Top videos

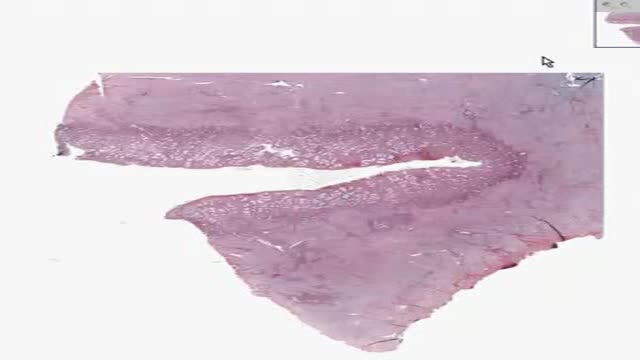
Intestinal malrotation is a developmental anomaly that occasionally causes an unusual array of symptoms in adults. The delay in diagnosis that is common in patients with malrotation frequently results in a ruptured appendix. Appendicitis should be considered when characteristic signs and symptoms are present, even if the location of abdominal pain is atypical.
A new natural painkiller based on a body-own molecule, available as supplement. An educational video on its mechanism of action: palmitoylethanolamide (PEA) is a new compound ready 4 use in the clinic to calm glia and mast cells in all states of chronic pain. Thus it focusses on 2 new targets in the treatment of pain: these extra-neuronal targets in chronic pain can be modulated by PEA.
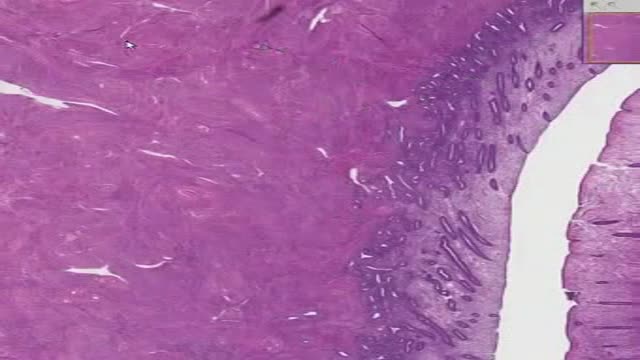
Pancreatitis is inflammation in the pancreas. The pancreas is a long, flat gland that sits tucked behind the stomach in the upper abdomen. The pancreas produces enzymes that assist digestion and hormones that help regulate the way your body processes sugar (glucose). Pancreatitis can occur as acute pancreatitis — meaning it appears suddenly and lasts for days. Or pancreatitis can occur as chronic pancreatitis, which describes pancreatitis that occurs over many years. Mild cases of pancreatitis may go away without treatment, but severe cases can cause life-threatening complications.

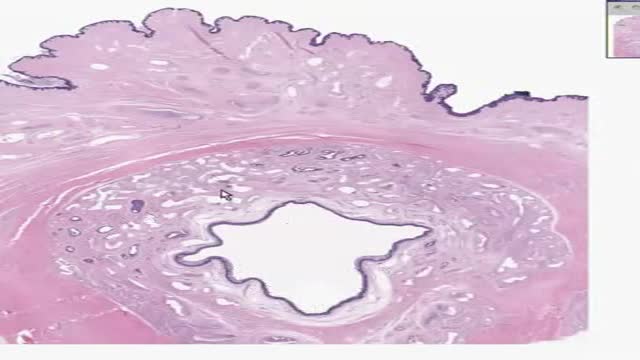
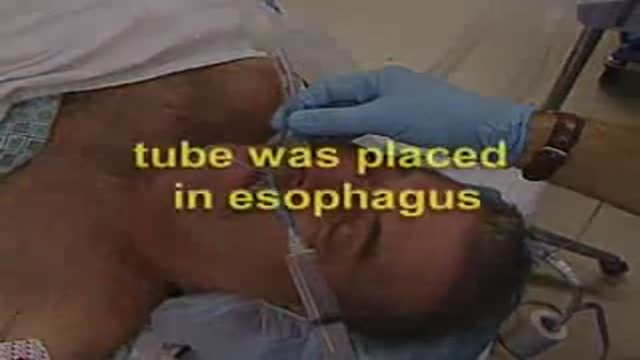
Retropharyngeal abscess (RPA) produces the symptoms of sore throat, fever, neck stiffness, and stridor. RPA occurs less commonly today than in the past because of the widespread use of antibiotics for suppurative upper respiratory infections. The incidence of RPA in the United States is rising, however. Once almost exclusively a disease of children, RPA is observed with increasing frequency in adults. It poses a diagnostic challenge for the emergency physician because of its infrequent occurrence and variable presentation.