Top videos

UPDATE 1/30/15: Watch the updated version of this animation: https://www.youtube.com/watch?v=LVP6JngpgEE
This 3D medical animation shows how adhesions in the abdomen may cause complications. These problems may include obstruction, twisting, and dislocating areas of the small intestine. Adhesions can be separated with laparoscopic instruments.
ANH00037

Tourette syndrome (also called Tourette's disorder or simply, "Tourette's") is an abnormal neurological condition characterized by motor and vocal tics. Tics are involuntary, rapid, sudden repetitive movements or sounds. Tics can be classified in a variety of ways. Motor tics can affect any part of the body including the head, neck, face, arms, shoulders, hands, feet, or legs. Facial tics, especially eye blinking, are usually the first symptoms of TS. Vocal tics are sounds that are made involuntarily. Vocal tics can include clearing the throat, coughing, sniffing, grunting, yelping, or shouting. In a few cases, vocal tics can include strange, inappropriate, or obscene words and phrases (called coprolalia). Vocal tics can also appear as constantly repeating the words of others (echolalia).
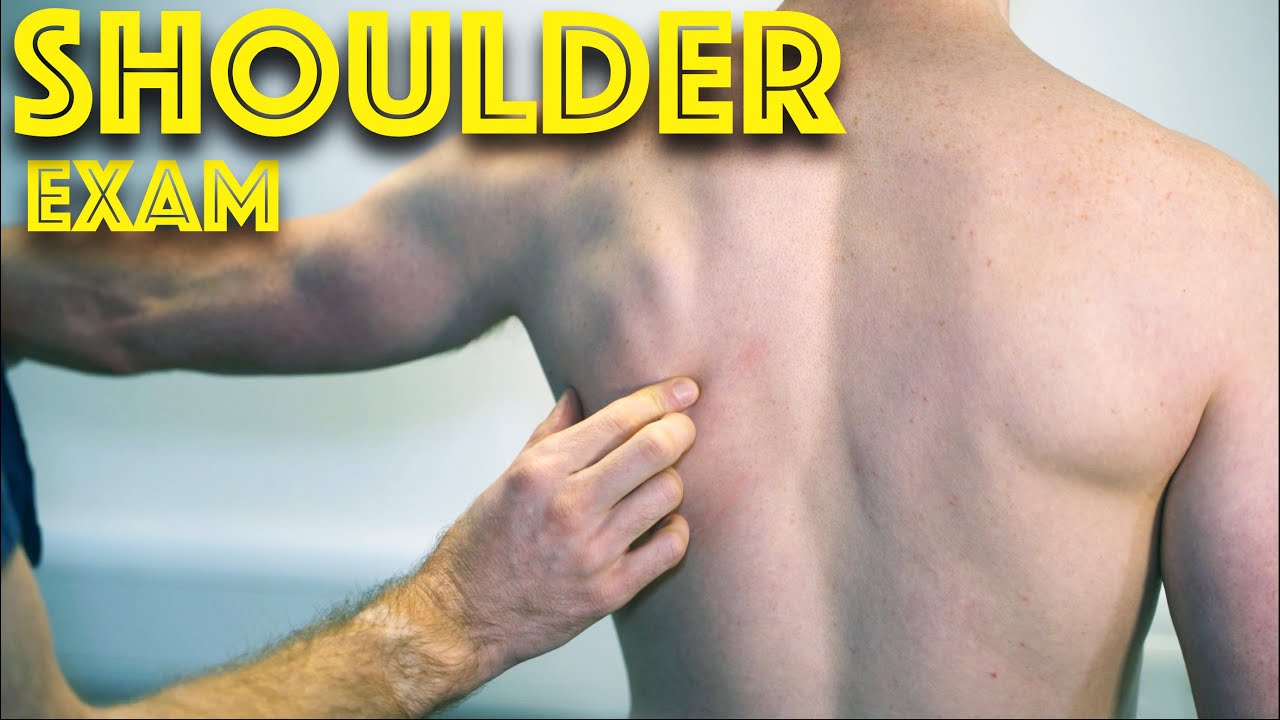
Shoulder Clinical Examination - Medical School Clinical Skills - Dr Gill
Personally, I find the shoulder examination the most complex examination possibly as there are so many variations and special tests. Some of which overlap and some will relate specifically to a patients presentation.
Often in a medical school syllabus, only select special tests will be used. In this shoulder exam demonstration, we include the Hawkins-Kennedy Test looking for impingement. This is dovetailed with examination for bicipital tendonitis as this is another possible cause of impingement type symptoms.
This shoulder upper limb exam follows the standard "Look, Feel, Move" orthopaedic exam approach, and overall order as set out in MacLeods Clinical Examination
Watch further orthopaedic examinations for your OSCE revision:
The Spine Examination:
https://youtu.be/pJxMHa6SCgU
Knee Examination
https://youtu.be/oyKH4EYfJDM
Hip Joint Clinical Examination
https://youtu.be/JC9GKq5nSdQ
________
Please note that there is no ABSOLUTE way to perform a clinical examination. Different institutions and even clinicians will have differing degrees of variations - the aim is the effectively identify medically relevant signs.
However during OSCE assessments. Different medical schools, nursing colleges, and other health professional courses will have their own preferred approach to a clinical assessment - you should concentrate on THEIR marks schemes for your assessments.
The examination demonstrated here is derived from Macleods Clinical Examination - a recognized standard textbook for clinical skills.
#ShoulderExamination #ClinicalSkills #DrGill
Bone marrow examination refers to the pathologic analysis of samples of bone marrow obtained by bone marrow biopsy (often called a trephine biopsy) and bone marrow aspiration. Bone marrow examination is used in the diagnosis of a number of conditions, including leukemia, multiple myeloma, anemia, and pancytopenia. The bone marrow produces the cellular elements of the blood, including platelets, red blood cells and white blood cells. While much information can be gleaned by testing the blood itself (drawn from a vein by phlebotomy), it is sometimes necessary to examine the source of the blood cells in the bone marrow to obtain more information on hematopoiesis; this is the role of bone marrow aspiration and biopsy.

