Top videos

Ellis demonstrates how to perform a sterile wound dressing change. It would be appropriate to perform hand hygiene between glove changes.
Our Critical Nursing Skills video tutorial series is taught by Ellis Parker MSN, RN-BC, CNE, CHS and intended to help RN and PN nursing students study for your nursing school exams, including the ATI, HESI and NCLEX.
#NCLEX #ClinicalSkills #woundcare #HESI #Kaplan #ATI #NursingSchool #NursingStudent #Nurse #RN #PN #Education #LVN #LPN #nurseeducator
00:00 What to expect
00:51 Prepping for wound dressing change
1:15 Removing the old wound dressing
1:40 Assessing a wound
2:05 Setting up sterile field
2:49 Sterile gloving
4:02 Preparing equipment for wound dressing change
5:09 Cleaning a wound
6:13 Drying a wound
6:28 Packing a wound
7:19 Covering a wound
7:47 Labeling a wound dressing
🚨 Reminder: shipping deadlines are looming 👀
🎁 Regular Shipping: Order by Friday, December 15
🚀 Expedited Shipping: Order by Monday, December 18
🔍 Still searching for last-minute gifts? Consider a Level Up RN Gift Card! 💌 It’s not only a thoughtful present but also the perfect way to share treasures like Pharmacology Flashcards OR digital treasures like Flashables Digital Nursing Flashcards & the Level Up RN membership. Give the gift of knowledge this holiday season! 🧠⚡️💖 bit.ly/LevelUpRNGC
🚪 Access our Cram Courses, Quizzes and Videos all in one ad free space with Level Up RN Membership https://bit.ly/LevelUpRNMembership
Want more ways to MASTER Clinical Skills? Check out our flashcards & videos!
👇👇👇👇👇👇👇👇👇👇
👉 https://bit.ly/clinicalnursingskills 👈
☝️👆☝️👆☝️👆☝️👆☝️👆
This is your one-stop-shop for materials to help you LEARN & REVIEW so you can PASS Nursing School.
🤔🤔🤔 DO YOU WANT TO PASS your classes, proctored exams and the NCLEX? 🤔🤔🤔 Our resources are the best you can buy. They are built with a single goal: help you pass with no fluff. Everything you need, and nothing you don’t. Don’t take our word for it, though! Check out our hundreds of ⭐️⭐️⭐️⭐️⭐️ reviews from nurses who passed their exams and the NCLEX with Level Up RN.
🗂️ Our Ultimate Nursing School Survival kit is your number 1 resource to get through nursing school and to pass the NCLEX. Whether you're just starting school or you’re already prepping for the NCLEX, this bundle of flashcards is the best you can buy. It covers all the information you need to know to pass all your exams and it has FREE shipping!
➡️ https://bit.ly/TUNSSK ⬅️
L👀king for EVEN MORE resources to survive Nursing School? Make your Nursing School experience your own! Life’s difficult enough—learning shouldn’t be.
🪅 Games https://nursesquad.com
💻 Digital resources https://bit.ly/NursingStudyCourses
📅 Organizational tools https://bit.ly/OrganizingSchool
✨Want perks? Join our channel!
https://youtube.com/leveluprn/join
🏷 Head to https://leveluprn.com/specials for all our latest deals!🥳️
📧 LOOKING FOR FREE RESOURCES TO HELP WITH YOUR EXAMS? Get exclusive tips, latest video releases and more delivered to your email!
➡️ https://leveluprn.com/signup ⬅️
⚕ 👩 LEVEL UP NURSE SQUAD 👩⚕️
All of the nurses at Level Up RN are here to help! Cathy Parkes started helping her fellow classmates back when she was in nursing school, tutoring so they could pass their exams and graduate. After she got her BSN and started working as an RN at Scripps Encinitas Hospital, she started this YouTube channel to help nursing students around the world. Since then she has built a team of top-notch dedicated nurses and nurse educators who are focused on improving nursing education and supporting career advancement for nurses everywhere. With flashcards, videos, courses, organizational tools and more, we are singularly focused on helping students and nurses Level Up on their exams and nursing careers.

