Top videos
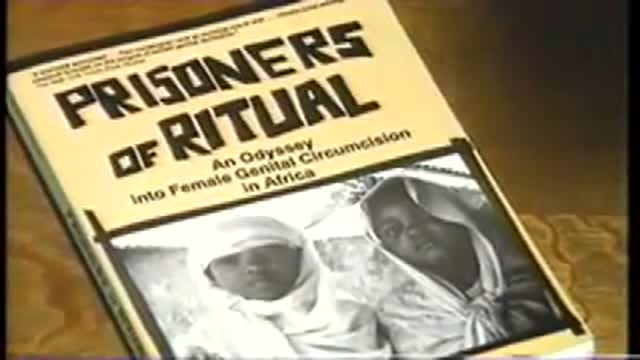
Acclaimed sexologist Hanny Lightfoot-Klein, author of several highly illuminating books on genital mutilation, discusses compromises in orgasm after male circumcision. Also commenting is cultural anthropologist James De Meo.From the groundbreaking documentary film, "Whose Body, Whose Rights?"

Watch this clinical examination video to learn how to diagnose inguinal related groin pain.
This video clip is part of the FIFA Diploma in Football Medicine and the FIFA Medical Network. To enrol or to find our more click on the following link http://www.fifamedicalnetwork.com
The Diploma is a free online course designed to help clinicians learn how to diagnose and manage common football-related injuries and illnesses. There are a total of 42 modules created by football medicine experts. Visit a single page, complete individual modules or finish the entire course.
The network provides the opportunity for clinicians around the world to meet and share ideas relating to football medicine. Ask about an interesting case, debate current practice and discuss treatment strategies. Create a profile and log on to interact with other health professionals from around the globe.
This is not medical advice. The content is intended as educational content for health care professionals and students. If you are a patient, seek care of a health care professional.

Watch as Dr. Diaz performs a tummy tuck procedure on one of our patients!
A tummy tuck, also known as abdominoplasty, removes excess fat and skin and restores weakened muscles to create a smoother, firmer abdominal profile.
This patient as well wanted to receive liposuction in conjunction with the abdominoplasty. Liposuction sometimes referred to as "lipo" by patients, slims and reshapes specific areas of the body by removing excess fat deposits and improving your body contours and proportions.
The recovery time for a tummy tuck ranges anywhere from two to six weeks. The amount of recovery time you need depends on several factors of your surgery.
If you're interested in a consultation, contact us today! 424.235.6608

Tummy Tuck ( Classic Method ) : Surgery | 3D Animation
How long does tummy tuck last?
Tummy tuck results are considered permanent, insofar that the fat cells and skin removed during an abdominoplasty cannot grow back. Likewise, the internal sutures placed to repair abdominal muscles are designed to remain in place indefinitely.
What is tummy tuck surgery?
A tummy tuck — also known as abdominoplasty — is a cosmetic surgical procedure to improve the shape and appearance of the abdomen. During a tummy tuck, excess skin and fat are removed from the abdomen. Connective tissue in the abdomen (fascia) usually is tightened with sutures as well.
How much does tummy tuck cost?
How much does it cost? It can cost from about £5,000 to £10,000 to have an abdominoplasty in the UK, plus the cost of any consultations or follow-up care.
How painful is a tummy tuck?
A tummy tuck requires significant downtime
At the beginning, you will be fatigued, swollen and sore. It is normal to have moderate pain during these first several days, although this will steadily improve. It is vital to allow yourself time to focus on rest and healing.
What is the disadvantage of tummy tuck?
The cons of a tummy tuck include: A full abdominoplasty is a major operation with a considerable recovery. Expect to postpone strenuous activities for at least 6 weeks. Results take time.
Is tummy tuck more painful than C section?
That's something many women want to know. While patients have different experiences, most plastic surgeons would agree that a cesarean section is more painful than most tummy tucks.
- Tummy tuck
- Abdominoplasty
- Abdominal tuck
- Tummy tuck procedure
- Tummy tuck process
- Tummy tuck surgery
- Tummy tuck operation
- Tummy tuck video
- Tummy tuck recovery
- Tummy tuck before and after
- Abdominoplasty surgery
- Abdominal contouring surgery
- Postpartum tummy tuck
- Post pregnancy tummy tuck
- Mini tummy tuck
- Tummy tuck cost
- Tummy tuck risks
- Tummy tuck complications
- How long does a tummy tuck take
- Tummy tuck scarring
- Tummy tuck skin removal
- Tummy tuck muscle tightening
#tummytuck
#abdominoplasty
#plastic_surgery
#cosmetic_surgery
#body_contouring
#tummy_tuck_surgery
#surgery
#cosmetic_procedure
#beauty
#health
#fitness
#medical_animation
#3d_animation
#medical_video
#explainer_video
#education

