Top videos
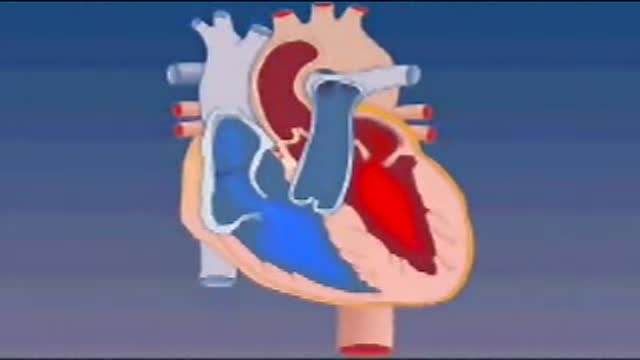
Blood enters the heart through two large veins, the inferior and superior vena cava, emptying oxygen-poor blood from the body into the right atrium. As the atrium contracts, blood flows from your right atrium into your right ventricle through the open tricuspid valve.
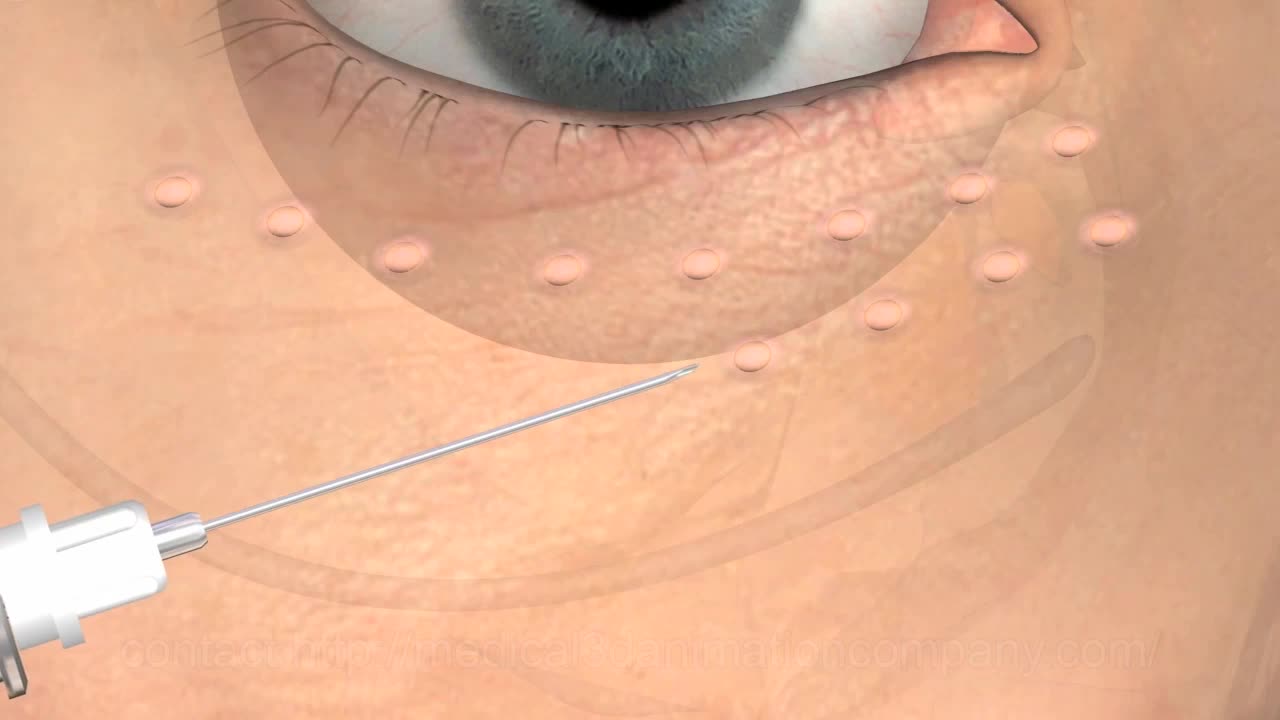
Thoracentesis is a procedure in which a needle is inserted into the pleural space between the lungs and the chest wall. This procedure is done to remove excess fluid, known as a pleural effusion, from the pleural space to help you breathe easier. It may be done to determine the cause of your pleural effusion. Some conditions such as heart failure, lung infections, and tumors can cause pleural effusions.
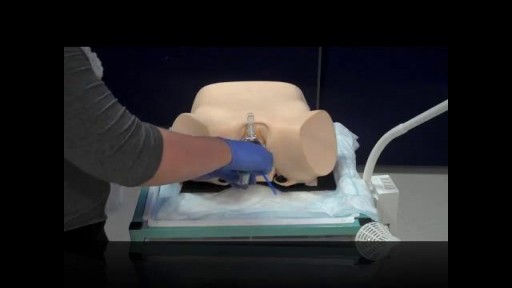
Pelvic examinations during labor are used for several purposes, among them assessment of cervical dilatation, effacement, station of the presenting part, presentation, position, and pelvic capacity.Instruction in these techniques is particularly important for those health care providers involved in labor management, including physicians, nurses, midwives, paramedics and EMT personnel.