If you are tired of dealing with glasses or squinting to read signs in the distance, then you should consider LASIK Eye Surgery. In this outpatient refractive procedure, lasers are used to correct vision issues by changing the structure of the cornea. This may entirely eliminate reliance upon glasses or contacts. In this interactive LASIK Eye Surgery, you will assist in numbing the patient’s eye and cleaning the area for the procedure. With a speculum, you will hold the eye open, mark the cornea using a water-soluble ink, then attach a suction ring to it. After that, a specialized blade device is used to cut into the corneal flap and peel it back so that the laser can clear away corneal tissue underneath. This process corrects the shape of the cornea in less than a minute before putting the corneal flap back in place. After the procedure, we will go over LASIK Eye Surgery recovery instructions. Scrub in and let’s get started!

35 year old women with breathing difficulties for 6 months and feels like fluid is leaking down her front and back. Pain in thorax, lower back and pelvic. Weight loss. Was exposed to mold for a 2 years. Has a dog witch has persistent worm infection. Also been traveling out of the country.

Macrobiopsy of breast lesions is a complicated procedure when performed with vacuum assisted biopsy tools. The Spirotome is a hand-held needle set that doesn't need capital investment, is ready to use and provides tissue samples of high quality in substantial amounts. In this way quantitative molecular biology is possible with one tissue sample. The Coramate is an automated version of this direct and frontal technology.
Today on Crash Course Anatomy & Physiology, Hank breaks down the parts and functions of one of your body's unsung heroes: your epithelial tissue.
Pssst... we made flashcards to help you review the content in this episode! Find them on the free Crash Course App!
Download it here for Apple Devices: https://apple.co/3d4eyZo
Download it here for Android Devices: https://bit.ly/2SrDulJ
Chapters:
Introduction 00:00
Proper Epithelium & Glandular Epithelium 1:38
We're All Just Tubes! 2:12
Cell Shapes: Squamous, Cuboidal, or Columnar 3:34
How Form Relates to Function 4:15
Layering: Simple or Stratified 5:26
Epithelial Cells: Apical & Basal Sides 7:06
Glandular Epithelial Tissue Forms Endocrine & Exocrine Glands 8:20
Review 9:16
Credits 9:54
***
Crash Course is on Patreon! You can support us directly by signing up at http://www.patreon.com/crashcourse
Want to find Crash Course elsewhere on the internet?
Facebook - http://www.facebook.com/YouTubeCrashCourse
Twitter - http://www.twitter.com/TheCrashCourse
Instagram - https://www.instagram.com/thecrashcourse/
CC Kids: http://www.youtube.com/crashcoursekids
Describe pre-procedure considerations for administering a subcutaneous injection.
Describe and demonstrate the preparation for administering a subcutaneous injection.
Describe and demonstrate needle and blood safety.
Describe and demonstrate suitable injection sites for subcutaneous injections.
Discuss the appropriate needle and syringe sizes for subcutaneous injection.
Describe and demonstrate the preparation of the substance to be injected.
Describe and demonstrate safe and correct administration of a subcutaneous injection.
Understand and apply Occupational Safety and Health Administration (OSHA) guidelines.
Understand and apply drug administration safety guidelines (seven rights).
Understand correct post-procedure considerations.
Describe and demonstrate correct documentation.
Define and demonstrate correct recording and reporting procedures.
Define and use related medical terminology.
Explain the Patient Privacy Rule (HIPAA), Patient Safety Act, and Patients' Bill of Rights.
www.simtics.com