Top videos
Though the risk of HIV transmission through oral sex is very low, but several factors might increase the risk, including sores in the mouth or vagina or on the penis, bleeding gums, having an oral contact with menstrual blood, and the presence of other sexually transmitted diseases. But still the risk is low. by the way better to think twice before having the Oralsex with strangers. because you are not safe 100%.

Your body's immune system protects you from disease and infection. But if you have an autoimmune disease, your immune system attacks healthy cells in your body by mistake. Autoimmune diseases can affect many parts of the body. No one is sure what causes autoimmune diseases. They do tend to run in families. Women - particularly African-American, Hispanic-American, and Native-American women - have a higher risk for some autoimmune diseases. There are more than 80 types of autoimmune diseases, and some have similar symptoms. This makes it hard for your health care provider to know if you really have one of these diseases, and if so, which one. Getting a diagnosis can be frustrating and stressful. Often, the first symptoms are fatigue, muscle aches and a low fever. The classic sign of an autoimmune disease is inflammation, which can cause redness, heat, pain and swelling. The diseases may also have flare-ups, when they get worse, and remissions, when symptoms get better or disappear. Treatment depends on the disease, but in most cases one important goal is to reduce inflammation. Sometimes doctors prescribe corticosteroids or other drugs that reduce your immune response.
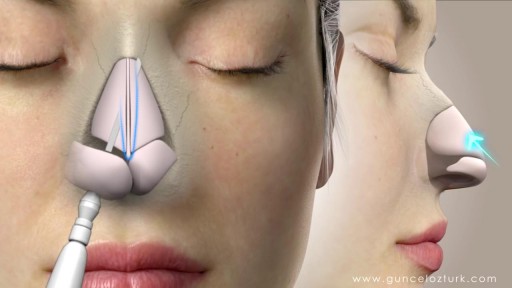
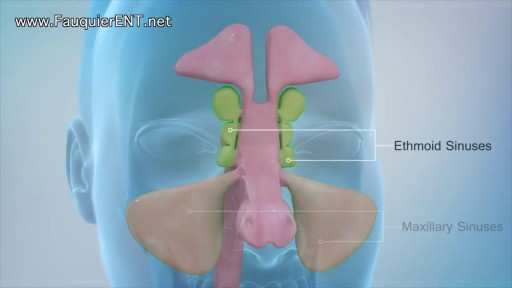
Rhinoplasty, sometimes referred to as a "nose job" or "nose reshaping" by patients, enhances facial harmony and the proportions of your nose. It can also correct impaired breathing caused by structural defects in the nose. What surgical rhinoplasty can treat Nose size in relation to facial balance Nose width at the bridge or in the size and position of the nostrils Nose profile with visible humps or depressions on the bridge Nasal tip that is enlarged or bulbous, drooping, upturned or hooked Nostrils that are large, wide or upturned Nasal asymmetry If you desire a more symmetrical nose, keep in mind that everyone's face is asymmetric to some degree. Results may not be completely symmetric, although the goal is to create facial balance and correct proportion. Rhinoplasty to correct a deviated septum Nose surgery that's done to improve an obstructed airway requires careful evaluation of the nasal structure as it relates to airflow and breathing. Correction of a deviated septum, one of the most common causes of breathing impairment, is achieved by adjusting the nasal structure to produce better alignment.
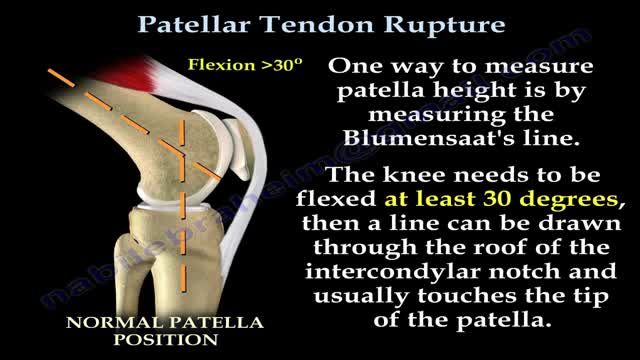
Patellar tendon rupture is a rupture of the tendon that connects the patella to the tibia. The superior portion of the patellar tendon attaches on the posterior portion of the patella, and the posterior portion of the patella tendon attaches to the tibial tubercle on the front of the tibia.

