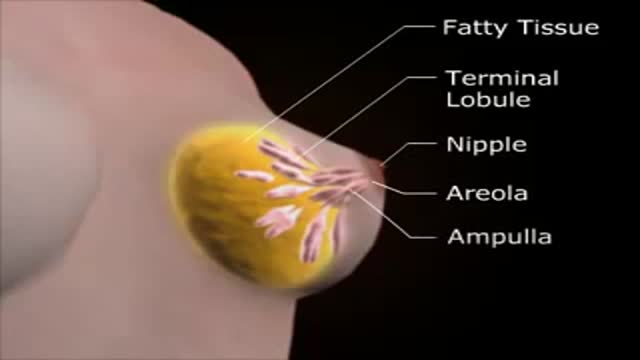
Macrobiopsy of breast lesions is a complicated procedure when performed with vacuum assisted biopsy tools. The Spirotome is a hand-held needle set that doesn’t need capital investment, is ready to use and provides tissue samples of high quality in substantial amounts. In this way quantitative molecular biology is possible with one tissue sample. The Coramate is an automated version of this direct and frontal technology

Bone marrow biopsy and bone marrow aspiration are procedures to collect and examine bone marrow — the spongy tissue inside some of your larger bones. Bone marrow biopsy and aspiration can show whether your bone marrow is healthy and making normal amounts of blood cells. Doctors use these procedures to diagnose and monitor blood and marrow diseases, including some cancers, as well as fevers of unknown origin. Bone marrow has a fluid portion and a more solid portion. In bone marrow biopsy, your doctor uses a needle to withdraw a sample of the solid portion. In bone marrow aspiration, a needle is used to withdraw a sample of the fluid portion.

New Minimally Invasive Procedure with No Pain or Downtime… From Dr. Michael Goodman, Caring For Women Wellness Center Laser Vaginal Tightening for Improved Sexual Pleasure and Relief from Minimal Urinary Incontinence Laser Vaginal Therapy for reversing Vaginal Atrophy (Good also for Breast Cancer Survivors with Vaginal Atrophy)

An excellent video demonstrating how a laparoscopy is performed to evaluate the uterus (note a small fibroid appearing as a bulge in the uterus), fallopian tubes and ovaries. Blue dye is injected into the uterus, entering the fallopian tubes and spilling from the end of the tubes into the abdominal cavity, confirming that both tubes are open
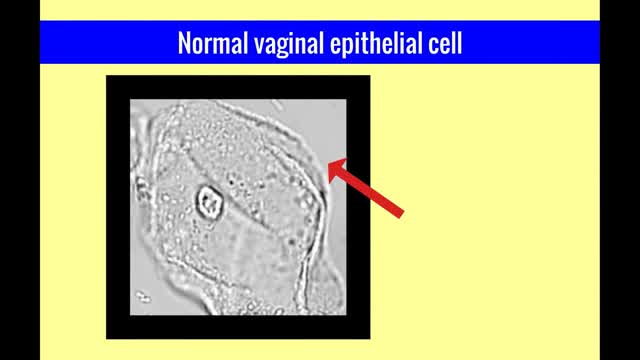
The vulvar vaginal diseases service sees referrals to help women with short--and long--term problems of the outer genital area (vulva), vagina and pelvic floor muscles including: Vulvar vaginal burning, itching, irritation and pain Vulvar Vestibulitis Pain with intercourse Discharge Yeast infections Bacterial vaginosis Pelvic floor muscle dysfunction A patient must be referred by her local health care provider. Services include: Skin care education Examinations-Your healthcare provider will examine you and talk with you about recommendations for treatment and/or management of your symptoms. Some vulvar diseases require a biopsy to diagnose the condition. Referrals-Your healthcare team may refer you to other specialists, including physical therapists or health psychologists. Separate insurance authorization is necessary for these services. The clinic staff provides general education and support to help women cope with these very personal health problems. Following a clinic visit, a letter is promptly sent to your local health care provider. The letter provides the results of your exam and the plan of care.

This is a 60 year man having large swelling of size 7cm x 5 cm behind neck for one year. Patient complained pain and tenderness over local area for 7 days and came to us.On examination punctum found in the centre of swelling and fluctuation positive.Infected sebaceous cyst diagnosis made. Incision and drainage surgery done under local anesthesia.all infected pultaceous material evacuated.Pus culture sent and antibiotics given as per sensitivity report. Patient improved with daily dressing.
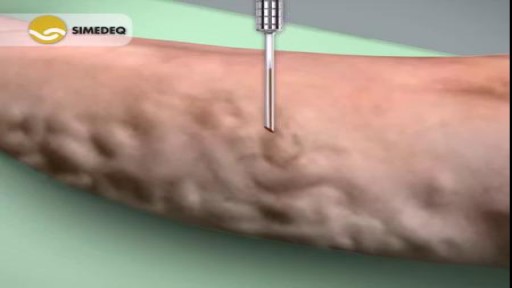
Varicose veins are generally benign. The cause of this condition is not known. For many people, there are no symptoms and varicose veins are simply a cosmetic concern. In some cases, they cause aching pain and discomfort or signal an underlying circulatory problem. Treatment involves compression stockings, exercise, or procedures to close or remove the veins.
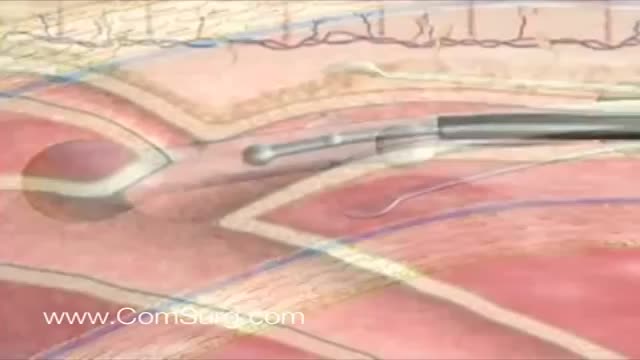
Like the VenaCure EVLT® procedure, which uses a laser to ablate the varicose vein, VNUS RF treatment is an alternative to more invasive leg stripping surgery. It is used primarily to treat the great saphenous veins (GSV), small saphenous vein (SSV), and other superficial veins in the legs.