Top videos
There are several reasons that your doctor may recommend that you have your spleen removed. These include having: a spleen that’s damaged from injury an enlarged spleen or ruptured spleen, which can occur from trauma certain rare blood disorders cancer or large cysts of the spleen infection

Skin cancer is the most common type of cancer. There are three major types of skin cancer — Basal Cell Carcinoma, Squamous Cell Carcinoma and melanoma. Out of these, Melanoma is the deadliest form of skin cancer. Melanoma appears on the skin as a new spot or growth or a change in an already existing mole. It is often fast growing and can spread to other parts of your body, including your bones, liver, and lungs to form a new cancer.

Can Birth Control Be a Dysmenorrhea Treatment? || Common gynaecological problems in women Dysmenorrhea is the medical term used for when you have painful menstrual cramps that occur immediately before or during your period. The pain can be so bad that it limits your daily activities. Dysmenorrhea is the most commonly reported menstrual disorder. It can affect up to 90 percent of young women. The Pill (as well as other hormonal contraceptives) can help in the treatment of dysmenorrhea.
A young patient undergoes state of the art robotic surgery for Ovarian Cancer and Endometrial Cancer in Chicago, IL. The surgery is performed by noted gynecologic oncologist and expert robotic surgeon M. Patrick Lowe MD. Dr Lowe has been performing robotic surgery since 2006 and is one of a few gynecologic oncologist in the United States who utilizes robotics for ovarian cancer.

A breech birth is the birth of a baby from a breech presentation. In the breech presentation the baby enters the birth canal with the buttocks or feet first as opposed to the normal head first presentation.
There are either three or four main categories of breech births, depending upon the source:
* Frank breech - the baby's bottom comes first, and his or her legs are flexed at the hip and extended at the knees (with feet near the ears). 65-70% of breech babies are in the frank breech position.
* Complete breech - the baby's hips and knees are flexed so that the baby is sitting crosslegged, with feet beside the bottom.
* Footling breech - one or both feet come first, with the bottom at a higher position. This is rare at term but relatively common with premature fetuses.
* Kneeling breech - the baby is in a kneeling position, with one or both legs extended at the hips and flexed at the knees. This is extremely rare, and is excluded from many classifications.
As in labour with a baby in a normal head-down position, uterine contractions typically occur at regular intervals and gradually cause the cervix to become thinner and to open. In the more common breech presentations, the baby’s bottom (rather than feet or knees) is what is first to descend through the maternal pelvis and emerge from the vagina.
At the beginning of labour, the baby is generally in an oblique position, facing either the right or left side of the mother's back. As the baby's bottom is the same size in the term baby as the baby's head. Descent is thus as for the presenting fetal head and delay in descent is a cardinal sign of possible problems with the delivery of the head.
In order to begin the birth, internal rotation needs to occur. This happens when the mother's pelvic floor muscles cause the baby to turn so that it can be born with one hip directly in front of the other. At this point the baby is facing one of the mother's inner thighs. Then, the shoulders follow the same path as the hips did. At this time the baby usually turns to face the mother's back. Next occurs external rotation, which is when the shoulders emerge as the baby’s head enters the maternal pelvis. The combination of maternal muscle tone and uterine contractions cause the baby’s head to flex, chin to chest. Then the back of the baby's head emerges and finally the face.
Due to the increased pressure during labour and birth, it is normal for the baby's leading hip to be bruised and genitalia to be swollen. Babies who assumed the frank breech position in utero may continue to hold their legs in this position for some days after birth.
mply put, relapses, also known as flare ups, or (MS) attacks are new or worsening MS symptoms. But there is a concrete definition used by healthcare providers to identify MS attacks. To be considered an MS relapse: Old symptoms of MS must have become worse or new symptoms appeared.
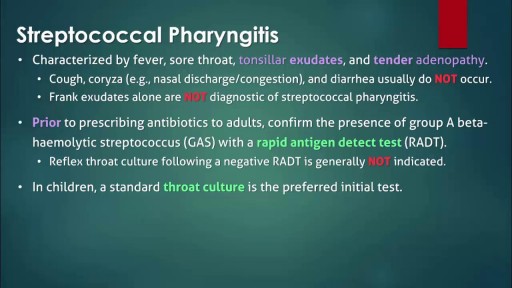
The infection is generally transmitted by direct contact with the mucus or sores of someone else with strep. Common symptoms include sore throat, fever, and swollen lymph nodes in the neck. Rarely, complications can involve the heart or kidneys. Treatment is important to reduce complications. Oral antibiotics like penicillin, amoxicillin, cephalexin, or azithromycin are commonly used. Other medicines such as acetaminophen or ibuprofen can help with pain and fever.
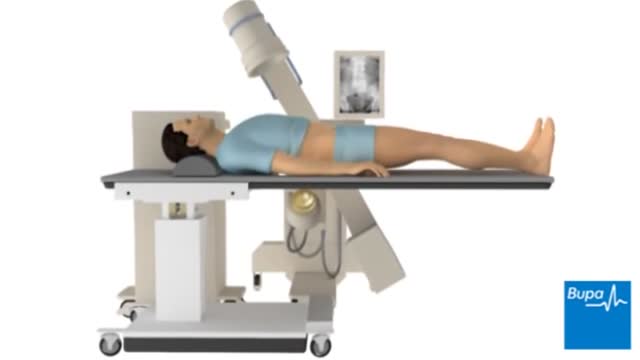
Extracorporeal shock wave lithotripsy (ESWL) uses shock waves to break a kidney stone into small pieces that can more easily travel through the urinary tract camera.gif and pass from the body. See a picture of ESWL camera.gif. You lie on a water-filled cushion, and the surgeon uses X-rays or ultrasound tests to precisely locate the stone. High-energy sound waves pass through your body without injuring it and break the stone into small pieces. These small pieces move through the urinary tract and out of the body more easily than a large stone. The process takes about an hour. You may receive sedatives or local anesthesia. Your surgeon may use a stent if you have a large stone. A stent is a small, short tube of flexible plastic mesh that holds the ureter open. This helps the small stone pieces to pass without blocking the ureter.