There are several approaches to scoliosis surgery, but all use modern instrumentation systems in which hooks and screws are applied to the spine to anchor long rods. The rods are then used to reduce and hold the spine while bone that is added fuses together with existing bone.
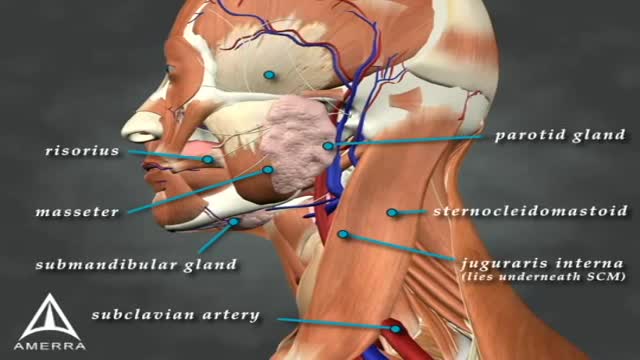
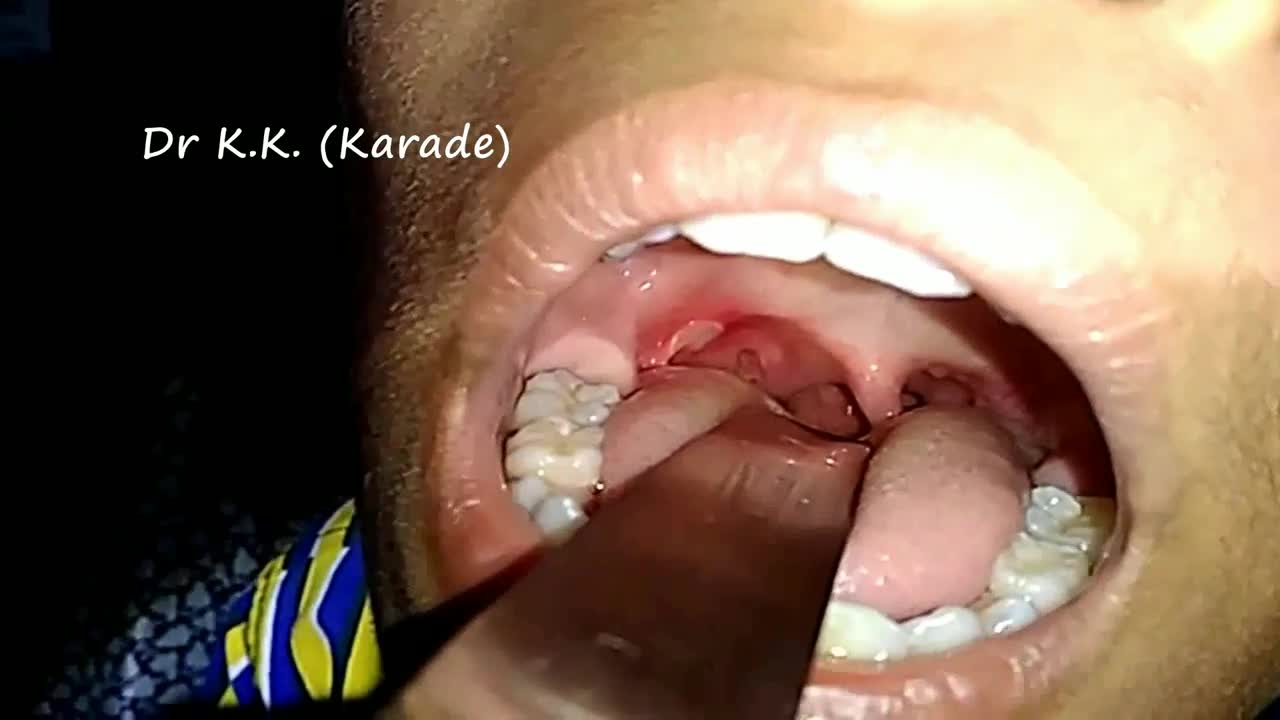
Sialorrhea or excessive drooling is a major issue in children with cerebral palsy and adults with neurodegenerative disorders. In this review, we describe the clinical features, anatomy and physiology of sialorrhea, as well as a review of the world literature on medical treatment using Yale University’s search engine; including but not limited to Medline and Erasmus. Level of drug efficacy is defined according to the guidelines of American Academy of Neurology. Current medical management is unsatisfactory. Topical agents (scopolamine and tropicamide) and oral agents (glyccopyrolate) combined render a level B evidence (probably effective); however, this treatment is associated with troublesome side effects. Double-blind and placebo-controlled studies of botulinum toxin (BoNT) provide a level A evidence for type B (two class I studies; effective and established) and both overall and individual B level of evidence for OnabotulinumtoxinA (A/Ona) and AbobotulinumtoxinA (A/Abo); these are probably effective. For IncobotulinumtoxinA (A/Inco), the level of evidence is U (insufficient) due to lack of blinded studies. Side effects are uncommon; transient and comparable between the two types of toxin. A clinical note at the end of this review comments on fine clinical points. Administration of BoNTs into salivary glands is currently the most effective way of treating sialorrhea.

