Top videos

How to perform a parotidectomy gland resection? In this video we take you step by step through the protid gland resection surgical technique. This video is intended for ENT residents and Head and Neck Surgery Surgeons. It is part of the ORL-Information's Head and Neck surgery Masterclass in collaboration with the University Hospital of Nîmes. Surgeons Editors: Pr. Benjamin LALLEMANT, MD, PhD - Dr. Camille GALY, MD Head and and Neck Department, University Hospital of Nîmes, France Official video | www.orl-information.fr
Cette vidéo présentent la technique de la parotidectomie avec dissection du nerf facial. Elle illustre les différents temps de l'intervention notamment le temps de repérage du nerf facial.
--------------------------------------
@Prévention médecine | Comment préserver sa santé ?
✔Abonnez-vous à la chaîne ORL-Information : https://www.youtube.com/c/ORLINFORMATION
✔Retrouvez-nous sur internet: https://www.orl-information.fr
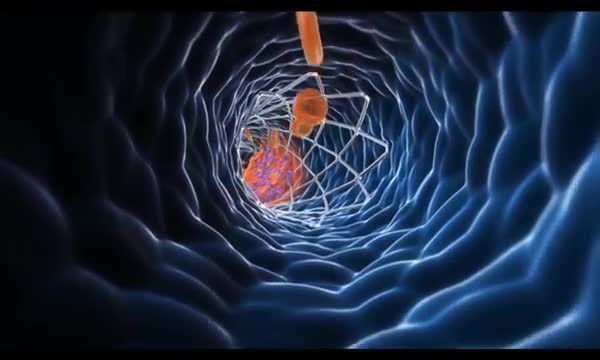
Coronary artery bypass grafting (CABG) is a type of surgery that improves blood flow to the heart. Surgeons use CABG to treat people who have severe coronary heart disease (CHD). CHD is a disease in which a waxy substance called plaque (plak) builds up inside the coronary arteries.

The sinus is a hollow area in the back part of the mouth, when people lost thier teeth in this area, the bone will quickly resorbed, One way we can place implant into this area is by put graft materials in the sinus and hoped that the bone will take and allow us to place implant into the grafted bone. The grafting increases the time and the risk of successful implantation.

Otto Placik MD. a board certified Chicago based plastic surgeon presents Vulvar Vaginal Genital anatomy lesson reviewing the Vulva, Mons Pubis, clitoral hood, prepuce, frenulum, labia minora & majora, vagina, urethra and fourchette with surgical implications and techniques. Photos pictures and video of anatomic models are reviewed in detail on different models. Great for patients thinking about or planning before labiaplasty or vaginal cosmetic surgery