Top videos
Menorrhagia is the medical term for menstrual periods with abnormally heavy or prolonged bleeding. Although heavy menstrual bleeding is a common concern, most women don't experience blood loss severe enough to be defined as menorrhagia. With menorrhagia, you can't maintain your usual activities when you have your period because you have so much blood loss and cramping. If you dread your period because you have such heavy menstrual bleeding, talk with your doctor. There are many effective treatments for menorrhagia.

What is the spleen and what causes an enlarged spleen (splenomegaly)? The spleen sits under your rib cage in the upper left part of your abdomen toward your back. It is an organ that is part of the lymph system and works as a drainage network that defends your body against infection. White blood cells produced in the spleen engulf bacteria, dead tissue, and foreign matter, removing them from the blood as blood passes through it. The spleen also maintains healthy red and white blood cells and platelets; platelets help your blood clot. The spleen filters blood, removing abnormal blood cells from the bloodstream. A spleen is normally about the size of your fist. A doctor usually can't feel it during an exam. But diseases can cause it to swell and become many times its normal size. Because the spleen is involved in many functions, many conditions may affect it.

Focal seizures (also called partial seizures [citation needed] and localized seizures) are seizures which affect initially only one hemisphere of the brain. [citation needed] The brain is divided into two hemispheres, each consisting of four lobes – the frontal, temporal, parietal and occipital lobes.
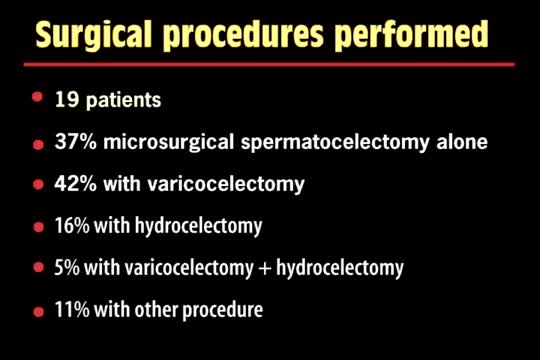
A spermatocelectomy is surgery to remove a spermatocele. A spermatocele is a cyst (sac of fluid) that contains sperm. It forms inside your scrotum on the outside of your testicle. The cyst is most often attached to your epididymis. The epididymis is a tube that stores sperm.

Dr. Joanna Chikwe, explains how patients may feel after heart surgery.
Learn more about the Smidt Heart Institute at Cedars-Sinai at https://ceda.rs/3meIA2A
Learn more about Dr. Joanna Chikwe at https://ceda.rs/3ul6I6t
Connect with us:
https://twitter.com/CedarsSinai
https://www.facebook.com/CedarsSinai
https://www.instagram.com/CedarsSinai
Cedars-Sinai is a leader in providing high-quality healthcare encompassing primary care, specialized medicine and research. Since 1902, Cedars-Sinai has evolved to meet the needs of one of the most diverse regions in the nation, setting standards in quality and innovative patient care, research, teaching and community service. Today, Cedars- Sinai is known for its national leadership in transforming healthcare for the benefit of patients. Cedars-Sinai impacts the future of healthcare by developing new approaches to treatment and educating tomorrow’s health professionals. Additionally, Cedars-Sinai demonstrates a commitment to the community through programs that improve the health of its most vulnerable residents.

