Top videos

Bilateral High flex knee replacements for British patient. 81 year old Ken Perris is highly satisfied after double flexible knee replacements in Chennai hospital by Orthopaedic surgeon Dr.A.K.Venkatachalam of www.kneeindia.com. High flex or flexible knee replacements confer the ability to kneel, squat, sit cross legged. Minimally invasive surgical approaches reduce pain and hasten recovery.
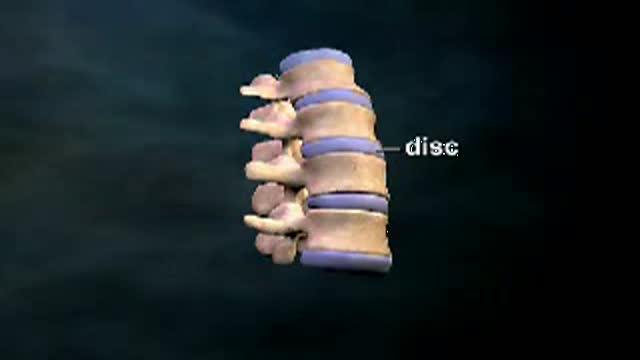
Herniated or Ruptured Disc: Between each of the vertebre of the spine is a disc which is filled with a gel type material to cushion the connection between the vertebre. With age or injury these intervertebral discs can rupture or herniate. This herniation causes them to push against the adjacent nerves which come from the spinal cord. This can frequently cause pain, numbenss and tingling. This animated video reviews herniated disc.

Otto Placik MD. a board certified Chicago based plastic surgeon presents Vulvar Vaginal Genital anatomy lesson reviewing the Vulva, Mons Pubis, clitoral hood, prepuce, frenulum, labia minora & majora, vagina, urethra and fourchette with surgical implications and techniques. Photos pictures and video of anatomic models are reviewed in detail on different models. Great for patients thinking about or planning before labiaplasty or vaginal cosmetic surgery
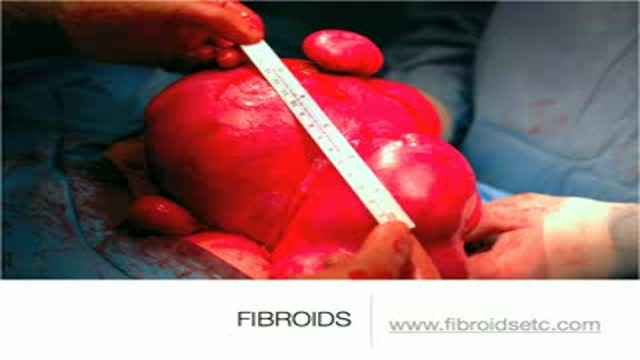
A uterine fibroid (also uterine leiomyoma, myoma, fibromyoma, leiofibromyoma, fibroleiomyoma, and fibroma) (plural of ... myoma is ...myomas or ...myomata) is a benign (non-cancerous) tumor that originates from the smooth muscle layer (myometrium) and the accompanying connective tissue of the uterus. Fibroids are the most common benign tumors in females and typically found during the middle and later reproductive years. While most fibroids are asymptomatic, they can grow and cause heavy and painful menstruation, painful sexual intercourse, and urinary frequency and urgency. Uterine fibroids is the major indication for hysterectomy in the US.[2] Fibroids are often multiple and if the uterus contains too many leiomyomatas to count, it is referred to as uterine leiomyomatosis. The malignant version of a fibroid is uncommon and termed a leiomyosarcoma.

Macrobiopsy of breast lesions is a complicated procedure when performed with vacuum assisted biopsy tools. The Spirotome is a hand-held needle set that doesn’t need capital investment, is ready to use and provides tissue samples of high quality in substantial amounts. In this way quantitative molecular biology is possible with one tissue sample. The Coramate is an automated version of this direct and frontal technology

Identify the anatomy and explain the physiology of the breast on diagrams and sonograms.
Describe and demonstrate the protocol for sonographic scanning of the breast, including the clock and quadrant methods, and targeted examinations based on mammographic findings.
Describe the various diagnostic pathways that may lead to a sonographic breast examination, and explain how the ultrasound findings are correlated with other imaging modalities.
Identify and describe sonographic images of benign and malignant features and common breast pathologies.
Explain biopsy techniques for breast tumors.
Define and use related medical terminology.
Explain the Patient Privacy Rule (HIPAA) and Patient Safety Act (see reference