Common Benign Pain Syndromes--Symptoms and Etiology:
1. Non-specific musculoskeletal pain: This is the most common cause of back pain. Patients present with lumbar area pain that does not radiate, is worse with activity, and improves with rest. There may or may not be a clear history of antecedent over use or increased activity. The pain is presumably caused by irritation of the paraspinal muscles, ligaments or vertebral body articulations. However, a precise etiology is difficulty to identify.
2. Radicular Symptoms: Often referred to as "sciatica," this is a pain syndrome caused by irritation of one of the nerve roots as it exits the spinal column. The root can become inflamed as a result of a compromised neuroforamina (e.g. bony osteophyte that limits size of the opening) or a herniated disc (the fibrosis tears, allowing the propulsus to squeeze out and push on the adjacent root). Sometimes, it's not precisely clear what has lead to the irritation. In any case, patient's report a burning/electric shock type pain that starts in the low back, traveling down the buttocks and along the back of the leg, radiating below the knee. The most commonly affected nerve roots are L5 and S1.
3. Spinal Stenosis: Pain starts in the low back and radiates down the buttocks bilaterally, continuing along the backs of both legs. Symptoms are usually worse with walking and improve when the patient bends forward. Patient's may describe that they relieve symptoms by leaning forward on their shopping carts when walking in a super market. This is caused by spinal stenosis, a narrowing of the central canal that holds the spinal cord. The limited amount of space puts pressure on the nerve roots when the patient walks, causing the symptoms (referred to as neurogenic claudication). Spinal stenosis can be congenital or develop over years as a result of djd of the spine. As opposed to true claudication (pain in calfs/lower legs due to arterial insufficiency), pain resolves very quickly when person stops walking and assumes upright position. Also, peripheral pulses should be normal.
4. Mixed symptoms: In some patients, more then one process may co-exist, causing elements of more then one symptom syndrome to co-exist.

A subdural hematoma is most often the result of a severe head injury. This type of subdural hematoma is among the deadliest of all head injuries. The bleeding fills the brain area very rapidly, compressing brain tissue. This often results in brain injury and may lead to death. Subdural hematomas can also occur after a minor head injury. The amount of bleeding is smaller and occurs more slowly. This type of subdural hematoma is often seen in older adults. These may go unnoticed for many days to weeks, and are called chronic subdural hematomas. With any subdural hematoma, tiny veins between the surface of the brain and its outer covering (the dura) stretch and tear, allowing blood to collect. In older adults, the veins are often already stretched because of brain shrinkage (atrophy) and are more easily injured.
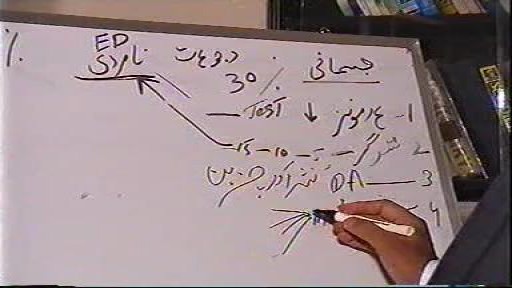
How to Improve Sexual Health or Stamina part 4 All Solution of Male Disorder Male Infertility Diagnostic and Treatment Re-Slim Care Latest Technology in Pakistan Dr. Aslam Naveed is a well known sexologist in Pakistan. He has treated more than 1 Lac patients since last 30 years of clinical Practice in sexology, he knows how to help the people facing sexual disorders. Contact: 02134965050, 03432821919 www.sexologistpakistan.com https://www.facebook.com/menssexcareclinic/ https://youtu.be/_fRbtwWtLoE Part 1 https://youtu.be/S17bCnwCLuI Part 2 https://youtu.be/CPAXxkdz7mM Part 3 https://youtu.be/YlsdBZJ4prg Part 4 https://youtu.be/fylxbK4azvs Part 5 https://youtu.be/Zb8TcdgJ7Io Part 6 https://youtu.be/0wbDDNAwsmo Part 7 https://youtu.be/gHDmwfsMgTw Part 8 https://youtu.be/IasXoRKUlV4 Part 9 ADDRESS: Men’s Care Modern Hospital, Opposite, Safari Park, University Road, Karachi, Pakistan.