Vital signs help us assess patients in the nursing profession, and there are six common vital signs that we assess as nurses:
1. Heart Rate (Pulse)
2. Respiration Rate
3. Temperature
4. Blood Pressure
5. Pain Rating
6. Oxygen Saturation
This video will demonstrate how to check vital signs (live) on a patient, along with normal rates for each assessment. I also give you a few tips for taking vital signs as a nurse, CNA, or other healthcare profession.
🟣ABG eBook: https://registerednursern.creator-spring.com/
🟣ABG physical book: https://amzn.to/3EsF0Mc (affiliate link)
More nursing skills: https://www.youtube.com/watch?v=G5-Rp-6FMCQ&list=PLQrdx7rRsKfUhd_qQYEbp0Eab3uUKhgKb
Website: https://www.registerednursern.com/
More Videos: https://www.youtube.com/watch?v=R2XMro13dD0&list=UUPyMN8DzkFl2__xnTEiGZ1w
Nursing Gear: https://teespring.com/stores/registerednursern
Instagram: https://www.instagram.com/registerednursern_com/
Facebook: https://www.facebook.com/RegisteredNurseRNs
Twitter: https://twitter.com/NursesRN
Popular Playlists:
NCLEX Reviews: https://www.youtube.com/playli....st?list=PLQrdx7rRsKf
Fluid & Electrolytes: https://www.youtube.com/playli....st?list=PLQrdx7rRsKf
Nursing Skills: https://www.youtube.com/playli....st?list=PLQrdx7rRsKf

This video is brought to you by the Stanford Medicine 25 to teach you the common causes of shoulder pain and how to diagnose them by the physical exam.
The Stanford Medicine 25 program for bedside medicine at the Stanford School of Medicine aims to promote the culture of bedside medicine to make current and future clinicians and other healthcare provides better at the art of physical diagnosis and more confident at the bedside of their patients.
Visit us:
Website: http://stanfordmedicine25.stanford.edu/
Blog: http://stanfordmedicine25.stanford.edu/blog.html
Facebook: https://www.facebook.com/StanfordMedicine25
Twitter: https://twitter.com/StanfordMed25
Diagnoses covered in this video:
Rotator Cuff Pathology
Impingement Syndrome
Biceps Tendinopathy
Adhesive Capsulitis (Frozen Shoulder)
Acromioclavicular (AC) Joint Disease
Shoulder Instability
Labral Tears (SLAP Lesions)

