Top videos

This video: Patent ductus arteriosus (PDA) is a persistent opening between two major blood vessels leading from the heart. The opening, called the ductus arteriosus, is a normal part of a baby's circulatory system before birth that usually closes shortly after birth. If it remains open, however, it's called a patent ductus arteriosus. A small patent ductus arteriosus often doesn't cause problems and might never need treatment. However, a large patent ductus arteriosus left untreated can allow poorly oxygenated blood to flow in the wrong direction, weakening the heart muscle and causing heart failure and other complications. Treatment options for a patent ductus arteriosus include monitoring, medications and closure by cardiac catheterization or surgery.

Visit http://www.nasalcleanse.com/index.php after watching our video on NasalCare nasal irrigation versus sinus sprays for sinusitis & sinus congestion relief. Learn how & why this natural sinus remedy really works! Unlike the temporary relief offered by chemical-laden nasal sprays, our patented NasalCare® Nasal Rinse System ensures comfortable and effective delivery throughout the nasal passages, preventing sinus infection, allergy and post nasal drip. A soothing mix of sea salt and Aloe Vera extract washes away nasal irritants and the common causes of colds and flu without the potential addiction that comes with nasal spray use. NasalCare also acts as a sinus wash for allergy treatment. Used for centuries in the Orient as a preventative measure for all sinus conditions, nasal irrigation is just catching on here. Catch us now and stop catching colds and the flu – the natural way! Order online at: http://www.nasalcleanse.com/index.php.
ormal sperm densities range from 15 million to greater than 200 million sperm per milliliter of semen. You are considered to have a low sperm count if you have fewer than 15 million sperm per milliliter or less than 39 million sperm total per ejaculate.

The physical signs of pregnancy are easy to recognize -- nausea, fatigue, that swollen belly and (often) a healthy glow. But what if you had these telltale pregnancy symptoms -- and weren't actually pregnant? As crazy as it sounds, it does happen. False pregnancy, or pseudocyesis, is a condition in which a woman believes that she's pregnant, yet conception hasn't taken place and no baby is forming inside. Common, and often lasting, pregnancy symptoms help to reinforce this idea, which can lead a woman to be absolutely certain she's expecting, for months or even years!

Butt implants are a popular plastic surgery procedure among those who wish to enhance the appearance, shape, and size of their rear ends. Buttock augmentation involves the surgical insertion of artificial body implants into a patient’s buttocks to create a larger, shapelier, and more sensuous rear end. Patients who have underdeveloped buttocks can achieve a more proportionate figure with butt implants. Women who wish to achieve an “hour glass” figure or are unhappy with the size of their buttocks can benefit from female butt implants. Men with flat or poorly developed buttocks can enhance the shape of the area to their liking with male butt implants. Many buttock augmentation patients say that their clothes fit better, they feel more attractive, and their confidence levels have improved.

