Top videos
Removal of the womb by keyhole surgery. The womb is detached from its pelvic attachments and removed through the birth canal. The birth canal is then stitched closed.
Watch that video of a Korean model disfigured after cooking oil injections
Women are routinely invited to have cervical screening tests (also called smear tests). The tests are done to prevent cervical cancer, not to diagnose cancer. During each test some cells are removed from the neck of the womb (cervix), with a plastic brush. The cells are examined under a microscope to look for early changes that, if ignored and not treated, could develop into cancer of the cervix. You are very unlikely to develop cervical cancer if you have regular cervical screening tests at the times advised by your doctor. If the test shows any abnormality, you will have treatment to stop you ever getting cancer of the cervix. So, an abnormal test does not mean you have cancer. It means you should have some treatment to stop you getting cancer.
Thighplasty after massive weight loss
The Respiratory System
Breast reduction can relieve strain from shoulder straps, neck, back, and upper arms.
It can provide an uplift to help clothes fit and look better. Traditionally, insurance companies would provide benefits for a broad range of breast sizes and gram weight of tissue to be removed from each breast. At present most insurance companies limit authorization when the doctor plans to remove less than 500gm weight per breast. Since many patients present with symptoms in a D cup to DD cup, often, the very removal of over 500 grams weight may reduce the breasts too much. This amount of reduction may not be in harmony with body shape. Newer methods of breast assembly after reduction, will tighten things using internal brassiere techniques that also compact and reduce breast volume. Therefore, a gram weight reduction of 500gms in some patients combined with internal tightening efforts, could pose an over-reduction. With the unreliability of insurance support in some cases, it is best not to look solely at gram weight in the surgical planning of breast reduction. When excess skin and weight is removed, the improved location of the breasts on the chest will give marked relief of symptoms.
Surgery takes from 2 to 5 hours and can be done as an outpatient or with a brief overnight stay. When possible, no scarring other than around the areola can be planned which follows the Brazilian and French methods (Goes and Benelli). For very large reductions, a vertical method, or T pattern approach is offered. Recovery is a few days, with special care to avoid strain for 4 to 6 weeks. Some soreness may persist for a few weeks. The breasts can appear tight, swollen, and bruised at first, but will usually settle to their near final look by 6 weeks. There may be sutures to be removed in some cases. Costs relate to the severity of the sag, and weight of the breasts.
The operation can make a stunning change in body image, relief of upper body symptoms, and offer a cosmetic lift to naturally sloping breasts.
http://www.hypodermic-injection.com This is a demonstration of an IM hypodermic injection administered in the gluteus maximus muscle. The patient is in the prone position.
Examination of the eye by an ophthalmoscope from the USMLE collection
The peroneal artery is closely positioned to the fibula. The artery arises from the tibioperoneal trunk, distal to the takeoff of the anterior tibial artery (seen in the illustration below perforating the interosseous membrane). The peroneal artery sends perforators laterally to the skin of the lower leg, sometimes in a septocutaneous fashion via the lateral intermuscular septum, but often with muscular perforators. The length of the pedicle is usually short, but can be increased substantially by dissecting the peroneal artery and its venae from the fibula and using the distal bone for reconstruction.
A breech birth is the birth of a baby from a breech presentation. In the breech presentation the baby enters the birth canal with the buttocks or feet first as opposed to the normal head first presentation.
There are either three or four main categories of breech births, depending upon the source:
* Frank breech - the baby's bottom comes first, and his or her legs are flexed at the hip and extended at the knees (with feet near the ears). 65-70% of breech babies are in the frank breech position.
* Complete breech - the baby's hips and knees are flexed so that the baby is sitting crosslegged, with feet beside the bottom.
* Footling breech - one or both feet come first, with the bottom at a higher position. This is rare at term but relatively common with premature fetuses.
* Kneeling breech - the baby is in a kneeling position, with one or both legs extended at the hips and flexed at the knees. This is extremely rare, and is excluded from many classifications.
As in labour with a baby in a normal head-down position, uterine contractions typically occur at regular intervals and gradually cause the cervix to become thinner and to open. In the more common breech presentations, the baby’s bottom (rather than feet or knees) is what is first to descend through the maternal pelvis and emerge from the vagina.
At the beginning of labour, the baby is generally in an oblique position, facing either the right or left side of the mother's back. As the baby's bottom is the same size in the term baby as the baby's head. Descent is thus as for the presenting fetal head and delay in descent is a cardinal sign of possible problems with the delivery of the head.
In order to begin the birth, internal rotation needs to occur. This happens when the mother's pelvic floor muscles cause the baby to turn so that it can be born with one hip directly in front of the other. At this point the baby is facing one of the mother's inner thighs. Then, the shoulders follow the same path as the hips did. At this time the baby usually turns to face the mother's back. Next occurs external rotation, which is when the shoulders emerge as the baby’s head enters the maternal pelvis. The combination of maternal muscle tone and uterine contractions cause the baby’s head to flex, chin to chest. Then the back of the baby's head emerges and finally the face.
Due to the increased pressure during labour and birth, it is normal for the baby's leading hip to be bruised and genitalia to be swollen. Babies who assumed the frank breech position in utero may continue to hold their legs in this position for some days after birth.
