Top videos

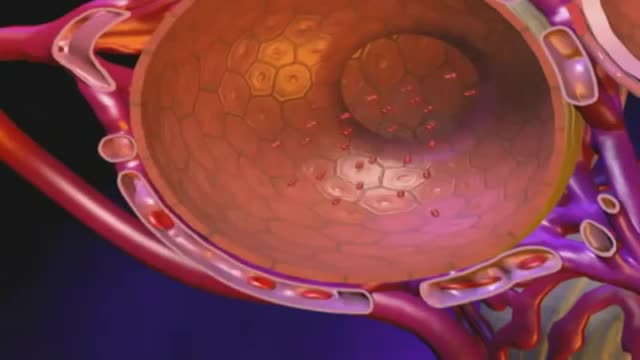
The sinus is a hollow area in the back part of the mouth, when people lost thier teeth in this area, the bone will quickly resorbed, One way we can place implant into this area is by put graft materials in the sinus and hoped that the bone will take and allow us to place implant into the grafted bone. The grafting increases the time and the risk of successful implantation.

Otto Placik MD. a board certified Chicago based plastic surgeon presents Vulvar Vaginal Genital anatomy lesson reviewing the Vulva, Mons Pubis, clitoral hood, prepuce, frenulum, labia minora & majora, vagina, urethra and fourchette with surgical implications and techniques. Photos pictures and video of anatomic models are reviewed in detail on different models. Great for patients thinking about or planning before labiaplasty or vaginal cosmetic surgery

How to use a Hepatitis B rapid test kit for self-diagnosis of Hepatitis B (fingerstick blood). Convenient, Easy to Use, and over 98% Accurate. Certified GMP and ISO13485. Test yourself at home with Complete Privacy. Buy online today at: http://www.stdrapidtest.com

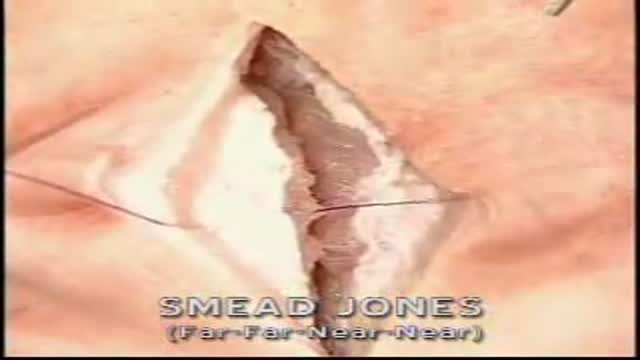
Care must be taken to prevent stenosis at the anastomotic site. If the diameter of the anastomosis is less than 2 cm, the anastomosis should be taken down and resected. A classic end-to-end anastomosis should be performed to ensure adequate diameter to the intestine. If the posterior wall of the colon has been preserved, care should be taken to close the colostomy prior to opening the peritoneal cavity. This will reduce intraperitoneal contamination from the stoma site. Copious irrigation of the wound should be made prior to primary closure. If gross contamination has occurred, delayed closure of the wound should be considered.
This 40 years old man lost his arm in car turn over in 2015. The video is taken 2 years after replantation. You can see another videos in my site: https://drliaghatclinic.com, https://instagram.com/liaghatclinic, https://t.me/liaghatclinic
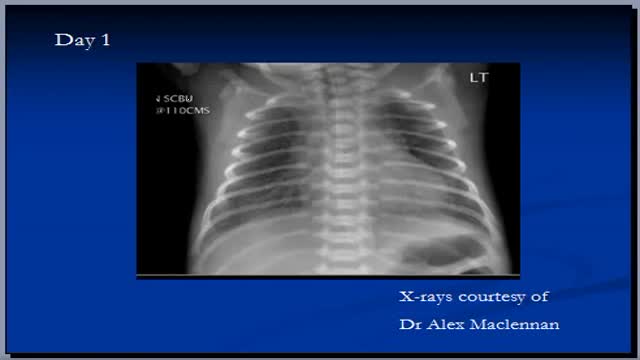
Bronchiectasis is an abnormal dilation of the proximal and medium-sized bronchi (>2 mm in diameter) caused by weakening or destruction of the muscular and elastic components of the bronchial walls. Affected areas may show a variety of changes, including transmural inflammation, edema, scarring, and ulceration, among other findings. Distal lung parenchyma may also be damaged secondary to persistent microbial infection and frequent postobstructive pneumonia. Bronchiectasis can be congenital but is most often acquired.[9] Congenital bronchiectasis usually affects infants and children. These cases result from developmental arrest of the bronchial tree. Acquired forms occur in adults and older children and require an infectious insult, impairment of drainage, airway obstruction, and/or a defect in host defense. The tissue is also damaged in part by the host response of neutrophilic proteases, inflammatory cytokines, nitric oxide, and oxygen radicals. This results in damage to the muscular and elastic components of the bronchial wall. Additionally, peribronchial alveolar tissue may be damaged, resulting in diffuse peribronchial fibrosis.[12] The result is abnormal bronchial dilatation with bronchial wall destruction and transmural inflammation. The most important functional finding of altered airway anatomy is severely impaired clearance of secretions from the bronchial tree. Impaired clearance of secretions causes colonization and infection with pathogenic organisms, contributing to the purulent expectoration commonly observed in patients with bronchiectasis. The result is further bronchial damage and a vicious cycle of bronchial damage, bronchial dilation, impaired clearance of secretions, recurrent infection, and more bronchial damage
Vaginal discharge serves an important housekeeping function in the female reproductive system. Fluid made by glands inside the vagina and cervix carries away dead cells and bacteria. This keeps the vagina clean and helps prevent infection. Most of the time, vaginal discharge is perfectly normal. The amount can vary, as can odor and hue (its color can range from clear to a milky white-ish), depending on the time in your menstrual cycle. For example, there will be more discharge if you are ovulating, breastfeeding, or are sexually aroused. The smell may be different if you are pregnant or you haven't been diligent about your personal hygiene. None of those changes is cause for alarm. However, if the color, smell, or consistency seems significantly unusual, especially if it accompanied by vaginal itching or burning, you could be noticing an infection or other condition. What causes abnormal discharge? Any change in the vagina's balance of normal bacteria can affect the smell, color, or discharge texture. These are a few of the things that can upset that balance:

Shut the front door: Scientists have finally found the perfect breasts. No, they weren't hiding in the Amazon or roving solo across the Sahara (although we have no doubt there are women in both the Amazon and the Sahara who have magnificent mammaries); it turns out these perfect breasts were hiding in a plastic surgeon's office this whole time! Now, before you get all worked up, the American Society of Plastic Surgeons (ASPS) would like you to know that the super-fake looking plastic breasts of yore are not actually what people think are most attractive now. According to a study published in the Journal of Plastic and Reconstructive Surgery—which involved asking over 1,300 people to look at pictures of naked boobies and rank them by hotness (stop laughing, this is serious research!)—people preferred a more "real" and "normal" look from their silicone, with the ideal breast shape having a 45:55 ratio. People said the best chests have 45 percent of the fullness above the nipple line and 55 percent of the fullness below, in a slightly teardrop shape. Researchers noted this preference remained consistent across gender, racial, and ethnic groups with the 45:55 ratio favored by 87 percent of women in their 30s, 90 percent of men, and 94 percent of plastic surgeons.

Genital warts are soft growths that appear on the genitals. Genital warts are a sexually transmitted infection (STI) caused by certain strains of the human papillomavirus (HPV). These skin growths can cause pain, discomfort, and itching. They are especially dangerous for women because some types of HPV can also cause cancer of the cervix and vulva.