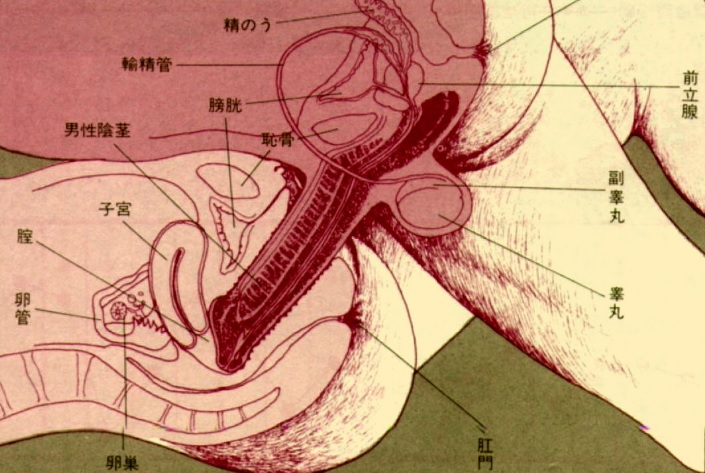
There are lots of fallacies about the missionary position being the best position for getting pregnant. With the woman on her back and her partner on top, it is thought that gravity will assist the sperm to swim upwards towards the egg.
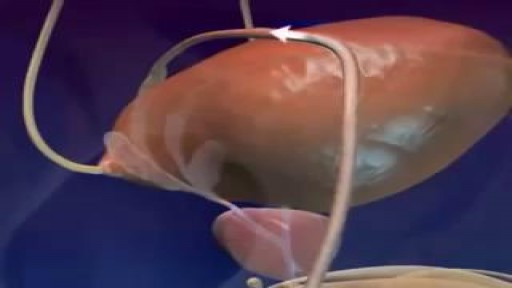
The male orgasm is a common subject but usually misunderstood at the same time. Men are sometimes led to believe that ejaculating often is a bad thing, particularly if you masturbate. The truth is that ejaculation is important to every man due to a number of reasons. The main goal of this post is to shed some light on reasons why men need to ejaculate.
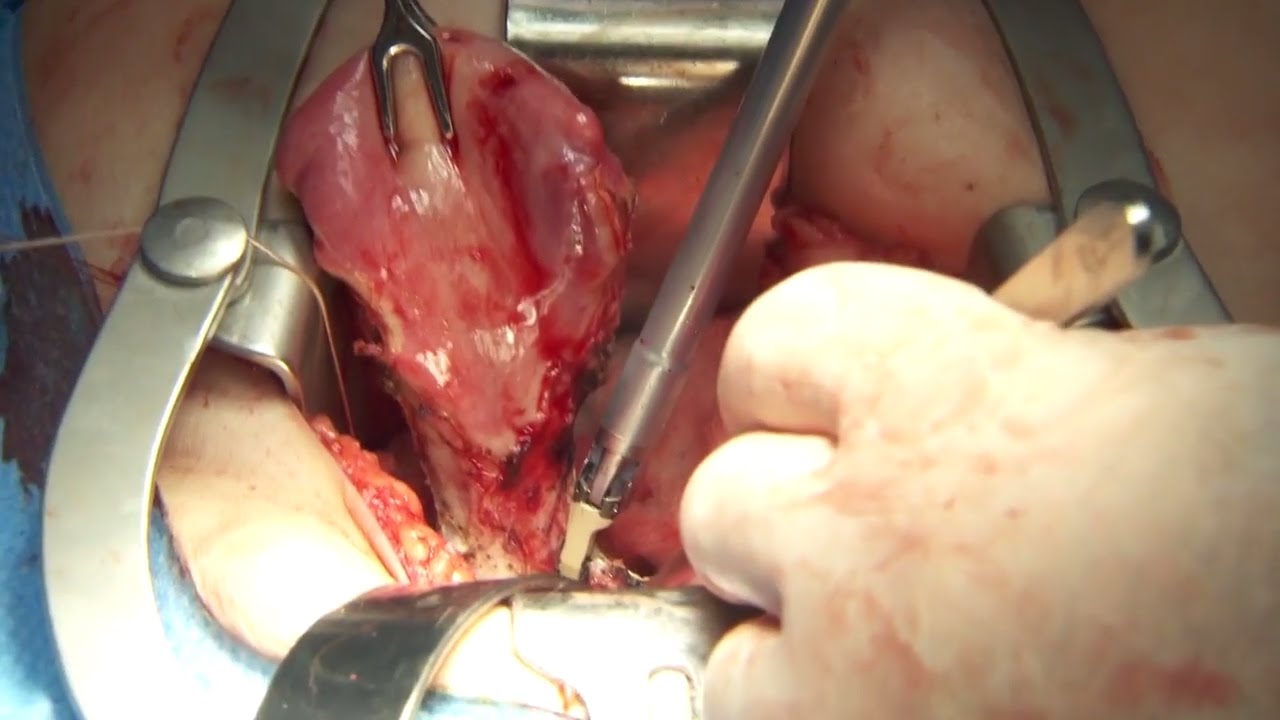
Olympus has extended the value of its award-winning combined surgical energy device, THUNDERBEAT, to open surgical procedures. Watch Dr. Francois Blaudeau master use of THUNDERBEAT Open Extended Jaw (OEJ) in a total abdominal hysterectomy.
http://medical.olympusamerica.com/products/thunderbeat?utm_source=youtube&utm_campaign=Total%20Abdominal%20Hysterectomy%20Surgery%20-%20THUNDERBEAT&utm_medium=description&utm_term=energy&utm_content=surgical
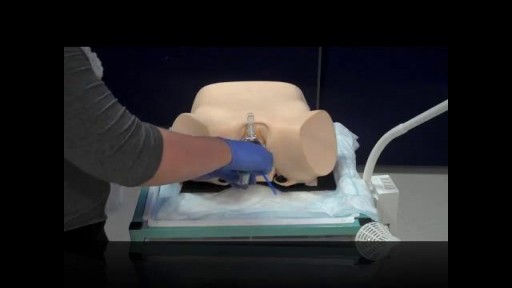
Pelvic examinations during labor are used for several purposes, among them assessment of cervical dilatation, effacement, station of the presenting part, presentation, position, and pelvic capacity.Instruction in these techniques is particularly important for those health care providers involved in labor management, including physicians, nurses, midwives, paramedics and EMT personnel.