Top videos

Repairing a myelomeningocele in utero, rather than after birth, reduces the risk for fetal or neonatal death and the need for shunting by age 1 and substantially improves neurologic and motor outcomes. However, it is not without maternal and fetal risks. These are the findings, in a nutshell, of the long-awaited Management of Myelomeningocele Study (MOMS), which were published online February 9 in The New England Journal of Medicine.
How To Lose Weight In A Week, How To Lose Fat Without Exercise, Diets That Work Fast
http://lose-weight-without-gym.info-pro.co
3 Ways For Fast Weight Loss
There are many people who would like to reduce their weight very fast sitting at home; cost is a constraint when it comes to reducing your weight, so membership in a health club or a weight reduction center is out of question for many people.
The ways of weight loss at home fast is not a rocket science exertion rather it’s like an open book. The most important rules are taking a balanced diet which is rich in fiber, cutting of carbohydrates from the meals and planning out exercises and work outs properly.
The following section discusses these 3 simple yet effective ways of weight loss.
How to train your brain to lose pounds
Click Here: http://lose-weight-without-gym.info-pro.co
Click The Link Below To Check It Out
http://lose-weight-without-gym.info-pro.co
Subscribe To Our Channel
https://www.youtube.com/user/NaturalFatBurners1
https://www.youtube.com/watch?v=EcicJ5J-C7U
How To Lose Weight In A Week, How To Lose Fat Without Exercise, Diets That Work Fast,
gym workout to lose weight,
how to lose weight in gym,
losing weight at the gym,
best workout for losing weight,
best gym workout to lose weight,
how to lose weight permanently,
how can you lose weight in a week,
great exercises to lose weight,
what is the best workout to lose weight,
what are the best exercises to lose weight

Depending on the fracture, the bone fragments may be fixed using screws, a plate and screws, or different wiring techniques. Because there is such a wide range of injuries, there is also a wide range of people's specific recovery time for ankle fracture surgery. It takes at least 6 weeks for the broken bones to heal.
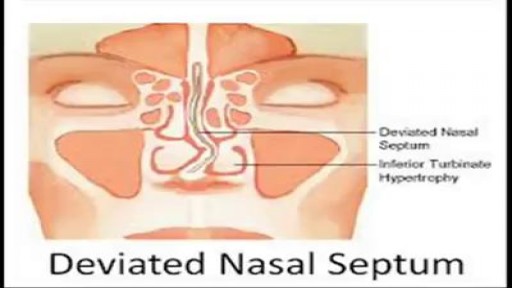
When a deviated septum is severe, it can block one side of your nose and reduce airflow, causing difficulty breathing. The additional exposure of a deviated septum to the drying effect of airflow through the nose may sometimes contribute to crusting or bleeding in certain individuals. Nasal obstruction can occur from a deviated nasal septum, from swelling of the tissues lining the nose, or from both. Treatment of nasal obstruction may include medications to reduce the swelling or nasal dilators that help open the nasal passages. To correct a deviated septum, surgery is necessar

Labia minoraplasty is an elective procedure that can reduce the size and reshape the inner vaginal lips. Large or asymmetrical labia minora can leave you feeling self-conscience in tight clothing or during intimacy. Long labia may result in rubbing, irritation or discomfort during intercourse and exercise. Certain skin conditions can cause increased sensitivity or tearing of the labia minora. In some cases, the labia minora may be fused with tissue in the labia majora and require medical correction.

A Pfannenstiel incision /ˈfɑːnᵻnʃtiːl/ is a type of abdominal surgical incision that allows access to the abdomen. It is used for gynecologic and orthopedics surgeries, and it is the most common method for performing Caesarian sections today.
There are many exciting milestones that accompany growing older with Down syndrome, old age can also bring unexpected challenges for which adults with Down syndrome, their families and caregivers.
www.homecareassistanceyork.com
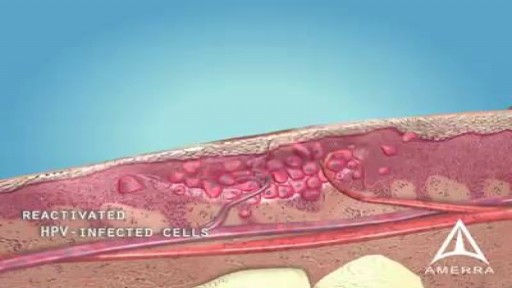
A wart is a skin growth caused by some types of the virus called the human papillomavirus (HPV). HPV infects the top layer of skin, usually entering the body in an area of broken skin. The virus causes the top layer of skin to grow rapidly, forming a wart. Most warts go away on their own within months or years.