Top videos
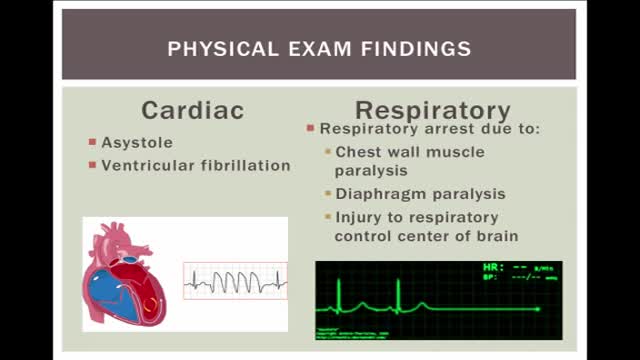
Electrical injuries can present with a variety of problems, including cardiac or respiratory arrest, coma, blunt trauma, and severe burns of several types. It is important to establish the type of exposure (high or low voltage), duration of contact, and concurrent trauma. Low-voltage AC injury without loss of consciousness and/or arrest These injuries are exposures of less than 1000V and usually occur in the home or office setting. Typically, children with electrical injuries present after biting or chewing on an electrical cord and suffer oral burns. Adults working on home appliances or electrical circuits can also experience these electrical injuries. Low-voltage AC may result in significant injury if there is prolonged, tetanic muscle contraction. Low-voltage AC injury with loss of consciousness and/or arrest In respiratory arrest or ventricular fibrillation that is not witnessed, an electrical exposure may be difficult to diagnose. All unwitnessed arrests should include this possibility in the differential diagnosis. Query EMS personnel, family, and coworkers about this possibility. Inquire if a scream was heard before the patient’s collapse; this may be due to involuntary contraction of chest wall muscles from electrical current. High-voltage AC injury without loss of consciousness and/or arrest Usually high-voltage injuries do not cause loss of consciousness but instead cause devastating thermal burns. In occupational exposures, details of voltage can be obtained from the local power company. High-voltage AC injury with loss of consciousness and/or arrest This is an unusual presentation of high-voltage AC injuries, which do not often cause loss of consciousness. History may need to come from bystanders or EMS personnel. Direct current (DC) injury These injuries typically cause a single muscle contraction that throws the victim away from the source. They are rarely associated with loss of consciousness unless there is severe head trauma, and victims can often provide their own history. Conducted electrical devices Conducted electrical weapons (CEWs) such as tasers are weapons used by law enforcement that deliver high-voltage current that is neither true AC or DC but is most like a series of low-amplitude DC shocks.[16] They can deliver 50,000 V in a 5-second pulse, with an average current of 2.1 mA.[17] Though they have been temporally associated with deaths in the law enforcement setting, conducted electrical devices (CEDs) in healthy volunteers have been shown to be safe without evidence of delayed arrhythmia or cardiac damage as measured by troponin I.[18, 17] One study of their use in 1201 law enforcement incidents showed mostly superficial puncture wounds from the device probes, and significant injuries only from trauma subsequent to shock, not from the device itself. Of 2 deaths in custody, neither was related to CEW exposure.[19]

A Lecture Presented by Dr. Mostafa Yakoot to Vascular Surgery Congress. TITLE: SAFETY & EFFICACY OF A NEW HONEY OINTMENT (PEDYPHAR) FOR DIABETIC FOOT ULCERS. Based on the original article in JWC by: Yakoot M, Abdelatif M, Etman M.
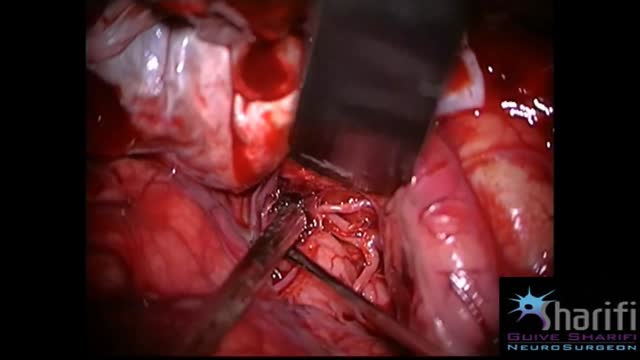
The goal of surgical clipping is to isolate an aneurysm from the normal circulation without blocking off any small perforating arteries nearby. Under general anesthesia, an opening is made in the skull, called a craniotomy. The brain is gently retracted to locate the aneurysm. A small clip is placed across the base, or neck, of the aneurysm to block the normal blood flow from entering. The clip works like a tiny coil-spring clothespin, in which the blades of the clip remain tightly closed until pressure is applied to open the blades. Clips are made of titanium and remain on the artery permanently.

Septic arthritis is also known as infectious arthritis, and is usually caused by bacteria, or fungus. The condition is an inflammation of a joint that's caused by infection. Typically, septic arthritis affects one large joint in the body, such as the knee or hip. Less frequently, septic arthritis can affect multiple joints