Top videos

Lattrell Wells was a perfect candidate for the MACI procedure. Dr. Michael O'Malley is a sports medicine surgeon at Carilion Clinic, "It’s a two stage procedure. So what we do is we actually harvest a small portion of the patient's cartilage and bone cells and we send it to a lab where the lab then that grows additional cartilage cells. It comes back to us in a little sheet and six weeks after that initial surgery, we re-implant the cartilage in a second surgery where we implant that sheet depending on the size of lesion right where his defect. This the only option where there’s virtually no risk of any kind of graft rejection or anything of that nature.
Prostate biopsy is a procedure in which small hollow needle-core samples are removed from a man's prostate gland to be examined microscopically for the presence of cancer. It is typically performed when the result from a PSA blood test rises to a level that is associated with the possible presence of prostate cancer.

Debridement is the removal of necrotic tissue, foreign debris, bacterial growth, callus, wound edge, and wound bed tissue from chronic wounds in order to stimulate the wound healing process. Stimulation of wound healing mediated by debridement is thought to occur by the conversion of a chronic non-healing wound environment to an acute healing environment through the removal of cells that are not responsive to endogenous healing stimuli. Debridement is used commonly in standard wound treatment of diabetic foot ulcers (DFUs). Methods of debridement include surgery (sharp debridement), chemical debridement (antiseptics, polysaccharide beads, pastes), autolytic (hydrogels, hydrocolloids and transparent films), biosurgery (maggots), mechanical (hydrodebridement), and biochemical debridement (enzyme preparations). Callus is a buildup of keratinized skin formed under conditions of repeated pressure or friction and may contribute to ulcer formation by creating focal areas of high plantar pressure. The debridement of callus has been proposed to be relevant for both treatment and prevention of DFU. The purpose of this report is to retrieve and review existing evidence of comparative clinical effectiveness of different methods of debridement for the treatment of DFUs. Additionally examined in this report is the clinical effectiveness for treatment and prevention of DFU using callus debridement. Cost-effectiveness, and existing debridement guidelines for the treatment of DFUs will also be reviewed.

Lumpectomy means that a focal area of cancer is going to be removed. A lot of patients with a lumpectomy don’t need any specific breast reconstruction, explains Dr. Miguel Angel Medina, Director of Microsurgery with Miami Cancer Institute.
Al the end of surgical treatment, all those patients go on to need radiation therapy. For patients who have large breasts, physicians have to take a larger lumpectomy than normal.
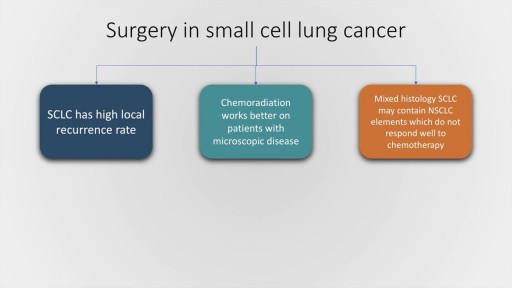
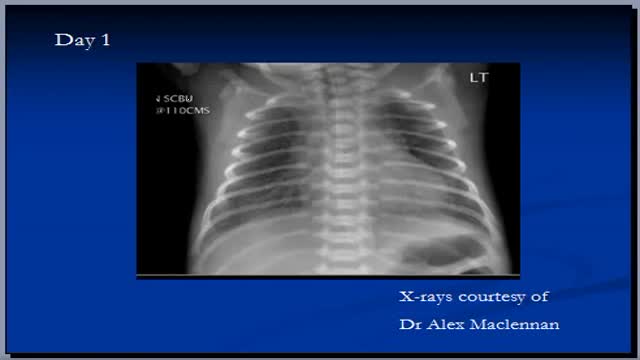
Small cell lung cancer, which occurs almost exclusively in smokers, is a malignancy characterised by rapid doubling time, high growth fraction and widespread metastasis at presentation. In this presentation, we will briefly discuss the classification of pulmonary Neuro-endocrine tumours by the World Health Organisation followed by a detailed discussion of the clinical features, lab evaluation and management of SCLC, both limited and extended stage. The frontline therapy in small cell lung cancer is etoposide and cisplatin along with thoracic radiotherapy and prophylactic cranial irradiation in patients who have a good response to therapy. Hyperfractionation of radiotherapy may provide some benefit but is also associated with increase incidence of complications. Newer agents for SCLC include Vandetanib and immunotherapy molecules, such as Iplimumab and nivolumab.