Dr. David Rivadeneira from Stony Brook University in Stony Brook, NY will host a panel discussion on how to obtain improved outcomes during open surgery through the application of advanced techniques and technologies, including the new LigaSure Impact™ instrument. "It provides excellent and reliable hemostasis on major blood vessels, but the big advancement is that it is faster than traditional techniques and leaves no foreign material behind."
The program will begin with a brief introduction of the topic, followed by video presentation of two procedures, a right hemicolectomy and a sigmoid colectomy. Dr. Rivadeneira will discuss the techniques that he uses. "You'll be able to see the impact of applying multifunctional energy-based instruments to enable rapid and reliable dissection of the mesentery and ligation of colonic blood supply. This is particularly evident on tough diverticular cases, where it works very well with complicated tissue." Joining Dr. Rivadeneira, to review and discuss the cases, will be Dr. Sang Lee from Weill Cornell Medical College, NY.

Trigeminal neuralgia is a chronic pain condition that affects the trigeminal nerve, which carries sensation from your face to your brain. If you have trigeminal neuralgia, even mild stimulation of your face — such as from brushing your teeth or putting on makeup — may trigger a jolt of excruciating pain. You may initially experience short, mild attacks. But trigeminal neuralgia can progress and cause longer, more-frequent bouts of searing pain. Trigeminal neuralgia affects women more often than men, and it's more likely to occur in people who are older than 50. Because of the variety of treatment options available, having trigeminal neuralgia doesn't necessarily mean you're doomed to a life of pain. Doctors usually can effectively manage trigeminal neuralgia with medications, injections or surgery.
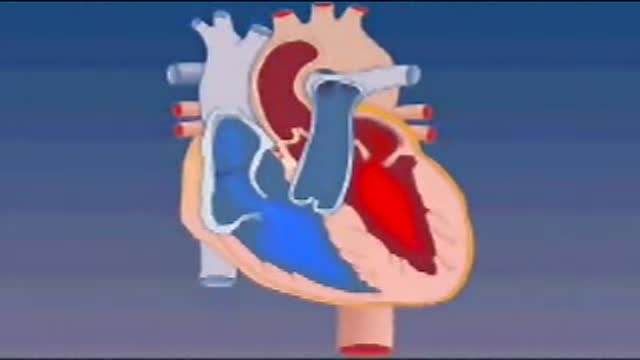
Blood enters the heart through two large veins, the inferior and superior vena cava, emptying oxygen-poor blood from the body into the right atrium. As the atrium contracts, blood flows from your right atrium into your right ventricle through the open tricuspid valve.

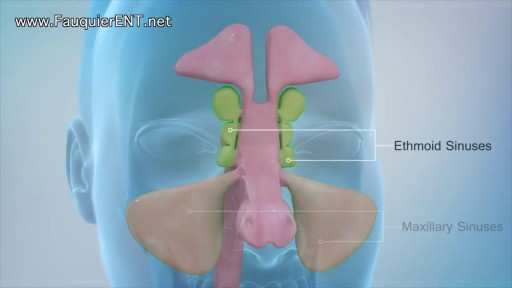
Nasal polyps are linked to allergic rhinitis, asthma, aspirin allergy, sinus infections, acute and chronic infections, something stuck in the nose, and cystic fibrosis. But many times the cause is unknown. Sometimes, people get them before they develop asthma or sinusitis