Top videos
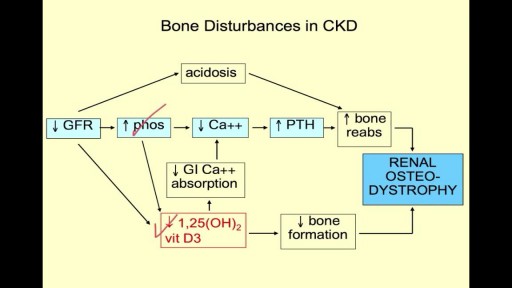
symptoms of kidney dysfunction. I find kidney dysfunction in my patients very frequently. Lower back pain is a common indicator that the kidneys are starting to become irritated. Yes, lower back pain can come from many different areas, but one of the areas I always rule out is kidney congestion.
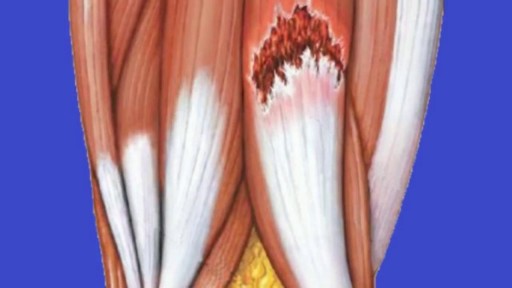
Pain in the upper thigh can be difficult to diagnose because this area of the body contains many muscles, tendons, and ligaments. This kind of pain may often be due to minor muscle injuries that are treatable at home. When the pain is intense or does not go away, however, it may signal a more serious problem. In this video, we examine some common causes of pain in the upper thigh, along with any symptoms that may occur alongside. We also take a look at the treatment options and how to prevent this type of pain.
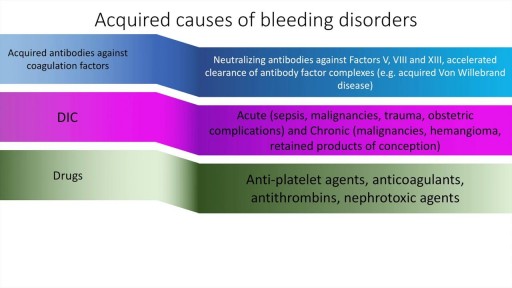
A detailed description of the approach to a use of bleeding disorders. This presentation includes the causes, history, clinical features and diagnosis of specific bleeding disorders. These include Haemophilia, DIC, Von Willebrand Disease and others. The final differentiation is often made on the basis of the Prothrombin Time, activated Partial thromboplastin time and platelet count.
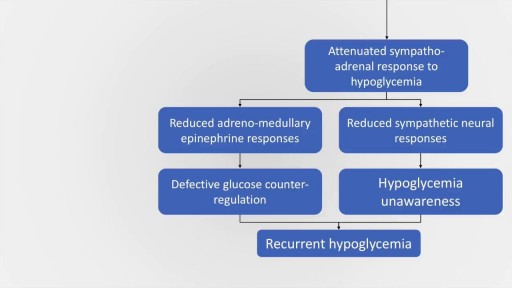
Hypoglycemia is a common and serious medical emergency which may occur in both daibetic and non-diabetic patients. The signs and symptoms of hypoglycaemia may be present in many individuals, but may also be masked in several individuals due to a condition called hypoglycaemia induced autonomic failure. This presentation aims to deal with the causes, clinical features, diagnosis and management of various causes of hypoglycaemia. The causes of hypoglycaemia may be divided into hypoglycaemia in ill or medicated individuals and hypoglycaemia in previously asymptomatic individuals. A variety of causes are discussed under both headings. Management of hypoglycaemia is also discussed in detail. There is also a brief discussion about management of insulinoma.

Rhabdomyolysis is a condition in which damaged skeletal muscle (Ancient Greek: rhabdomyo-) tissue breaks down rapidly (Greek –lysis). This damage may be caused by physical (e.g. crush injury), chemical, or biological factors. Breakdown products of damaged muscle cells are released into the bloodstream; some of these, such as the protein myoglobin, are harmful to the kidney and may lead to kidney dysfunction. The severity of the symptoms (which may include muscle pains, vomiting and confusion) depends on the extent of the muscle damage, and whether kidney failure develops. The mainstay of treatment is generous intravenous fluids, but could include dialysis or hemofiltration.
Rhabdomyolysis and its complications are significant problems for those injured in disasters such as earthquakes and bombing. Relief efforts in areas struck by earthquakes often include medical teams with skills and equipment for treatment of survivors with rhabdomyolysis. The disease and its mechanisms were first fully elucidated during the Blitz of London in 1941.