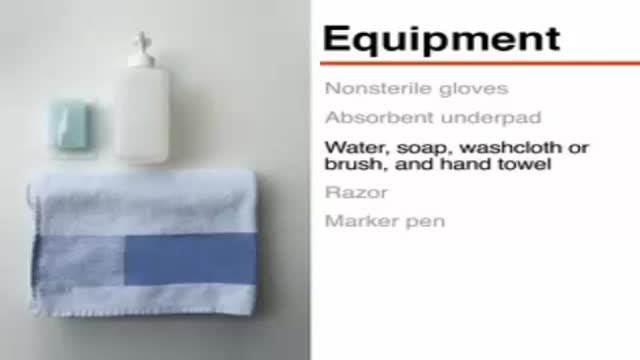
Leopold's Maneuvers are difficult to perform on obese women and women who have hydramnios. The palpation can sometimes be uncomfortable for the woman if care is not taken to ensure she is relaxed and adequately positioned. To aid in this, the health care provider should first ensure that the woman has recently emptied her bladder. If she has not, she may need to have a straight urinary catheter inserted to empy it if she is unable to micturate herself. The woman should lie on her back with her shoulders raised slightly on a pillow and her knees drawn up a little. Her abdomen should be uncovered, and most women appreciate it if the individual performing the maneuver warms their hands prior to palpation. First maneuver: Fundal Grip While facing the woman, palpate the woman's upper abdomen with both hands. A professional can often determine the size, consistency, shape, and mobility of the form that is felt. The fetal head is hard, firm, round, and moves independently of the trunk while the buttocks feel softer, are symmetric, and the shoulders and limbs have small bony processes; unlike the head, they move with the trunk. Second maneuver After the upper abdomen has been palpated and the form that is found is identified, the individual performing the maneuver attempts to determine the location of the fetal back. Still facing the woman, the health care provider palpates the abdomen with gentle but also deep pressure using the palm of the hands. First the right hand remains steady on one side of the abdomen while the left hand explores the right side of the woman's uterus. This is then repeated using the opposite side and hands. The fetal back will feel firm and smooth while fetal extremities (arms, legs, etc.) should feel like small irregularities and protrusions. The fetal back, once determined, should connect with the form found in the upper abdomen and also a mass in the maternal inlet, lower abdomen. Third maneuver: Pawlick's Grip In the third maneuver the health care provider attempts to determine what fetal part is lying above the inlet, or lower abdomen.[2] The individual performing the maneuver first grasps the lower portion of the abdomen just above the symphysis pubis with the thumb and fingers of the right hand. This maneuver should yield the opposite information and validate the findings of the first maneuver. If the woman enters labor, this is the part which will most likely come first in a vaginal birth. If it is the head and is not actively engaged in the birthing process, it may be gently pushed back and forth. The Pawlick's Grip, although still used by some obstetricians, is not recommended as it is more uncomfortable for the woman. Instead, a two-handed approach is favored by placing the fingers of both hands laterally on either side of the presenting part. Fourth maneuver The last maneuver requires that the health care provider face the woman's feet, as he or she will attempt to locate the fetus' brow. The fingers of both hands are moved gently down the sides of the uterus toward the pubis. The side where there is resistance to the descent of the fingers toward the pubis is greatest is where the brow is located. If the head of the fetus is well-flexed, it should be on the opposite side from the fetal back. If the fetal head is extended though, the occiput is instead felt and is located on the same side as the back. Cautions Leopold's maneuvers are intended to be performed by health care professionals, as they have received the training and instruction in how to perform them. That said, as long as care taken not to roughly or excessively disturb the fetus, there is no real reason it cannot be performed at home as an informational exercise. It is important to note that all findings are not truly diagnostic, and as such ultrasound is required to conclusively determine the fetal position.

