Top videos
The pathobiology of MM is complex and the root underlying cause of myeloma is the multistep genetic changes in the postgerminal center B cell. In addition, the bone marrow microenvironment plays a crucial role.[2] The interaction between myeloma cells and the microenvironment is mediated through adhesive interactions via cell-surface receptors, paracrine loops involving several cytokines, such as IL-6, VEGF and IL-10, and suppression of cell-mediated immunity.[2–4] IMiDs modulate many of these interactions leading to decreased myeloma cell growth and survival. Thalidomide was the first IMiD introduced to treat MM. It was initially synthesized in Germany in the late 1950s to treat insomnia and morning sickness. It was withdrawn from the market in 1961 because of its teratogenic effects. Its immunomodulatory properties were realized when it was observed to improve erythema nodosum leprosum, a painful immunologic reaction of leprosy, leading to its approval by the FDA in 1998 with tight prescribing and marketing regulations. Subsequent research showed the diverse mechanism of action of thalidomide including its immunomodulatory effect by inhibition of de novo IgM antibody synthesis,[5] modulation of the T-cell subset by increasing the T-helper cells, inhibitory effects on the TNF-α and antiangiogenic activity leading to its use in MM. Significantly higher response rates in combination with dexamethasone led to its approval in the treatment of newly diagnosed MM in 2006. Lenalidomide, a second-generation IMiD, was developed from the structural backbone of the thalidomide molecule by the addition of an amino group (NH2-) at position 4 of the phthaloyl ring and removal of the carbonyl group (C = O) of the 4-amino-substituted phthaloyl ring (Table 1).[6] In addition to immunomodulatory effects, other mechanisms of action have been described such as direct cytotoxicity via induction of apoptosis, inhibition of cell adhesion molecules and inhibition of growth signals that promote bone marrow angiogenesis

Patient Greg Grindley communicates with host Bryant Gumbel and his wife for the first time while undergoing deep brain stimulation surgery at University Hospital's Case Medical Center in Cleveland, Ohio.
➡ Subscribe: http://bit.ly/NatGeoSubscribe
About National Geographic:
National Geographic is the world's premium destination for science, exploration, and adventure. Through their world-class scientists, photographers, journalists, and filmmakers, Nat Geo gets you closer to the stories that matter and past the edge of what's possible.
Get More National Geographic:
Official Site: http://bit.ly/NatGeoOfficialSite
Facebook: http://bit.ly/FBNatGeo
Twitter: http://bit.ly/NatGeoTwitter
Instagram: http://bit.ly/NatGeoInsta
Greg's First In-Surgery Conversation | Brain Surgery Live
https://youtu.be/zvqV_2zncNU
National Geographic
https://www.youtube.com/natgeo

