Top videos
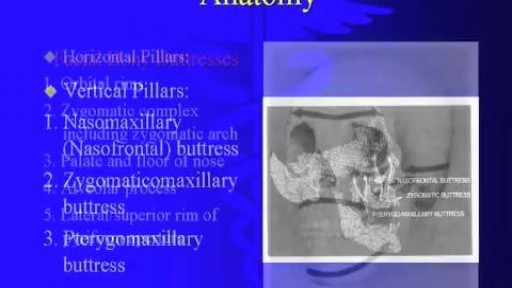
Reconstructive surgery is performed to treat structures of the body affected aesthetically or functionally by congenital defects, developmental abnormalities, trauma, infection, tumors or disease. It is generally done to improve function and ability, but may also be performed to achieve a more typical appearance of the affected structure. Reconstructive surgery is generally covered by most health insurance policies, although coverage for specific procedures and levels of coverage may vary greatly.

Hardware removals are among the most commonly performed surgical procedures worldwide. Current literature offers little data concerning postoperative patient satisfaction. The purpose of our study was to evaluate the patients’ point of view on implant removal. watch to learn more.

Choking occurs when a foreign object becomes lodged in the throat or windpipe, blocking the flow of air. In adults, a piece of food often is the culprit. Young children often swallow small objects. Because choking cuts off oxygen to the brain, administer first aid as quickly as possible. The universal sign for choking is hands clutched to the throat. If the person doesn't give the signal, look for these indications: Inability to talk Difficulty breathing or noisy breathing Inability to cough forcefully Skin, lips and nails turning blue or dusky Loss of consciousness
There are many exciting milestones that accompany growing older with Down syndrome, old age can also bring unexpected challenges for which adults with Down syndrome, their families and caregivers.
www.homecareassistanceyork.com
Liposuction surgery is used to reduce the extra fat from your body with the very safe surgical process but you must consult with your Surgeon first when deciding about using this surgery to meet your body fat needs.
Vaser Lipo was Rs. 65000 per region. Now at Rs. 50,000 per Region
Offer valid till 31st March only
Vaser Liposuction technology helps to reduce the healing time and increase effective skin contraction, giving you smooth, slim results. With Liposuction there are no stitches, only a single 1cm small incision giving you permanent large result.
For further information, are available visit our website:
http://www.imageclinic.org/liposuction.html
Your Query for Chat and call +91-9818369662, 9958221983 (WhatsApp)

Bipolar disorder, formerly called manic depression, is a mental health condition that causes extreme mood swings that include emotional highs (mania or hypomania) and lows (depression). When you become depressed, you may feel sad or hopeless and lose interest or pleasure in most activities. When your mood shifts to mania or hypomania (less extreme than mania), you may feel euphoric, full of energy or unusually irritable. These mood swings can affect sleep, energy, activity, judgment, behavior and the ability to think clearly. Episodes of mood swings may occur rarely or multiple times a year. While most people will experience some emotional symptoms between episodes, some may not experience any. Although bipolar disorder is a lifelong condition, you can manage your mood swings and other symptoms by following a treatment plan. In most cases, bipolar disorder is treated with medications and psychological counseling (psychotherapy).