Top videos
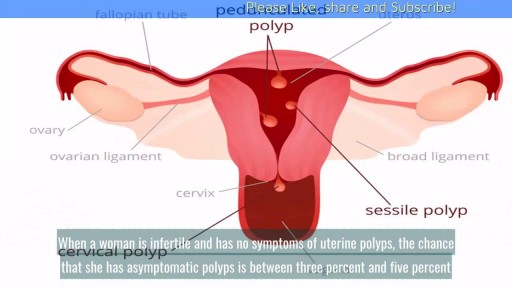
Uterine polyps, also called endometrial polyps, are usually small, bulb-shaped masses of endometrial tissue attached to the uterus by a stalk. They are soft, as opposed to uterine fibroids, which can grow much bigger and are made of hard muscle.
mply put, relapses, also known as flare ups, or (MS) attacks are new or worsening MS symptoms. But there is a concrete definition used by healthcare providers to identify MS attacks. To be considered an MS relapse: Old symptoms of MS must have become worse or new symptoms appeared.
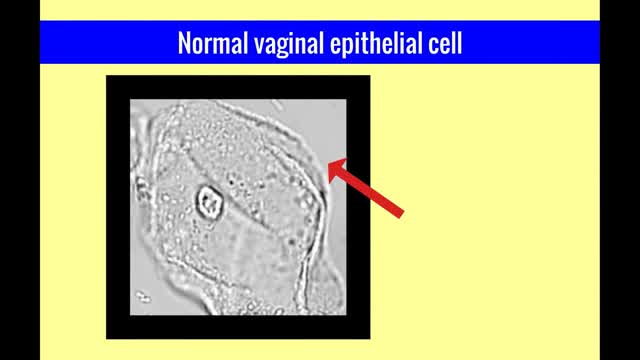
The vulvar vaginal diseases service sees referrals to help women with short--and long--term problems of the outer genital area (vulva), vagina and pelvic floor muscles including: Vulvar vaginal burning, itching, irritation and pain Vulvar Vestibulitis Pain with intercourse Discharge Yeast infections Bacterial vaginosis Pelvic floor muscle dysfunction A patient must be referred by her local health care provider. Services include: Skin care education Examinations-Your healthcare provider will examine you and talk with you about recommendations for treatment and/or management of your symptoms. Some vulvar diseases require a biopsy to diagnose the condition. Referrals-Your healthcare team may refer you to other specialists, including physical therapists or health psychologists. Separate insurance authorization is necessary for these services. The clinic staff provides general education and support to help women cope with these very personal health problems. Following a clinic visit, a letter is promptly sent to your local health care provider. The letter provides the results of your exam and the plan of care.

Trigeminal neuralgia is a chronic pain condition that affects the trigeminal nerve, which carries sensation from your face to your brain. If you have trigeminal neuralgia, even mild stimulation of your face — such as from brushing your teeth or putting on makeup — may trigger a jolt of excruciating pain. You may initially experience short, mild attacks. But trigeminal neuralgia can progress and cause longer, more-frequent bouts of searing pain. Trigeminal neuralgia affects women more often than men, and it's more likely to occur in people who are older than 50. Because of the variety of treatment options available, having trigeminal neuralgia doesn't necessarily mean you're doomed to a life of pain. Doctors usually can effectively manage trigeminal neuralgia with medications, injections or surgery.