What Is a Hair Transplant? It's a type of surgery that moves hair you already have to fill an area with thin or no hair. Doctors have been doing these transplants in the U.S. since the 1950s, but techniques have changed a lot in recent years. You usually have the procedure in the doctor's office. First, the surgeon cleans your scalp and injects medicine to numb the back of your head. Your doctor will choose one of two methods for the transplant: follicular unit strip surgery (FUSS) or follicular unit extraction (FUE). With FUSS, the surgeon removes a 6- to 10-inch strip of skin from the back of your head. He sets it aside and sews the scalp closed. This area is immediately hidden by the hair around it. Next, the surgeon’s team divides the strip of removed scalp into 500 to 2,000 tiny grafts, each with an individual hair or just a few hairs. The number and type of graft you get depends on your hair type, quality, color, and the size of the area where you’re getting the transplant. If you’re getting the FUE procedure, the surgeon’s team will shave the back of your scalp. Then, the doctor will remove hair follicles one by one from there. The area heals with small dots, which your existing hair will cover. After that point, both procedures are the same. After he prepares the grafts, the surgeon cleans and numbs the area where the hair will go, creates holes or slits with a scalpel or needle, and delicately places each graft in one of the holes. He’ll probably get help from other team members to plant the grafts, too. Depending on the size of the transplant you’re getting, the process will take about 4 to 8 hours. You might need another procedure later on if you continue to lose hair or decide you want thicker hair. Expectations and Recovery After the surgery, your scalp may be very tender. You may need to take pain medications for several days. Your surgeon will have you wear bandages over your scalp for at least a day or two. He may also prescribe an antibiotic or an anti-inflammatory drug for you to take for several days. Most people are able to return to work 2 to 5 days after the operation. Within 2 to 3 weeks after surgery, the transplanted hair will fall out, but you should start to notice new growth within a few months. Most people will see 60% of new hair growth after 6 to 9 months. Some surgeons prescribe the hair-growing drug minoxidil (Rogaine) to improve hair growth after transplantation, but it’s not clear how well it works. Risks and Costs of Treatment The price of a hair transplant will depend largely on the amount of hair you’re moving, but it generally ranges from $4,000 to $15,000. Most insurance plans don’t cover it.
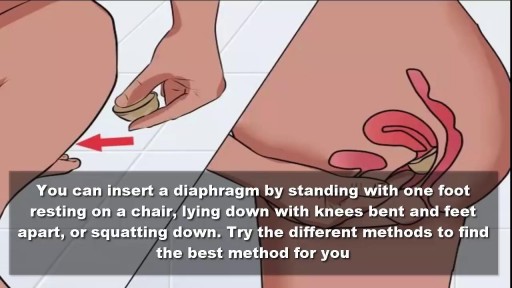
To use the diaphragm, first cover the inside of it with spermicide. Then insert it into your vagina so that it covers your cervix. You can insert the diaphragm up to 6 hours before sex. You should leave it in for at least 6 hours after the last time you have sex.
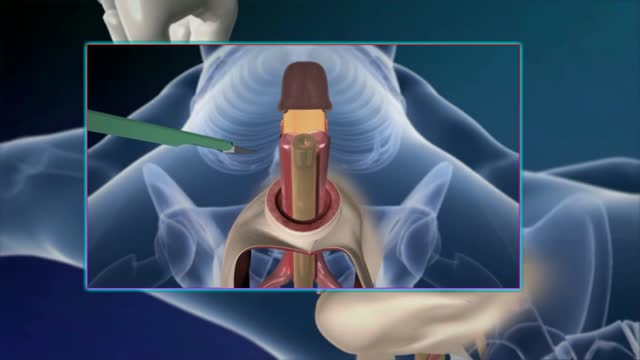
Sex reassignment surgery for male-to-female involves reshaping the male genitals into a form with the appearance of, and, as far as possible, the function of female genitalia. Prior to any surgeries, patients usually undergo hormone replacement therapy (HRT), and, depending on the age at which HRT begins, facial hair removal. There are associated surgeries patients may elect to, including facial feminization surgery, breast augmentation, and various other procedures
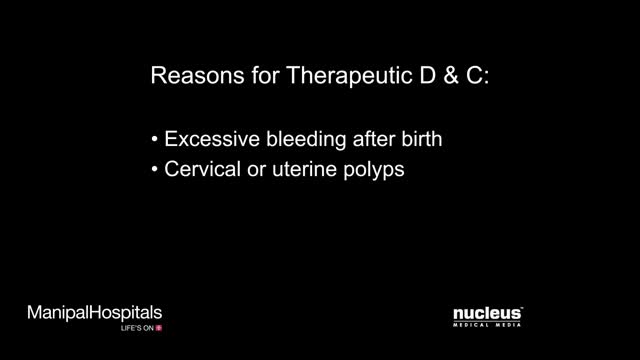
Dilation and curettage (D&C) is a procedure to remove tissue from inside your uterus. Doctors perform dilation and curettage to diagnose and treat certain uterine conditions — such as heavy bleeding — or to clear the uterine lining after a miscarriage or abortion. In a dilation and curettage — sometimes spelled "dilatation" and curettage — your doctor uses small instruments or a medication to open (dilate) your cervix — the lower, narrow part of your uterus. Your doctor then uses a surgical instrument called a curette to remove uterine tissue. Curettes used in a D&C can be sharp or use suction

Alexandra J. Golby, MD, Director, Image-guided Neurosurgery at Brigham and Women’s Hospital, discusses technological advancements to improve the precision of surgery to remove brain tumors.
It’s estimated that each year nearly 80,000 people are diagnosed with primary brain tumors and 100,000 with metastatic brain tumors. Nearly everybody is at risk for developing a brain tumor. Brain tumors can affect people from childhood to the last years of their lives. Men are slightly more affected than women and the causes of most brain tumors are not known.
There are a number of unique challenges in treating brain tumors. One challenge is that primary tumors can have indistinct margins that are difficult to see. Another challenge is that the tissue around a brain tumor is uniquely important and may impact things like language, visual and motor function.
The AMIGO Suite, opened in 2011 at Brigham and Women’s Hospital, is the Advanced Multimodality Image Guided Operating Suite. It's an NIH-funded national center which was developed with the goal of translating technological advances into improvements in surgical and interventional care for patients. In the AMIGO Suite, there is an intraoperative MRI scanner which can be brought in and out of the operating room during surgery to help surgeons visualize a patient’s tumor better.
Image-guided surgery uses the information obtained from advanced imaging and translates that into the planning and execution of surgery by acquiring high resolution and specialty structural images of the brain and also functional images of the brain. These images can be registered to one another and then to the patient's head during surgery. This allows surgeons to pinpoint the location of the tumor as well as the areas that we would like to preserve, areas that serve critical brain functions are located.
One of the big challenges, even with image-guided surgery, is that as we perform the surgery, the configuration of the brain is changing, and we call that brain shift. And it's due to changes in the brain itself and also as we remove tissue, things are constantly shifting and moving. When we're talking about doing brain tumor surgery, a few millimeters of movement can be a big difference. How to measure and track brain shift is an important area of research and a number of technologies are being studied to understand how to measure brain shift during surgery.
The development of various intraoperative imaging technologies allows surgeons to provide the most accurate surgical treatment for each individual patient.
Learn more about precision brain surgery at Brigham and Women’s Hospital:
https://www.brighamandwomens.o....rg/neurosurgery/brai

The cardiac cycle is the sequence of events that occurs when the heart beats. As the heart beats, it circulates blood through pulmonary and systemic circuits of the body. There are two phases of the cardiac cycle. In the diastole phase, the heart ventricles are relaxed and the heart fills with blood