Top videos

Care for Your Knee After Knee Replacement Surgery
In this video, Dr. Mark Hammerberg, provides details on two important activities to help during recovery from knee replacement surgery.
Denver Health's Orthopedics department offers many different types of treatments to help you, including surgical and non-surgical options. To find out if surgery is right for you, visit DenverHealth.org/Orthopedics or call 303-602-1590 to make an appointment.

Macrobiopsy of breast lesions is a complicated procedure when performed with vacuum assisted biopsy tools. The Spirotome is a hand-held needle set that doesn't need capital investment, is ready to use and provides tissue samples of high quality in substantial amounts. In this way quantitative molecular biology is possible with one tissue sample. The Coramate is an automated version of this direct and frontal technology.
Bone marrow examination refers to the pathologic analysis of samples of bone marrow obtained by bone marrow biopsy (often called a trephine biopsy) and bone marrow aspiration. Bone marrow examination is used in the diagnosis of a number of conditions, including leukemia, multiple myeloma, anemia, and pancytopenia. The bone marrow produces the cellular elements of the blood, including platelets, red blood cells and white blood cells. While much information can be gleaned by testing the blood itself (drawn from a vein by phlebotomy), it is sometimes necessary to examine the source of the blood cells in the bone marrow to obtain more information on hematopoiesis; this is the role of bone marrow aspiration and biopsy.

Giant cell arteritis is an inflammation of the lining of your arteries. Most often, it affects the arteries in your head, especially those in your temples. For this reason, giant cell arteritis is sometimes called temporal arteritis. Giant cell arteritis frequently causes headaches, scalp tenderness, jaw pain and vision problems. If left untreated, it can lead to stroke or blindness. Prompt treatment with corticosteroid medications usually relieves symptoms of giant cell arteritis and may prevent loss of vision. You'll likely begin to feel better within days of starting treatment. But even with treatment, relapses are common. You'll need to visit your doctor regularly for checkups and treatment of any side effects from taking corticosteroids.

Tourette syndrome (also called Tourette's disorder or simply, "Tourette's") is an abnormal neurological condition characterized by motor and vocal tics. Tics are involuntary, rapid, sudden repetitive movements or sounds. Tics can be classified in a variety of ways. Motor tics can affect any part of the body including the head, neck, face, arms, shoulders, hands, feet, or legs. Facial tics, especially eye blinking, are usually the first symptoms of TS. Vocal tics are sounds that are made involuntarily. Vocal tics can include clearing the throat, coughing, sniffing, grunting, yelping, or shouting. In a few cases, vocal tics can include strange, inappropriate, or obscene words and phrases (called coprolalia). Vocal tics can also appear as constantly repeating the words of others (echolalia).

UPDATE 1/30/15: Watch the updated version of this animation: https://www.youtube.com/watch?v=LVP6JngpgEE
This 3D medical animation shows how adhesions in the abdomen may cause complications. These problems may include obstruction, twisting, and dislocating areas of the small intestine. Adhesions can be separated with laparoscopic instruments.
ANH00037
Shoulder Clinical Examination - Medical School Clinical Skills - Dr Gill
Personally, I find the shoulder examination the most complex examination possibly as there are so many variations and special tests. Some of which overlap and some will relate specifically to a patients presentation.
Often in a medical school syllabus, only select special tests will be used. In this shoulder exam demonstration, we include the Hawkins-Kennedy Test looking for impingement. This is dovetailed with examination for bicipital tendonitis as this is another possible cause of impingement type symptoms.
This shoulder upper limb exam follows the standard "Look, Feel, Move" orthopaedic exam approach, and overall order as set out in MacLeods Clinical Examination
Watch further orthopaedic examinations for your OSCE revision:
The Spine Examination:
https://youtu.be/pJxMHa6SCgU
Knee Examination
https://youtu.be/oyKH4EYfJDM
Hip Joint Clinical Examination
https://youtu.be/JC9GKq5nSdQ
________
Please note that there is no ABSOLUTE way to perform a clinical examination. Different institutions and even clinicians will have differing degrees of variations - the aim is the effectively identify medically relevant signs.
However during OSCE assessments. Different medical schools, nursing colleges, and other health professional courses will have their own preferred approach to a clinical assessment - you should concentrate on THEIR marks schemes for your assessments.
The examination demonstrated here is derived from Macleods Clinical Examination - a recognized standard textbook for clinical skills.
#ShoulderExamination #ClinicalSkills #DrGill

35 year old women with breathing difficulties for 6 months and feels like fluid is leaking down her front and back. Pain in thorax, lower back and pelvic. Weight loss. Was exposed to mold for a 2 years. Has a dog witch has persistent worm infection. Also been traveling out of the country.

Pinch air out of the tip of the condom. Unroll condom all the way down the penis. After sex but before pulling out, hold the condom at the base. Then pull out, while holding the condom in place. Carefully remove the condom and throw it in the trash.

The OrthoIllustrated® animation for total knee replacement is an educational tool to help patients better understand the diagnosis and treatment of arthritis.
- - - - -
Why Work Arthrex https://www.arthrex.com/job-seeker
Find an Arthrex Surgeon: https://doctorfinder.orthoillustrated.com
- - - - -
Join the Community:
LinkedIn: https://www.linkedin.com/company/arthrex
Facebook: https://www.facebook.com/Arthrex
Instagram: https://www.instagram.com/arthrex_inc/
Twitter: https://twitter.com/Arthrex
TikTok: https://www.tiktok.com/@arthrex
- - - - -
Arthrex Inc., headquartered in Naples, Florida, is a global leader in orthopedic surgical device design, research, manufacturing, and medical education. Arthrex develops and releases more than 1,000 new products and procedures every year to advance minimally invasive orthopedics worldwide.
For more information, visit https://www.arthrex.com
- - - - -
OrthoPedia is an innovative educational website that was created for anyone interested in learning about orthopedics from the first-year student to the experienced orthopedic surgeon.
Visit https://www.orthopedia.com to experience the future of Medical Education.

nee joint aspiration and injection are performed to aid in diagnosis and treatment of knee joint diseases. The knee joint is the most common and the easiest joint for the physician to aspirate. One approach involves insertion of a needle 1 cm above and 1 cm lateral to the superior lateral aspect of the patella at a 45-degree angle. Once the needle has been inserted 1 to 1½ inches, aspiration aided by local compression is performed. Local corticosteroid injections can provide significant relief and often ameliorate acute exacerbations of knee osteoarthritis associated with significant effusions. Among the indications for arthrocentesis are crystal-induced arthropathy, hemarthrosis, unexplained joint effusion, and symptomatic relief of a large effusion. Contraindications include bacteremia, inaccessible joints, joint prosthesis, and overlying infection in the soft tissue. Large effusions can recur and may require repeat aspiration. Anti-inflammatory medi
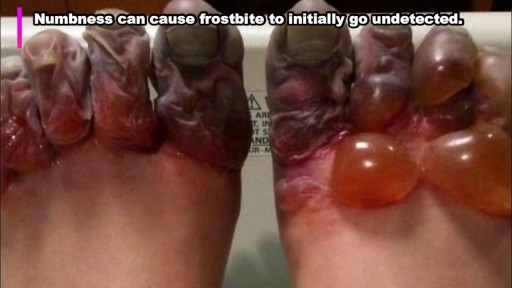
rostbite refers to the freezing of body tissue (usually skin) that results when the blood vessels contract, reducing blood flow and oxygen to the affected body parts. Normal sensation is lost, and color changes also occur in these tissues.