Butt implants are a popular plastic surgery procedure among those who wish to enhance the appearance, shape, and size of their rear ends. Buttock augmentation involves the surgical insertion of artificial body implants into a patient’s buttocks to create a larger, shapelier, and more sensuous rear end. Patients who have underdeveloped buttocks can achieve a more proportionate figure with butt implants. Women who wish to achieve an “hour glass” figure or are unhappy with the size of their buttocks can benefit from female butt implants. Men with flat or poorly developed buttocks can enhance the shape of the area to their liking with male butt implants. Many buttock augmentation patients say that their clothes fit better, they feel more attractive, and their confidence levels have improved.
Invasive intracranial pressure monitoring. The most common surgically placed monitors for ICP measurement are intraventricular catheters (external ventricular drain [EVD] or a ventriculostomy drain) and fiberoptic ICP monitors implanted into the parenchyma of the brain.

Pancreatic cysts are saclike pockets of fluid on or in your pancreas, a large organ behind the stomach that produces hormones and enzymes that help digest food. Most pancreatic cysts aren't cancerous, and many don't cause symptoms. They're typically found during imaging testing for another problem. Some are actually noncancerous (benign) pockets of fluids lined with scar or inflammatory tissue, not the type of cells found in true cysts (pseudocysts). But some pancreatic cysts can be or can become cancerous. Your doctor might take a sample of the pancreatic cyst fluid to determine if cancer cells are present. Or your doctor might recommend monitoring a cyst over time for changes that indicate cancer.

What factors should I consider when deciding whether to have surgery? The following factors should be considered when deciding whether to have surgery: Your age—If you have surgery at a young age, there is a chance that prolapse will recur and may possibly require additional treatment. If you have surgery at an older age, general health issues and any prior surgery may affect the type of surgery that you have. Your childbearing plans—Ideally, women who plan to have children (or more children) should postpone surgery until their families are complete to avoid the risk of prolapse happening again after corrective surgery. Health conditions—Any surgical procedure carries some risk, such as infection, bleeding, blood clots in the legs, and problems related to anesthesia. Surgery may carry more risks if you have a medical condition, such as diabetes, heart disease, or breathing problems, or if you smoke or are obese. New problems—Surgery also may cause new problems, such as pain during sex, pelvic pain, or urinary incontinence.

Mastitis is inflammation of tissue in one or both mammary glands inside the breast. Mastitis usually affects lactating women - women who are breastfeeding, producing milk. Hence, it is often referred to as lactation mastitis. The patient feels a hard, sore spot inside the breast.

When diving into a Breast Reduction procedure, there are many things to consider. Even as a patient, being aware of any concerns and how the procedure works is important. Therefore, when a plastic surgeon operates on a patient, the results are clear. Dr. Linder, a Breast surgeon specialist in Beverly Hills, helps explain what goes into a Breast Reduction Procedure.
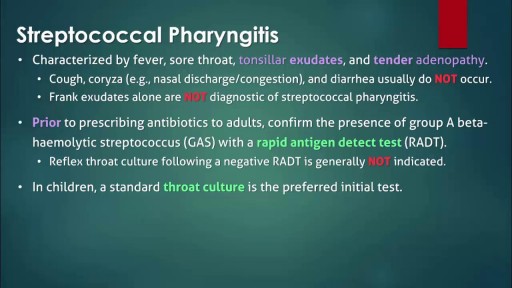
The infection is generally transmitted by direct contact with the mucus or sores of someone else with strep. Common symptoms include sore throat, fever, and swollen lymph nodes in the neck. Rarely, complications can involve the heart or kidneys. Treatment is important to reduce complications. Oral antibiotics like penicillin, amoxicillin, cephalexin, or azithromycin are commonly used. Other medicines such as acetaminophen or ibuprofen can help with pain and fever.

A man set to become the world’s first head transplant patient has scheduled the procedure for December 2017. Valery Spiridonov, 30, was diagnosed with a genetic muscle-wasting condition called Werdnig-Hoffmann disease, and volunteered for the procedure despite the risks involved, Central European News (CEN) reported. “When I realized that I could participate in something really big and important, I had no doubt left in my mind and started to work in this direction,” Spiridonov, a Russian computer scientist, told CEN. “The only thing I feel is the sense of pleasant impatience, like I have been preparing for something important all my life and it is starting to happen.”