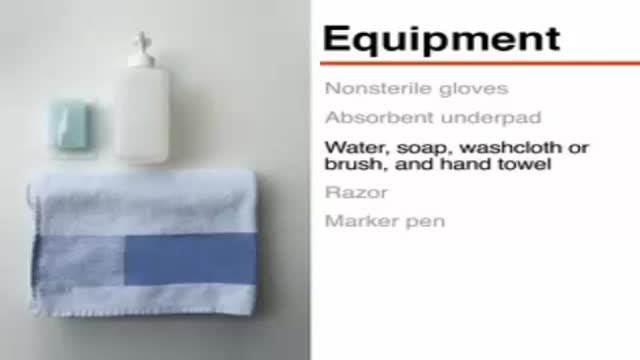
Leopold's Maneuvers are difficult to perform on obese women and women who have hydramnios. The palpation can sometimes be uncomfortable for the woman if care is not taken to ensure she is relaxed and adequately positioned. To aid in this, the health care provider should first ensure that the woman has recently emptied her bladder. If she has not, she may need to have a straight urinary catheter inserted to empy it if she is unable to micturate herself. The woman should lie on her back with her shoulders raised slightly on a pillow and her knees drawn up a little. Her abdomen should be uncovered, and most women appreciate it if the individual performing the maneuver warms their hands prior to palpation. First maneuver: Fundal Grip While facing the woman, palpate the woman's upper abdomen with both hands. A professional can often determine the size, consistency, shape, and mobility of the form that is felt. The fetal head is hard, firm, round, and moves independently of the trunk while the buttocks feel softer, are symmetric, and the shoulders and limbs have small bony processes; unlike the head, they move with the trunk. Second maneuver After the upper abdomen has been palpated and the form that is found is identified, the individual performing the maneuver attempts to determine the location of the fetal back. Still facing the woman, the health care provider palpates the abdomen with gentle but also deep pressure using the palm of the hands. First the right hand remains steady on one side of the abdomen while the left hand explores the right side of the woman's uterus. This is then repeated using the opposite side and hands. The fetal back will feel firm and smooth while fetal extremities (arms, legs, etc.) should feel like small irregularities and protrusions. The fetal back, once determined, should connect with the form found in the upper abdomen and also a mass in the maternal inlet, lower abdomen. Third maneuver: Pawlick's Grip In the third maneuver the health care provider attempts to determine what fetal part is lying above the inlet, or lower abdomen.[2] The individual performing the maneuver first grasps the lower portion of the abdomen just above the symphysis pubis with the thumb and fingers of the right hand. This maneuver should yield the opposite information and validate the findings of the first maneuver. If the woman enters labor, this is the part which will most likely come first in a vaginal birth. If it is the head and is not actively engaged in the birthing process, it may be gently pushed back and forth. The Pawlick's Grip, although still used by some obstetricians, is not recommended as it is more uncomfortable for the woman. Instead, a two-handed approach is favored by placing the fingers of both hands laterally on either side of the presenting part. Fourth maneuver The last maneuver requires that the health care provider face the woman's feet, as he or she will attempt to locate the fetus' brow. The fingers of both hands are moved gently down the sides of the uterus toward the pubis. The side where there is resistance to the descent of the fingers toward the pubis is greatest is where the brow is located. If the head of the fetus is well-flexed, it should be on the opposite side from the fetal back. If the fetal head is extended though, the occiput is instead felt and is located on the same side as the back. Cautions Leopold's maneuvers are intended to be performed by health care professionals, as they have received the training and instruction in how to perform them. That said, as long as care taken not to roughly or excessively disturb the fetus, there is no real reason it cannot be performed at home as an informational exercise. It is important to note that all findings are not truly diagnostic, and as such ultrasound is required to conclusively determine the fetal position.
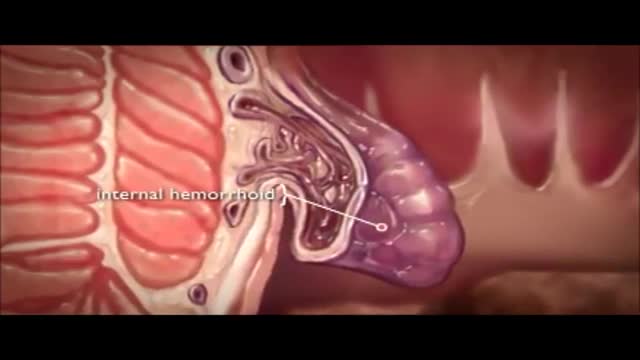
The veins around your anus tend to stretch under pressure and may bulge or swell. Swollen veins (hemorrhoids) can develop from an increase in pressure in the lower rectum. Factors that might cause increased pressure include: Straining during bowel movements.
Invasive intracranial pressure monitoring. The most common surgically placed monitors for ICP measurement are intraventricular catheters (external ventricular drain [EVD] or a ventriculostomy drain) and fiberoptic ICP monitors implanted into the parenchyma of the brain.
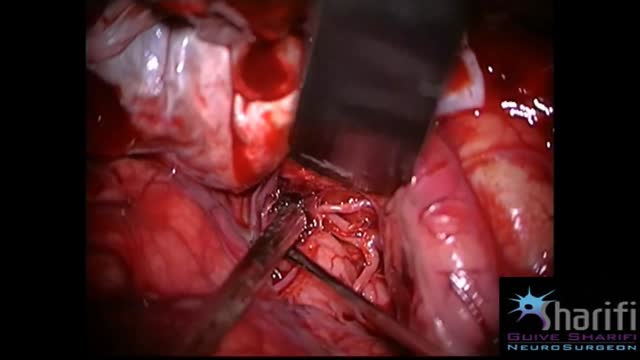
The goal of surgical clipping is to isolate an aneurysm from the normal circulation without blocking off any small perforating arteries nearby. Under general anesthesia, an opening is made in the skull, called a craniotomy. The brain is gently retracted to locate the aneurysm. A small clip is placed across the base, or neck, of the aneurysm to block the normal blood flow from entering. The clip works like a tiny coil-spring clothespin, in which the blades of the clip remain tightly closed until pressure is applied to open the blades. Clips are made of titanium and remain on the artery permanently.
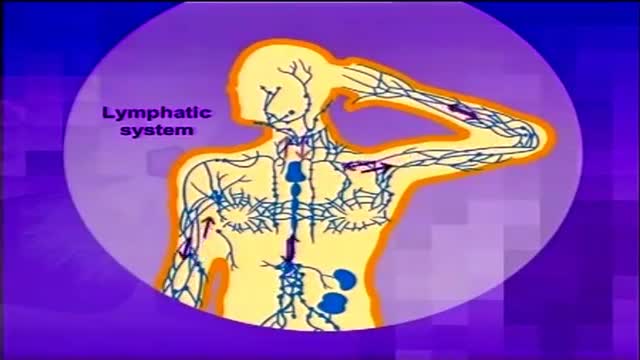
Lymphoma is cancer of the lymph system (or lymphatic system), which is part of our immunity. It is characterized by the formation of solid tumors in the immune system.1 The cancer affects immune cells called lymphocytes, which are white blood cells. Diagram of the lymphatic system The lymphatic system is a system of vessels that branch back from virtually all our tissues to drain excess fluids and present foreign material to the lymph nodes. Learn more about the lymphatic system here. Statistics from the US National Cancer Institute estimate that there are nearly 20 cases of non-Hodgkin's lymphoma for every 100,000 people in the American population.2 Hodgkin's lymphoma, meanwhile, is relatively rare, with around three cases in every 100,000 people.3