Top videos

-Tibial stress fractures are common in athletes and nonathletes who suddenly increase their physical activity. Clinical features include pain, localized tenderness, and swelling. Plain x-ray is <50% sensitive for stress fractures, especially in the first 2-3 weeks after the onset of symptoms. MRI is preferred over bone scan or ultrasound as it can show the fracture line that extends through the cortex into the medullary line. MRI can also identify ligament, muscle, and cartilage injuries. However, MRI findings may be persistently abnormal for up to 1 year after the stress fracture has healed.

Macrobiopsy of breast lesions is a complicated procedure when performed with vacuum assisted biopsy tools. The Spirotome is a hand-held needle set that doesn't need capital investment, is ready to use and provides tissue samples of high quality in substantial amounts. In this way quantitative molecular biology is possible with one tissue sample. The Coramate is an automated version of this direct and frontal technology.

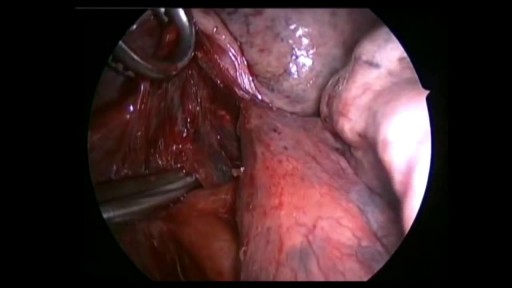
Doctor Ricky Brown reacts to this surgery simulation of an inguinal hernia repair where they repair the hernia sack and create a mesh for the organ to comfortably rest on.
3D Animation powered by:
3DMedWorld - 3dmedworld.com
#shorts #doctor #education #surgery #medical
If you have a lung disease, a type of surgery called a lobectomy is one treatment option your doctor may suggest. Your lungs are made up of five sections called lobes. You have three in your right lung and two in your left. A lobectomy removes one of these lobes. After the surgery, your healthy tissue makes up for the missing section, so your lungs should work as well or better than they did before.
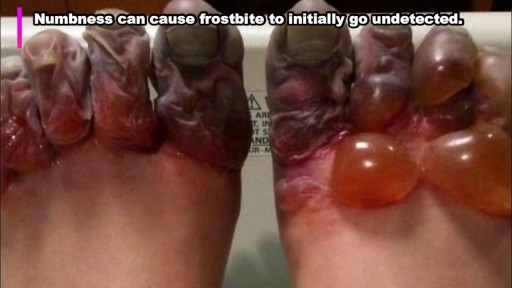
rostbite refers to the freezing of body tissue (usually skin) that results when the blood vessels contract, reducing blood flow and oxygen to the affected body parts. Normal sensation is lost, and color changes also occur in these tissues.