Patient Greg Grindley communicates with host Bryant Gumbel and his wife for the first time while undergoing deep brain stimulation surgery at University Hospital's Case Medical Center in Cleveland, Ohio.
➡ Subscribe: http://bit.ly/NatGeoSubscribe
About National Geographic:
National Geographic is the world's premium destination for science, exploration, and adventure. Through their world-class scientists, photographers, journalists, and filmmakers, Nat Geo gets you closer to the stories that matter and past the edge of what's possible.
Get More National Geographic:
Official Site: http://bit.ly/NatGeoOfficialSite
Facebook: http://bit.ly/FBNatGeo
Twitter: http://bit.ly/NatGeoTwitter
Instagram: http://bit.ly/NatGeoInsta
Greg's First In-Surgery Conversation | Brain Surgery Live
https://youtu.be/zvqV_2zncNU
National Geographic
https://www.youtube.com/natgeo

Possible complications could include: Difficulty healing. Infection. Stump pain (severe pain in the remaining tissue) Phantom limb pain (a painful sensation that the foot or toe is still there) Continued spread of gangrene, requiring amputation of more areas of your foot, toes or leg. Bleeding. Nerve damage.
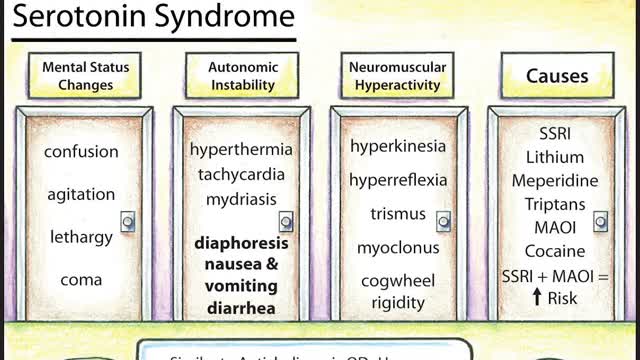
Symptoms of serotonin syndrome include a classic triad of mental status changes (eg, anxiety, delirium, confusion, restlessness), autonomic dysregulation (eg, diaphoresis, tachycardia, hypertension, hyperthermia, diarrhea, mydriasis), and neuromuscular hyperactivity (eg, hyperreflexia, tremor, rigidity, myoclonus, ocular clonus). Serotonin syndrome is clinically diagnosed and laboratory tests are used to rule out other etiologies. It usually occurs due to inadvertent interactions between drugs, therapeutic use of multiple serotonergic agents, or serotonergic medication overdose. Treatment involves discontinuation of serotonergic drugs, supportive measures, and sedation with benzodiazepines. In severe cases, a serotonin antagonist (cyproheptadine) may be used.
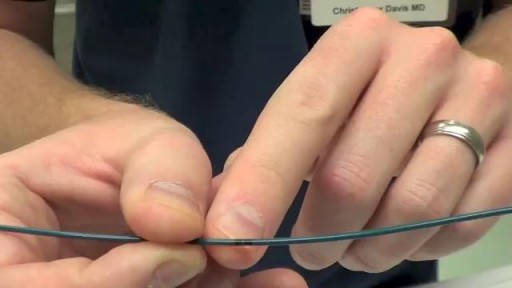
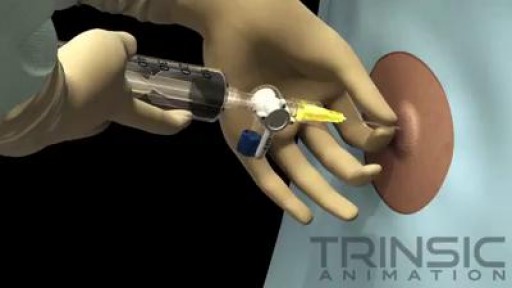
Transvenous cardiac pacing, also called endocardial pacing, is a potentially life saving intervention used primarily to correct profound bradycardia. It can be used to treat symptomatic bradycardias that do not respond to transcutaneous pacing or to drug therapy.
For strong lungs, chew 3 to 5 peppermint leaves each day. To treat congestion, add a few drops of peppermint oil to a pot of hot water and inhale the steam. You can also drink 2 cups of peppermint tea daily. To make the tea, add 1 teaspoon of dried peppermint leaves to a cup of hot water.