Top videos

This gentleman has a significant lumbar herniated disc with a positive well straight leg raise test. In this evaluation I test his deep tendon reflexes, sensation, muscle strength, and perform a straight leg raise test, Braggards's test and Well straight leg raise test.
✅ Support OEP: https://paypal.me/OrthoEvalPal?locale.x=en_US
✅ OEP Website: https://orthoevalpal.com/
✅ Online Coaching: https://orthoevalpal.com/coaching
✅ OEP Podcasts: https://orthoevalpal.com/podcast
▶▶ Like us on facebook: https://www.facebook.com/OrthoEvalPal
▶▶ Follow on Instagram: https://www.instagram.com/
▶▶ Follow on Twitter: https://twitter.com/home
✔ Get our NEW downloadable 1.5 hour shoulder anatomy with cadaver dissection lecture: http://www.meorthopedicseminar....s.com/shop/shoulder-
✔Get our NEW downloadable 7.5 hour cervical and lumbar continuing ed course: http://www.meorthopedicseminar....s.com/shop/rehabilit
✔Get our NEW downloadable 6.0 hour shoulder continuing ed course: http://www.meorthopedicseminar....s.com/shop/comprehen
Interested in our Sponsor Product
EZ Slant (http://ezslant.com/)
Check out our new OEP merchandise: 👚👕☕️https://www.youtube.com/channe....l/UC76MsdkAQaBkCb35K
#wellstraightlegraise #herniateddisc #LBP #lowbackpain #OrthoEvalPal #SpecialTests #Orthopedics #physicaltherapy #physicaltherapytests #athletictraining

Do you think you have a hernia?
What are hernias?
The hernias we address in this http://DoctorsExpressHartsdale.com Medical Minute are inguinal, or groin, hernias. More common in men than women, an inguinal hernia can occur when part of the small intestine protrudes through a weakness or tear in the area between your abdomen and your thigh- or your groin. It's possible for anyone to get an inguinal hernia, but it is more commonly found in males.
Hernias form a bulge and can be accompanied by pain. Men have an approximate 26% lifetime risk of having hernia at some point in their life, where as women have a much lower chance of one- only about 3% of women will experience a hernia at some point in their life. There are other types of hernias, such as abdominal, or "hiatal" hernias but groin hernias outnumber abdominal hernias by about 3 to 1.
What causes a hernia?
The cause of a hernia is not always known, but hernias are often the result of weak spots in the abdominal wall. Weaknesses can be due to congenital defects (present at birth) or formed later in life. Some risk factors for inguinal hernia include:
• fluid or pressure in the abdomen
• heavy lifting
• straining during urination or bowel movements
• obesity
• chronic cough
• pregnancy
Hernias often form in people with weakened abdominal muscles or in those who do a lot of heavy lifting or straining, which is why we see it quite often in young men. Physiology plays a part: men have testicles and scrotum which descend through the inguinal canal-much larger in men than in women. That is part of the reason men tend to be more susceptible to hernias than women.
Symptoms of hernia
Symptoms of inguinal hernia usually include a bulge in the groin area and pain, pressure, or aching at the bulge—especially when lifting, bending, or coughing. These symptoms usually subside during rest periods. Men may also experience swelling around the testicles.
Screening and Diagnosis of Hernias
If you are having abdominal pain or pelvic bulge and pain, you want to see physician, and he or she will do an exam. They will use their finger, to see if you have a bulge in your scrotum or on your groin and they'll see if its reducible or not. If the exam doesn't give them the answer, they can then perform an ultrasound, an inexpensive test that can tell you the same day whether a hernia is present.
What to do if you think you have a hernia
Most of the time hernias do not cause problems. People often live with hernias their entire life without them becoming aggravated or painful. When they do cause pain though, there is concern that complications may have arisen. Most common hernias are what we call reducible; you can take your finger or you can lie down in bed and due to the effects of gravity, the bulge in the groin will actually disappear, which means the intestinal contents actually go back into the abdominal cavity or to the correct location. If it's not reducible by lying down or using a finger or having a physician trying to reduce it, then there are concerns about complications such as strangulation, or incarceration occurring. If those concerns are there, then you need to see a surgeon, and there may be a need for surgery.
How to Treat a Hernia
As stated earlier, hernias can often be watched for years without being treated. If however, they are causing pain, we generally refer you to a surgeon who can do a very simple laparoscopic surgery.
If you suspect a hernia, but have not been diagnosed, you should see your doctor, and of course, we are happy to see you here at Doctors Express
A bone marrow biopsy removes a small amount of bone and a small amount of fluid and cells from inside the bone (bone marrow). A bone marrow aspiration removes only the marrow. These tests are often done to find the reason for many blood disorders and may be used to find out if cancer or infection has spread to the bone marrow. Bone marrow aspiration removes a small amount of bone marrow fluid and cells through a needle put into a bone. The bone marrow fluid and cells are checked for problems with any of the blood cells made in the bone marrow. Cells can be checked for chromosome problems. Cultures can also be done to look for infection. A bone marrow biopsy removes bone with the marrow inside to look at under a microscope. The aspiration (taking fluid) is usually done first, and then the biopsy.
minimally invasive procedure is the new gold standard for hemorrhoidectomy, according to American and European experts in the field. The procedure, known as PPH (procedure for prolapse and hemorrhoids) stapled hemorrhoidectomy, combines hemorrhoidal devascularization and repositioning to return the veins to the anal canal. “This year, this is the revolutionary new procedure in the United States,” Gary Hoffman, MD, clinical faculty member in general and colorectal surgery, Cedars-Sinai Medical Center, Los Angeles, told General Surgery News after moderating a live PPH telesurgery at the 2003 annual meeting of the Society of American Gastrointestinal Endoscopic Surgeons.

