Top videos

Homan’s sign test also called dorsiflexon sign test is a physical examination procedure that is used to test for Deep Vein Thrombosis (DVT). A positive Homan’s sign in the presence of other clinical signs may be a quick indicator of DVT. Clinical evaluation alone cannot be relied on for patient management, but when carefully performed, it remains useful in determining the need for additional testing (like D-dimer test, ultrasonography, multidetector helical computed axial tomography (CT), and pulmonary angiography) [1][2].

An untreated hepatic abscess is nearly uniformly fatal as a result of complications that include sepsis, empyema, or peritonitis from rupture into the pleural or peritoneal spaces, and retroperitoneal extension. Treatment should include drainage, either percutaneous or surgical. Antibiotic therapy as a sole treatment modality is not routinely advocated, though it has been successful in a few reported cases. It may be the only alternative in patients too ill to undergo invasive procedures or in those with multiple abscesses not amenable to percutaneous or surgical drainage. In these instances, patients are likely to require many months of antimicrobial therapy with serial imaging and close monitoring for associated complications.
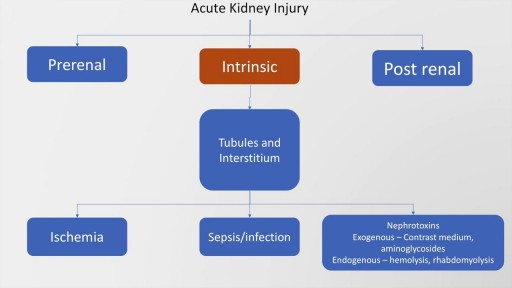
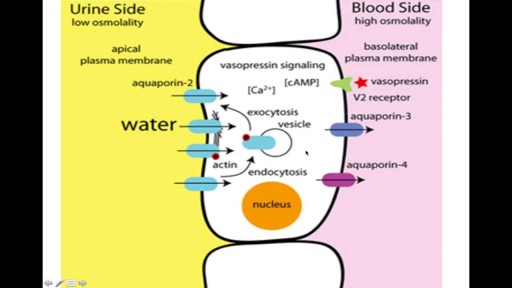
Acute kidney injury is common entity in medical practice. The present definition is based on a serum creatinine rise of more 0.3 mg/dl in 48 hours or less, a 50% increase from the baseline over a period of 07 days or a urine output of less than 0.5 ml/kg/hour for more than 06 hours. The main causes of acute kidney injury may be classified into pre renal, intrinsic or post renal causes. Rapid diagnosis and prompt treatment is essential to prevent mortality or morbidity. This presentation discusses in detail the causes of all three mechanisms, pre-renal, post renal and intrinsic.
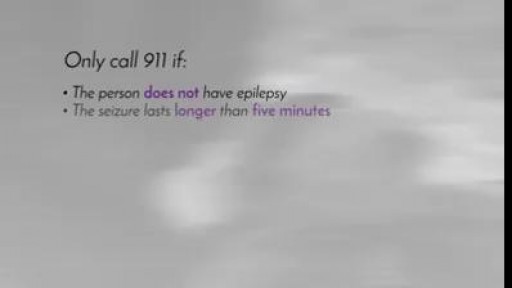
Epilepsy is the fourth most common neurological disorder and affects people of all ages Epilepsy means the same thing as "seizure disorders" Epilepsy is characterized by unpredictable seizures and can cause other health problems Epilepsy is a spectrum condition with a wide range of seizure types and control varying from person-to-person Public perception and misunderstanding of epilepsy causes challenges often worse than the seizures
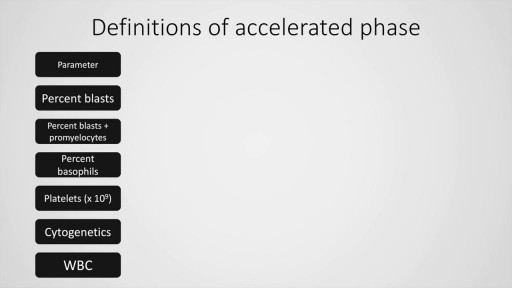
Chronic myeloid leukaemia is a common malignancy worldwide. We have come a long way from the limited treatment options and survival in this condition. Today, CML is a treatable malignancy with more than 80% patients surviving beyond 10 years after diagnosis, in absence of complications. This presentation deals with the definition, diagnostic criteria of chronic phase, accelerated and blastic phase (MD Anderson cancer centre, International bone marrow transplant registry and the WHO for the latter two) and management (first and second generation tyrosine kinase inhibitors) of this condition. Finally, a stepwise approach to chronic myeloid leukaemia is also presented including the definitive modality of treatment, allogeneic stem cell transplantation.

Sleep apnea is a potentially serious sleep disorder in which breathing repeatedly stops and starts. You may have sleep apnea if you snore loudly, and you feel tired even after a full night's sleep. The main types of sleep apnea are: Obstructive sleep apnea, the more common form that occurs when throat muscles relax. Central sleep apnea, which occurs when your brain doesn't send proper signals to the muscles that control breathing. Complex sleep apnea syndrome, also known as treatment-emergent central sleep apnea, occurs when someone has both obstructive sleep apnea and central sleep apnea. If you think you might have any form of sleep apnea, see your doctor. Treatment can ease your symptoms and may help prevent heart problems and other complications.