Top videos
Insulin is a hormone made by the pancreas that allows your body to use sugar (glucose) from carbohydrates in the food that you eat for energy or to store glucose for future use. Insulin helps keeps your blood sugar level from getting too high (hyperglycemia) or too low (hypoglycemia). The cells in your body need sugar for energy. However, sugar cannot go into most of your cells directly. After you eat food and your blood sugar level rises, cells in your pancreas (known as beta cells) are signaled to release insulin into your bloodstream. Insulin then attaches to and signals cells to absorb sugar from the bloodstream. Insulin is often described as a “key,” which unlocks the cell to allow sugar to enter the cell and be used for energy.

Learn about electromagnetic navigation diagnostic bronchoscopy, a new technology used to diagnose small lung cancer tumors as small as a pencil eraser before they have the chance to spread. Cleveland Clinic physician Dr. Thomas Gildea demonstrates how this endobronchial ultrasound procedure, which involves using a small camera probe inserted thru the nose into the lungs, allows doctors to reach possible cancer in the lungs that they could never reliably get to before

Bone marrow biopsy and bone marrow aspiration are procedures to collect and examine bone marrow — the spongy tissue inside some of your larger bones. Bone marrow biopsy and aspiration can show whether your bone marrow is healthy and making normal amounts of blood cells. Doctors use these procedures to diagnose and monitor blood and marrow diseases, including some cancers, as well as fevers of unknown origin. Bone marrow has a fluid portion and a more solid portion. In bone marrow biopsy, your doctor uses a needle to withdraw a sample of the solid portion. In bone marrow aspiration, a needle is used to withdraw a sample of the fluid portion.

An excellent video demonstrating how a laparoscopy is performed to evaluate the uterus (note a small fibroid appearing as a bulge in the uterus), fallopian tubes and ovaries. Blue dye is injected into the uterus, entering the fallopian tubes and spilling from the end of the tubes into the abdominal cavity, confirming that both tubes are open
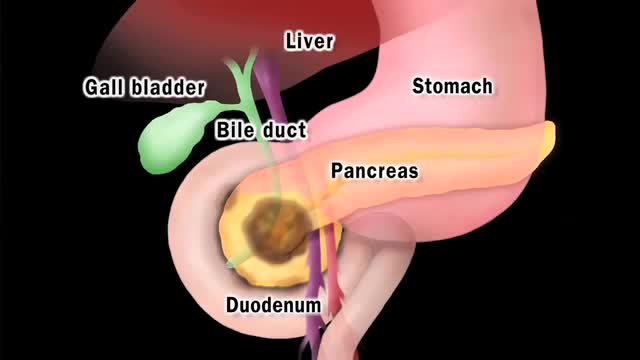
Pancreatic cancer begins in the tissues of your pancreas — an organ in your abdomen that lies horizontally behind the lower part of your stomach. Your pancreas secretes enzymes that aid digestion and hormones that help regulate the metabolism of sugars. Pancreatic cancer often has a poor prognosis, even when diagnosed early. Pancreatic cancer typically spreads rapidly and is seldom detected in its early stages, which is a major reason why it's a leading cause of cancer death. Signs and symptoms may not appear until pancreatic cancer is quite advanced and complete surgical removal isn't possible.

New Minimally Invasive Procedure with No Pain or Downtime… From Dr. Michael Goodman, Caring For Women Wellness Center Laser Vaginal Tightening for Improved Sexual Pleasure and Relief from Minimal Urinary Incontinence Laser Vaginal Therapy for reversing Vaginal Atrophy (Good also for Breast Cancer Survivors with Vaginal Atrophy)
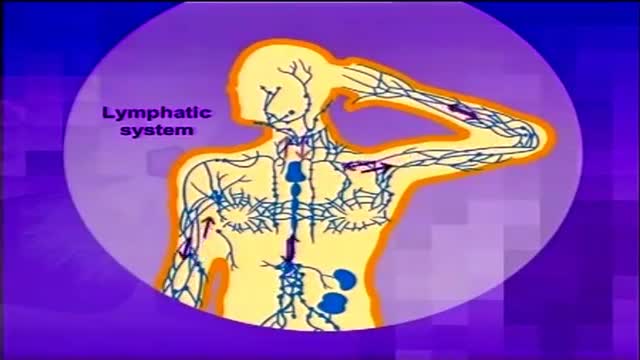
Lymphoma is cancer of the lymph system (or lymphatic system), which is part of our immunity. It is characterized by the formation of solid tumors in the immune system.1 The cancer affects immune cells called lymphocytes, which are white blood cells. Diagram of the lymphatic system The lymphatic system is a system of vessels that branch back from virtually all our tissues to drain excess fluids and present foreign material to the lymph nodes. Learn more about the lymphatic system here. Statistics from the US National Cancer Institute estimate that there are nearly 20 cases of non-Hodgkin's lymphoma for every 100,000 people in the American population.2 Hodgkin's lymphoma, meanwhile, is relatively rare, with around three cases in every 100,000 people.3
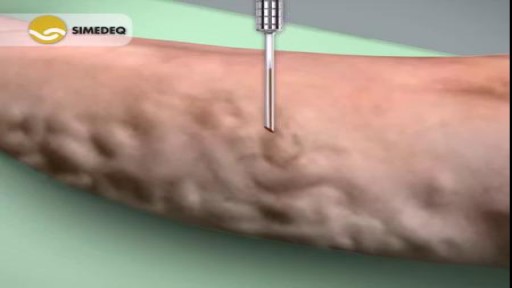
Varicose veins are generally benign. The cause of this condition is not known. For many people, there are no symptoms and varicose veins are simply a cosmetic concern. In some cases, they cause aching pain and discomfort or signal an underlying circulatory problem. Treatment involves compression stockings, exercise, or procedures to close or remove the veins.