Symptoms of depression in women include: Persistent sad, anxious, or "empty" mood. Loss of interest or pleasure in activities, including sex. Restlessness, irritability, or excessive crying. Feelings of guilt, worthlessness, helplessness, hopelessness, pessimism. Sleeping too much or too little, early-morning awakening.

Dr. Leo Maguire, a Mayo Clinic ophthalmologist, explains how laser-assisted in situ keratomileusis (LASIK) eye surgery can correct common vision problems.
This interview originally aired Jan. 26, 2019.
To learn more about LASIK surgery, visit: https://www.mayoclinic.org/tests-procedures/lasik-eye-surgery/about/pac-20384774?mc_id=us&utm_source=newsnetwork&utm_medium=l&utm_content=content&utm_campaign=mayoclinic&geo=national&placementsite=enterprise&cauid=100721&_ga=2.112234244.1227307149.1547427243-1780934405.1469629163

In this video, we have explained the procedure of total #knee #replacement #surgery in patient in 3D animation.
Learn more: https://ecgkid.com
_____________________________________________________________________
Knee replacement, commonly known as complete knee replacement or knee arthroplasty, is a surgical treatment that resurfaces a knee that has been destroyed by arthritis. The extremities of the bones that make up the knee joint, as well as the kneecap, are capped with metal and plastic pieces. Someone with severe arthritis or a major knee injury may benefit from this procedure.
The knee joint can be affected by a variety of arthritis forms. The degradation of joint cartilage and neighboring bone in the knees can be caused by osteoarthritis, a degenerative joint disease that primarily affects middle-aged and older persons. Rheumatoid arthritis produces pain and stiffness by inflaming the synovial membrane and resulting in an excess of synovial fluid. Traumatic arthritis, or arthritis caused by an injury, can harm the joints.
The purpose of knee replacement surgery is to resurface damaged areas of the knee joint and cure knee discomfort that has not responded to prior therapies.
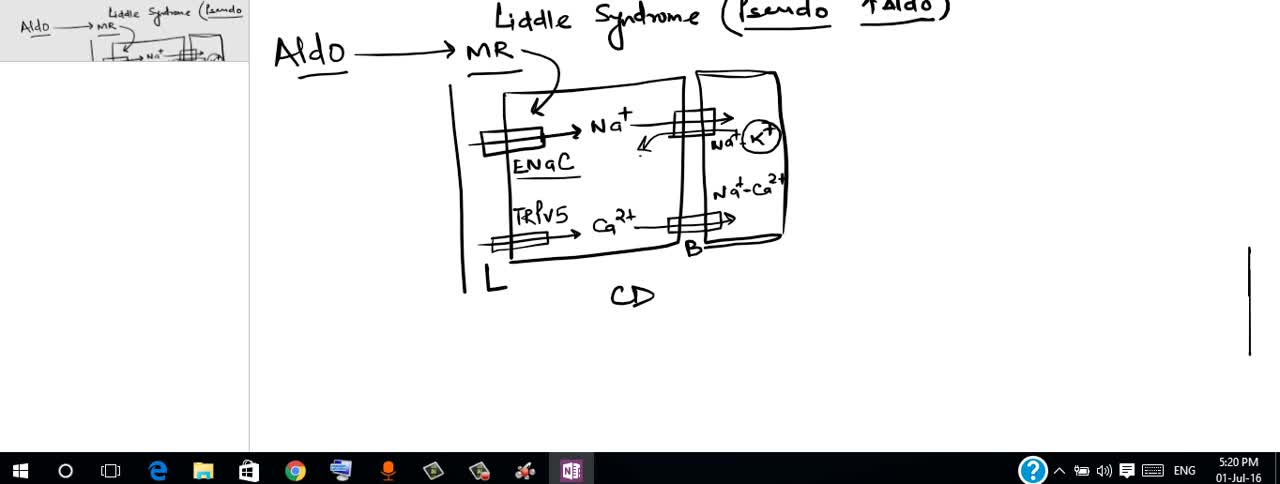
Liddle syndrome is an inherited form of high blood pressure (hypertension). This condition is characterized by severe hypertension that begins unusually early in life, often in childhood, although some affected individuals are not diagnosed until adulthood. Some people with Liddle syndrome have no additional signs or symptoms, especially in childhood. Over time, however, untreated hypertension can lead to heart disease or stroke, which may be fatal.

The sinus is a hollow area in the back part of the mouth, when people lost thier teeth in this area, the bone will quickly resorbed, One way we can place implant into this area is by put graft materials in the sinus and hoped that the bone will take and allow us to place implant into the grafted bone. The grafting increases the time and the risk of successful implantation.

Otto Placik MD. a board certified Chicago based plastic surgeon presents Vulvar Vaginal Genital anatomy lesson reviewing the Vulva, Mons Pubis, clitoral hood, prepuce, frenulum, labia minora & majora, vagina, urethra and fourchette with surgical implications and techniques. Photos pictures and video of anatomic models are reviewed in detail on different models. Great for patients thinking about or planning before labiaplasty or vaginal cosmetic surgery