Commentary:
0:24
He may not look like he’s in good condition but you can guesst that his somewhere in nirvana at this point
0:44
After the operation, this patient loses more than just color in his skin but apparently he loses his nipples as well
1:43
This sedated patient is equipped with his own hand-gun. No pun intended
2:17
His anesthesia dose came with the usual side effects of crazy talk with a dash of attitude and sarcasm
3:17
The only thing crazier than love is being sedated during an endometriosis surgery
4:36
This may come as a surprise to some but penguins don’t actually reside in Alaska. In case you didn’t know that well now you do
5:09
If the doctor advises you against something you can’t resist doing, how many of us would still listen to him?
6:35
When them meds start kicking in , it’s time to frame this experience as an excuse to divulge some of your secret fantasies
7:05
There’s a time and place dirty jokes but anesthesia told this guy any times the right time
7:24
Her 16 year old son talks about the last thing he remembers right after surgery and this is what he says
8:35
She’s definitely not in the mood at all. I wouldn’t wanna tick her off during this time if I were you
8:44
A feeling of relief after your operation may be followed by some emotional changes such as mood swings and over sensitivity
9:44
Even if you do say something you wouldn't normally say while you are under sedation, according to some doctors, “it's always kept within the operating room”
10:38
The beeping sounds of the medical equipments tip this patient over the edge. so she tries to drown out the noise with her own voice
11:08
Anyone who's received anesthesia can attest to feeling pretty loopy. Although many won't remember it's fairly common to say some wacky things after waking up
11:53
It's typical for people to feel sad or vulnerable after surgery. Kind of like how this girl is feeling right now
12:04
If she wasn’t under the influence in the hospital right now , it would be pretty hard to justify this type of behavior
12:17
Imagine working as an anesthesiologist. You might become numb to a lot of strange behaviors and everything unusual becomes the new norm for you
► Subscribe: https://bit.ly/3I4zXBT
Top Special Videos: https://bit.ly/3o64YOa
Acts Of Kindness: https://bit.ly/3E5FmXh
Try Not To Laugh Videos: https://bit.ly/3leRpdl
Social media:
► INSTAGRAM: https://www.instagram.com/topthings.tt/
► FACEBOOK: https://www.facebook.com/TopTh....ings-108385027422972
► TWITTER: https://twitter.com/TopThings10
► YOUTUBE: https://www.youtube.com/channe....l/UCArcrGQYzJhB_IfEl
#funnyvideos #anesthesia #anesthesiareactions

External cephalic version is a process by which a breech baby can sometimes be turned from buttocks or foot first to head first. External cephalic version (ECV) is a manual procedure that is advocated by national guidelines for breech presentation singleton pregnancy, in order to enable vaginal delivery.

Are most spiders poisonous? The majority of the 3,000 spiders in the United States aren’t poisonous. Even if most spiders did bite, their fangs are too small or weak to puncture human skin. Their bites may leave itchy, red wounds that heal within a week or so. The spiders that do manage to bite through our skin and insert toxic venom can cause serious health complications. Read on to learn what spider bites look like, what spider varieties leave certain bites, and how to treat spider bites. What do spider bites look like? Identifying a spider bite is easier if you saw the spider that bit you, but it’s possible that you won’t notice the wound until hours later. Look for things like: swelling a red welt skin damage any troubling symptoms that accompany the bite Other possible symptoms that may accompany a spider bite include: itching or rash pain around the area of the bite muscle pain or cramping blister that’s red or purple in color sweating difficulty breathing headache nausea and vomiting fever chills anxiety or restlessness rashes swollen lymph glands high blood pressure Spider bites often take longer to heal than other insect bites, and they may affect skin tissues. It’s important to keep the bite clean to reduce the risk of infection. How to treat a spider bite at home In some cases, you can treat spider bites at home. For nonvenomous spider bites, follow these steps: Apply an ice pack on and off the bite for 10 minutes at a time. Elevate the area to reduce swelling. Take an antihistamine, such as diphenhydramine (Benadryl), to help with itching. Clean the area with soap and water to prevent infection. Apply antibiotic ointment to the area if blisters develop. Seek medical attention if you’re showing symptoms of a spider bite or if the symptoms don’t go away over time. Always seek medical attention if you suspect you’ve been bitten by one of the following species: brown recluse black widow hobo spider tarantula Brazilian wandering spider

In this video, we have explained the procedure of total #knee #replacement #surgery in patient in 3D animation.
Learn more: https://ecgkid.com
_____________________________________________________________________
Knee replacement, commonly known as complete knee replacement or knee arthroplasty, is a surgical treatment that resurfaces a knee that has been destroyed by arthritis. The extremities of the bones that make up the knee joint, as well as the kneecap, are capped with metal and plastic pieces. Someone with severe arthritis or a major knee injury may benefit from this procedure.
The knee joint can be affected by a variety of arthritis forms. The degradation of joint cartilage and neighboring bone in the knees can be caused by osteoarthritis, a degenerative joint disease that primarily affects middle-aged and older persons. Rheumatoid arthritis produces pain and stiffness by inflaming the synovial membrane and resulting in an excess of synovial fluid. Traumatic arthritis, or arthritis caused by an injury, can harm the joints.
The purpose of knee replacement surgery is to resurface damaged areas of the knee joint and cure knee discomfort that has not responded to prior therapies.