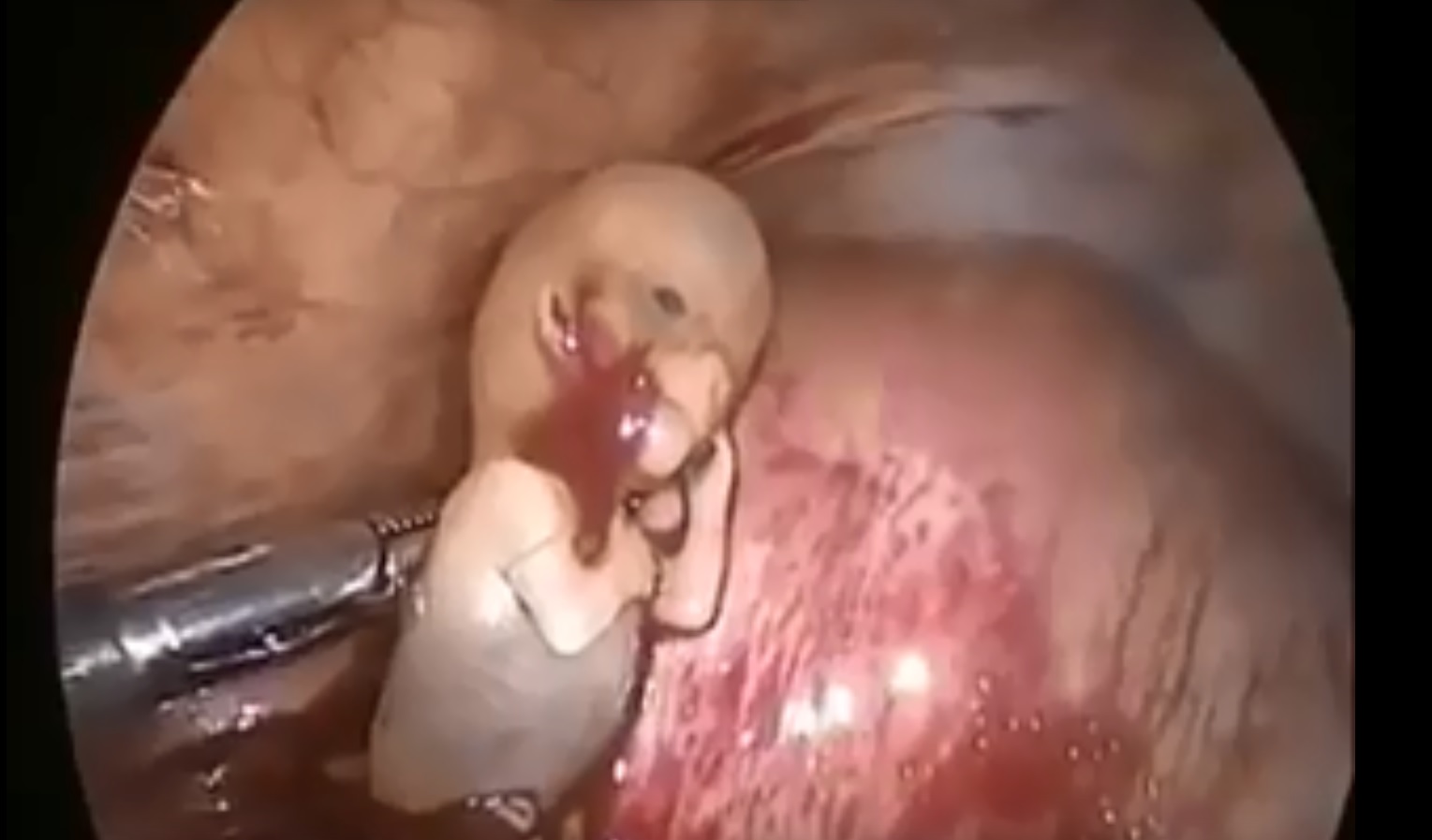
A breech birth occurs when a baby is born bottom first instead of head first. Around 3-5% of pregnant women at term (37–40 weeks pregnant) will have a breech baby. Most babies in the breech position are born by a caesarean section because it is seen as safer than being born vaginally.

A hematoma is a collection of blood outside of a blood vessel Some causes of hematomas are as pelvic bone fractures, fingernail injuries (subungual), bumps, passing blood clots, blood clot in the leg (DVT), blood cancers, and excessive alcohol use.

Most babies will move into delivery position a few weeks prior to birth, with the head moving closer to the birth canal. When this fails to happen, the baby’s buttocks and/or feet will be positioned to be delivered first. This is referred to as “breech presentation.” Breech births occur in approximately 1 out of 25 full-term births.

If you use condoms perfectly every single time you have sex, they’re 98% effective at preventing pregnancy. But people aren’t perfect, so in real life condoms are about 85% effective — that means about 15 out of 100 people who use condoms as their only birth control method will get pregnant each year.

As you consider Fort HealthCare and our Pediatric Surgical Services, here is a quick tour to give you and your child an idea of what to expect.
We look forward to helping you.
To find out more information, please visit forthealthcare.com/PediatricSurgery
Video production by Highlights Media, LLC

Emergency contraception is a method of birth control you can use if you had sex without using birth control or if your birth control method did not work correctly. You must use emergency contraception as soon as possible after unprotected sex. Emergency contraception pills are different from the abortion pill. If you are already pregnant, emergency contraception pills do not stop or harm your pregnancy. Emergency contraception has also been called the "morning-after pill," but you do not need to wait until the morning after unprotected sex to take it. Emergency contraception is not meant to be used for regular birth control. Talk to your doctor or nurse about regular birth control to help prevent pregnancy. Nearly half of all pregnancies in the United States are unplanned.1

It flattens the natural curve of the spine, which can lead to lower back pain. Sleeping all night with the head turned to one side also strains the neck. If this is the preferred position, try using pillows to gradually train the body to sleep on one side

ThermiVa is a non-surgical vaginal tightening treatment for women who want to reclaim what childbirth or aging may have taken away. Using the same technology that’s used in ThermiTight and ThermiSmooth, radiofrequency energy is sent to the desired area (internally or externally), heating the tissue and stimulating the body’s own collagen. ThermiVa is performed in three treatments over the course of three months.