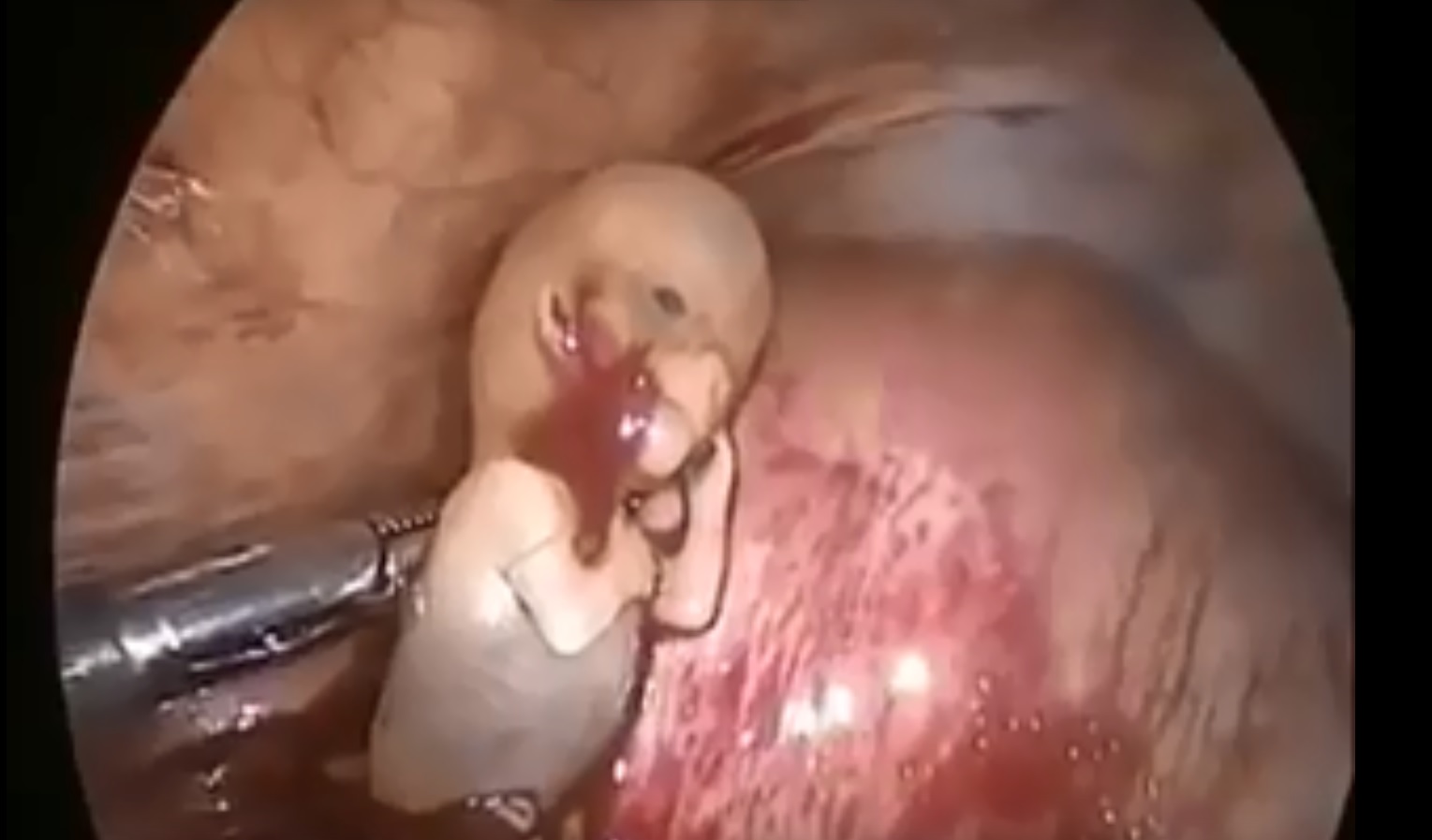
Dr. David Rivadeneira from Stony Brook University in Stony Brook, NY will host a panel discussion on how to obtain improved outcomes during open surgery through the application of advanced techniques and technologies, including the new LigaSure Impact™ instrument. "It provides excellent and reliable hemostasis on major blood vessels, but the big advancement is that it is faster than traditional techniques and leaves no foreign material behind."
The program will begin with a brief introduction of the topic, followed by video presentation of two procedures, a right hemicolectomy and a sigmoid colectomy. Dr. Rivadeneira will discuss the techniques that he uses. "You'll be able to see the impact of applying multifunctional energy-based instruments to enable rapid and reliable dissection of the mesentery and ligation of colonic blood supply. This is particularly evident on tough diverticular cases, where it works very well with complicated tissue." Joining Dr. Rivadeneira, to review and discuss the cases, will be Dr. Sang Lee from Weill Cornell Medical College, NY.
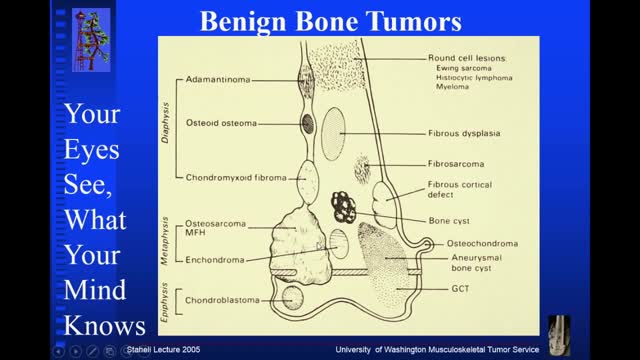
Osteochondroma. Osteochondromas (osteocartilaginous exostoses), the most common benign bone tumors, may arise from any bone but tend to occur near the ends of long bones. ... Enchondroma. ... Chondroblastoma. ... Chondromyxofibroma. ... Osteoid osteoma. ... Nonossifying fibroma (fibrous cortical defect) ... Benign giant cell tumor of bone.

Rhinoplasty enhances facial harmony and the proportions of your nose. It can also correct impaired breathing caused by structural defects in the nose. Rhinoplasty surgery can change: Nose size in relation to facial balance Nose width at the bridge or in the size and position of the nostrils Nose profile with visible humps or depressions on the bridge Nasal tip that is enlarged or bulbous, drooping, upturned or hooked Nostrils that are large, wide, or upturned Nasal asymmetry If you desire a more symmetrical nose, keep in mind that everyone’s face is asymmetric to some degree. Results may not be completely symmetric, although the goal is to create facial balance and correct proportion.

Wisdom teeth extractions can rear their ugly head later in life. This is a video of a patient with neck pain and neck weakness. When we stimulated the nerve fibers in the area of the extracted teeth there was an immediate improvement in her ability to control her neck muscles.
symptoms of kidney dysfunction. I find kidney dysfunction in my patients very frequently. Lower back pain is a common indicator that the kidneys are starting to become irritated. Yes, lower back pain can come from many different areas, but one of the areas I always rule out is kidney congestion.