Examination of different gaits
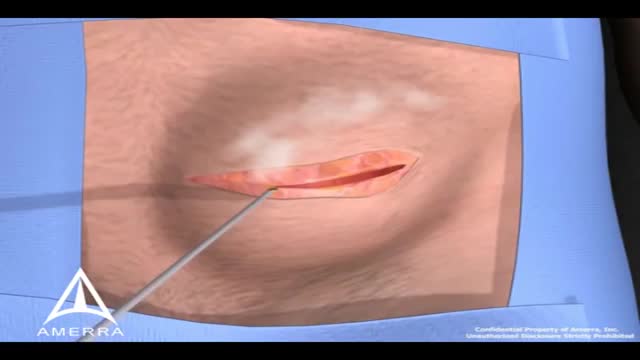
During surgery to repair the hernia, the bulging tissue is pushed back in. Your abdominal wall is strengthened and supported with sutures (stitches), and sometimes mesh. This repair can be done with open or laparoscopic surgery. You and your surgeon can discuss which type of surgery is right for you.
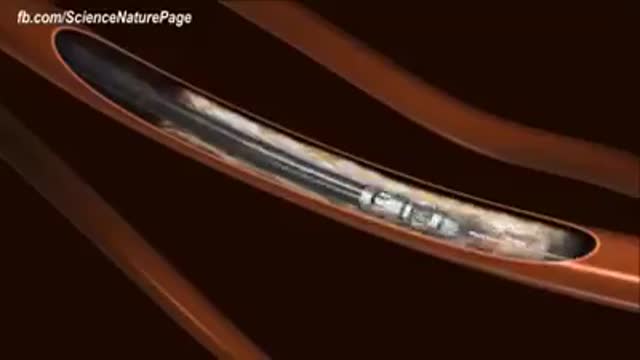
Cholesterol is a fat-like, waxy substance that can be found in all parts of your body. It helps your body make cell membranes, many hormones, and vitamin D. The cholesterol in your blood comes from two sources: the foods you eat and your liver. But your liver makes all the cholesterol your body needs.
http://www.mediplus.co.uk A new and safer method of inserting a Foley catheter suprapubically. The technique allows the insertion to be carried out in an Outpatient setting, thus saving time, cost and effort. By using the Seldinger technique, the product reduces the chances of bowel or bladder perforation and resultant morbidity.
The product has been chosen by The NHS National Technology Adoption Centre to help facilitate adoption of the product.
Watch that video of Indian boy has 232 teeth removed from his mouth
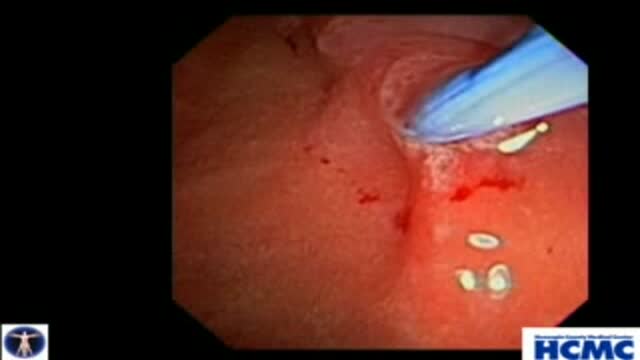
Biliary and Pancreatic Sphincterotomies for Sphincter of Oddi Dysfunction
This 43 year old woman has severe recurrent RUQ pain post cholecystectomy. Liver and pancreatic chemistries and duct size are normal, but pancreatic manometry is abnormal. The plan is to perform dual biliary and pancreatic sphincterotomy. The pancreatic duct is cannulated with a 3.9 French tip tr...iple lumen papillotome loaded with a 0.025 inch Jagwire. Contrast is injected to outline the course of the duct. The wire is passed to the tail. Notice the knuckling of the wire into the tail. This provides a safety loop, but is only safe in a small duct with use of a smaller caliber wire. Then with the wire securely in PD, papillotome is used to cannulate the bile duct. Placement of the wire in PD guarantees access for pancreatic stent placement, which is mandatory in these patients to reduce risk, it also facilitates difficult biliary cannulation. Here is the fluoroscopic view as the papillotome is passed deep into bile duct. This shows wires in the CBD and PD. Now a biliary sphincterotomy is performed, with the pancreatic guidewire in place beside the papillotome. The scope is pushed into a longer position to orient up the middle of the papilla. The sphincterotomy is done in very careful stepwise fashion to avoid perforation. Now the biliary wire is removed and the papillotome passed over the pancreatic wire for pancreatic sphincterotomy. The incision is aimed back up towards the biliary sphincterotomy to ensure the septum only is cut. Note the large pancreatic orifice. Last, a 4 French 9cm unflanged soft material pancreatic stent is placed. We always use single pigtail design to avoid inward migration of the stent. The long unflanged design allows spontaneous passage within a few weeks.
Medical examination of the abdomen from Loyola University, Chicago
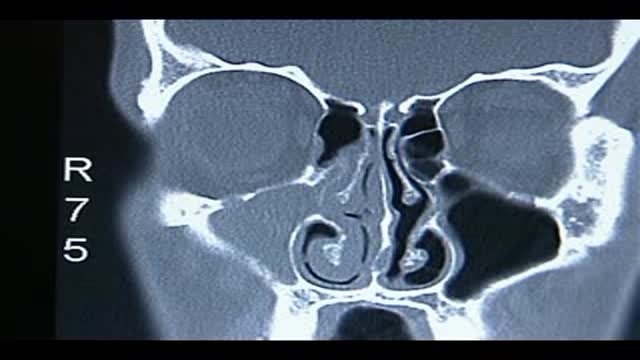
Loyola Respiratory System Exam Part 2 A video from Loyola Medical School, Chicago showing the medical and clinical examination of the respiratory system.
The endoscopic removal of a large intramaxillary sinus cyst which contained serous like fluid and many shiny falt white cholesterol crystals.