What is Venipuncture? While venipuncture can refer to a variety of procedures, including the insertion of IV tubes into a vein for the direct application of medicine to the blood stream, in phlebotomy venipuncture refers primarily to using a needle to create a blood evacuation point. As a phlebotomist, you must be prepared to perform venipuncture procedures on adults, children, and even infants while maintaining a supportive demeanor and procedural accuracy. Using a variety of blood extraction tools, you must be prepared to respond to numerous complications in order to minimize the risk to the patient while still drawing a clean sample. In its entirety, venipuncture includes every step in a blood draw procedure—from patient identification to puncturing the vein to labeling the sample. Patient information, needle placement, and emotional environment all play a part in the collection of a blood sample, and it's the fine details that can mean the difference between a definite result and a false positive. After placing the tourniquet and finding the vein, it's time for the phlebotomist to make the complex choice on what procedure will best suit the specific situation. Keeping this in mind, it should be noted that the following information is not an instructional guide on how to perform these phlebotomy procedures. Rather, the information below is intended to serve as an educational resource to inform you of the equipment and procedures you will use. Venipuncture Technqiues Venipuncture with an Evacuated or Vacuum Tube: This is the standard procedure for venipuncture testing. Using a needle and sheath system, this procedure allows multiple sample tubes to be filled through a single puncture. This procedure is ideal for reducing trauma to patients. After drawing the blood, the phlebotomist must make sure the test stopper is correctly coded and doesn't contact exposed blood between samples. Venipuncture with a Butterfly Needle : This is a specialized procedure that utilizes a flexible, butterfly needle adaptor. A butterfly needle has two plastic wings (one on either side of the needle) and is connected to a flexible tube, which is then attached to a reservoir for the blood. Due to the small gauge of the needle and the flexibility of the tube, this procedure is used most often in pediatric care, where the patients tend to have smaller veins and are more likely to move around during the procedure. After being inserted into a vein at a shallow angle, the butterfly needle is held in place by the wings, which allow the phlebotomist to grasp the needle very close to the skin. Phlebotomists should be careful to watch for blood clots in the flexible tubing. Venipuncture with a Syringe: This technique is typically only used when there is a supply shortage, or when a technician thinks it is the appropriate method. It uses the classic needle, tube, and plunger system, operating in a similar manner to the vacuum tube but requiring multiple punctures for multiple samples. Additionally, after the blood is drawn it must be transferred to the appropriate vacuum tube for testing purposes. If you choose to use this method, remember to check for a sterile seal, and use a safety device when transferring the sample. Fingerstick (or Fingerprick): This procedure uses a medical lance to make a small incision in the upper capillaries of a patient's finger in order to collect a tiny blood sample. It is typically used to test glucose and insulin levels. When performing a Fingerstick, the phlebotomist should remember to lance the third or fourth finger on the non-dominant arm. Never lance the tip or the center of the finger pad; instead, lance perpendicular to the fingerprint lines. Heelstick (or Heelprick): Similar to the Fingerstick procedure, this process is used on infants under six months of age. A medical lance is used to create a small incision on the side of an infant's heel in order to collect small amounts of blood for screening. As with a Fingerstick, the incision should be made perpendicular to the heel lines, and it should be made far enough to the left or right side of the heel to avoid patient agitation. Before performing a Heelstick, the infant's heel should be warmed to about 42 degrees Celsius in order to stimulate capillary blood and gas flow. Therapeutic Phlebotomy: This involves the actual letting of blood in order to relieve chemical and pressure imbalances within the blood stream. Making use of a butterfly needle, this therapy provides a slow removal of up to one pint of blood. Though the blood removed is not used for blood transfusions, the procedure and concerns are the same as with routine blood donation. As with any phlebotomy procedure, one should pay close attention to the patient in order to prevent a blood overdraw. Bleeding Time: A simple diagnostic test that is used to determine abnormalities in blood clotting and platelet production. A shallow laceration is made, followed by sterile swabbing of the wound every 30 seconds until the bleeding stops. Average bleed times range between one and nine minutes. As a phlebotomist, you should familiarize yourself with the application and cross-application of these procedures in order to recognize when a procedure is necessary, and what the risks are for each.