Top videos

This is a 60 year man having large swelling of size 7cm x 5 cm behind neck for one year. Patient complained pain and tenderness over local area for 7 days and came to us.On examination punctum found in the centre of swelling and fluctuation positive.Infected sebaceous cyst diagnosis made. Incision and drainage surgery done under local anesthesia.all infected pultaceous material evacuated.Pus culture sent and antibiotics given as per sensitivity report. Patient improved with daily dressing.
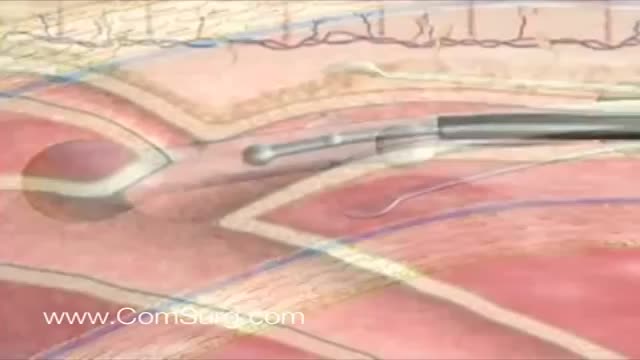
Like the VenaCure EVLT® procedure, which uses a laser to ablate the varicose vein, VNUS RF treatment is an alternative to more invasive leg stripping surgery. It is used primarily to treat the great saphenous veins (GSV), small saphenous vein (SSV), and other superficial veins in the legs.
Though the risk of HIV transmission through oral sex is very low, but several factors might increase the risk, including sores in the mouth or vagina or on the penis, bleeding gums, having an oral contact with menstrual blood, and the presence of other sexually transmitted diseases. But still the risk is low. by the way better to think twice before having the Oralsex with strangers. because you are not safe 100%.
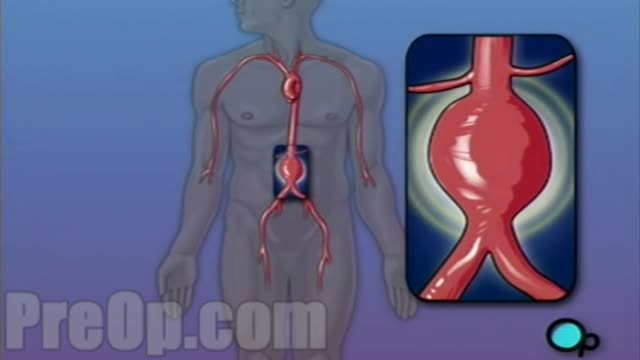
For this surgery, your doctor makes a large incision in the abdomen to expose the aorta. Once he or she has opened the abdomen, a graft can be used to repair the aneurysm. Open repair remains the standard procedure for an abdominal aortic aneurysm repair. Endovascular aneurysm repair (EVAR).
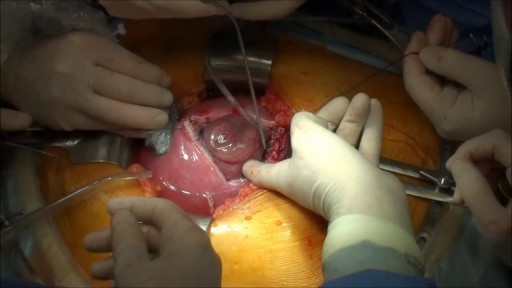
Prenatal repair of myelomeningocele (MMC), the most common and severe form of spina bifida, is a delicate surgical procedure where fetal surgeons open the uterus and close the opening in the baby's back while they are still in the womb.
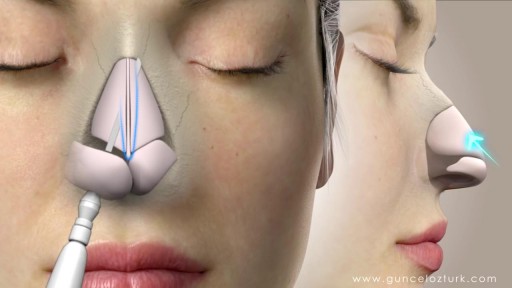
Rhinoplasty, sometimes referred to as a "nose job" or "nose reshaping" by patients, enhances facial harmony and the proportions of your nose. It can also correct impaired breathing caused by structural defects in the nose. What surgical rhinoplasty can treat Nose size in relation to facial balance Nose width at the bridge or in the size and position of the nostrils Nose profile with visible humps or depressions on the bridge Nasal tip that is enlarged or bulbous, drooping, upturned or hooked Nostrils that are large, wide or upturned Nasal asymmetry If you desire a more symmetrical nose, keep in mind that everyone's face is asymmetric to some degree. Results may not be completely symmetric, although the goal is to create facial balance and correct proportion. Rhinoplasty to correct a deviated septum Nose surgery that's done to improve an obstructed airway requires careful evaluation of the nasal structure as it relates to airflow and breathing. Correction of a deviated septum, one of the most common causes of breathing impairment, is achieved by adjusting the nasal structure to produce better alignment.

New flu vaccines are released every year to keep up with rapidly adapting flu viruses. Because flu viruses evolve so quickly, last year's vaccine may not protect you from this year's viruses. After vaccination, your immune system produces antibodies that will protect you from the vaccine viruses.

This video: Patent ductus arteriosus (PDA) is a persistent opening between two major blood vessels leading from the heart. The opening, called the ductus arteriosus, is a normal part of a baby's circulatory system before birth that usually closes shortly after birth. If it remains open, however, it's called a patent ductus arteriosus. A small patent ductus arteriosus often doesn't cause problems and might never need treatment. However, a large patent ductus arteriosus left untreated can allow poorly oxygenated blood to flow in the wrong direction, weakening the heart muscle and causing heart failure and other complications. Treatment options for a patent ductus arteriosus include monitoring, medications and closure by cardiac catheterization or surgery.