Most people develop several moles (nevi) throughout adulthood. Moles can be found anywhere on the body, usually in sun-exposed areas, and are usually brown, smooth, and slightly raised. In most cases, a nevus is benign and doesn't require treatment. Rarely, they turn into melanoma or other skin cancers. A nevus that changes shape, grows bigger, or darkens should be evaluated for removal.
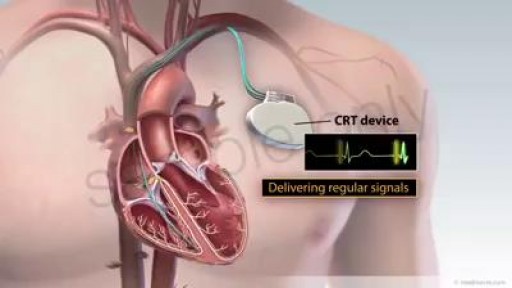
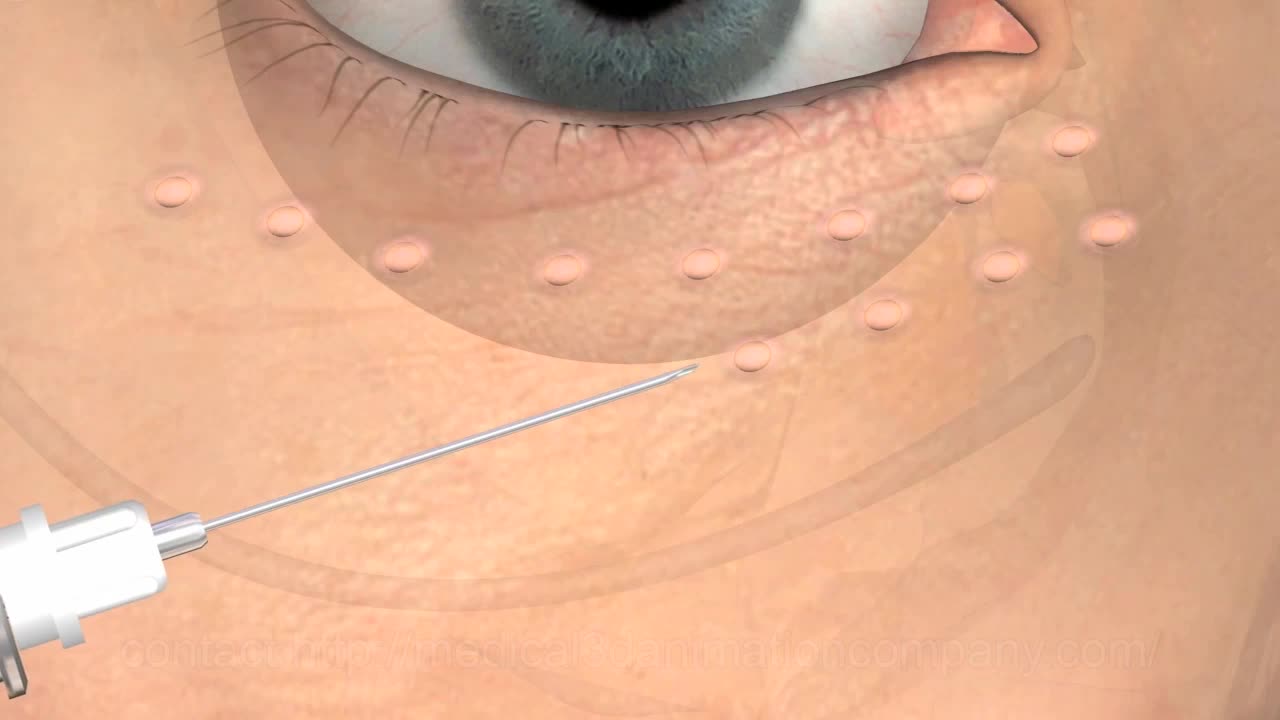
CRT is a clinically proven treatment option for some individuals with heart failure. A CRT device sends small electrical impulses to both lower chambers of the heart to help them beat together in a more synchronized pattern. This may improve the heart’s ability to pump blood and oxygen to your body. A CRT system is made up of two parts. The heart device, which is actually a tiny computer, plus a battery, contained in a small titanium metal case that is about the size of a pocket watch. Insulated wires, called leads, that are implanted to carry information signals from your heart to the heart device and to carry electrical impulses to your heart After the device system is implanted, an external computer, called a programmer, located at your doctor's office or clinic can be used to program the heart device and retrieve information from your heart device that will assist your doctor in your heart failure treatment. Your doctor will schedule periodic monitoring which may be done remotely if physician deems appropriate

A 76 year-old, female, presented with a three day history of melena without any abdominal pain. She had one episode of hematemesis (about 100 ml blood) in the emergency room, patient has a strong alcoholic drink abuse.
An upper endoscopy with magnification was performed.
multiple ulcers were detected across of the gastric camera,
esophageal varices was also detected

#CNA_Practice_Test Welcome to This CNA practice test 15 Basic Nursing Skills Fully Explained Answers. Includes questions from 171 to 180 of These 270 questions that are very similar to the real test #CNA_EXAM.