Top videos
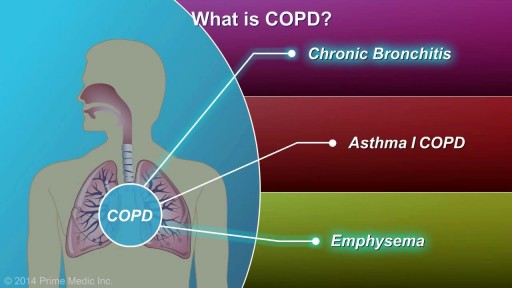
COPD, or chronic obstructive pulmonary disease, is a progressive disease that makes it hard to breathe. Progressive means the disease gets worse over time. COPD can cause coughing that produces large amounts of a slimy substance called mucus, wheezing, shortness of breath, chest tightness, and other symptoms. Cigarette smoking is the leading cause of COPD. Most people who have COPD smoke or used to smoke. However, up to 25 percent of people with COPD never smoked. Long-term exposure to other lung irritants—such as air pollution, chemical fumes, or dusts—also may contribute to COPD. A rare genetic condition called alpha-1 antitrypsin (AAT) deficiency can also cause the disease.

Squamous cell carcinomas typically appear as persistent, thick, rough, scaly patches that can bleed if bumped, scratched or scraped. They often look like warts and sometimes appear as open sores with a raised border and a crusted surface. In addition to the signs of SCC shown here, any change in a preexisting skin growth, such as an open sore that fails to heal, or the development of a new growth, should prompt an immediate visit to a physician.

Sleep apnea is a potentially serious sleep disorder in which breathing repeatedly stops and starts. You may have sleep apnea if you snore loudly, and you feel tired even after a full night's sleep. The main types of sleep apnea are: Obstructive sleep apnea, the more common form that occurs when throat muscles relax. Central sleep apnea, which occurs when your brain doesn't send proper signals to the muscles that control breathing. Complex sleep apnea syndrome, also known as treatment-emergent central sleep apnea, occurs when someone has both obstructive sleep apnea and central sleep apnea. If you think you might have any form of sleep apnea, see your doctor. Treatment can ease your symptoms and may help prevent heart problems and other complications.

The principal signs of cerebellar dysfunction are the following: Ataxia: unsteadiness or incoordination of limbs, posture, and gait. A disorder of the control of force and timing of movements leading to abnormalities of speed, range, rhythm, starting, and stopping.

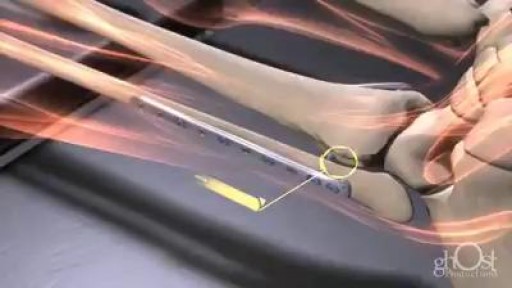
The Ortolani method is an examination method that identifies a dislocated hip that can be reduced into the socket (acetabulum). Ortolani described the feeling of reduction as a “Hip Click” but the translation from Italian was interpreted a sound instead of a sensation of the hip moving over the edge of the socket when it re-located. After the age of six weeks, this sensation is rarely detectable and should not be confused with snapping that is common and can occur in stable hips when ligaments in and around the hip create clicking noises. When the Ortolani test is positive because the hip is dislocated, treatment is recommended to keep the hip in the socket until stability has been established

In breech position, the baby's bottom is down. There are a few types of breech: Complete breech means the baby is bottom-first, with knees bent. Frank breech means the baby's legs are stretched up, with feet near the head. Footling breech means one leg is lowered over the mother's cervix. You are more likely to have a breech baby if you: Go into early labor Have an abnormally shaped uterus, fibroids, or too much amniotic fluid Have more than one baby in your womb Have placenta previa (when the placenta is on the lower part of the uterine wall, blocking the cervix)
Hodgkin lymphoma has characteristics that distinguish it from other diseases classified as lymphoma, including the presence of Reed-Sternberg cells. These are large, cancerous cells found in Hodgkin lymphoma tissues, named for the scientists who first identified them. Hodgkin lymphoma is one of the most curable forms of cancer. NHL represents a diverse group of diseases distinguished by the characteristics of the cancer cells associated with each disease type. Most people with NHL have a B-cell type of NHL (about 85 percent). The others have a T-cell type or an NK-cell type of lymphoma. Some patients with fast-growing NHL can be cured. For patients with slow-growing NHL, treatment may keep the disease in check for many years.
Rhabdomyolysis is a condition in which damaged skeletal muscle (Ancient Greek: rhabdomyo-) tissue breaks down rapidly (Greek –lysis). This damage may be caused by physical (e.g. crush injury), chemical, or biological factors. Breakdown products of damaged muscle cells are released into the bloodstream; some of these, such as the protein myoglobin, are harmful to the kidney and may lead to kidney dysfunction. The severity of the symptoms (which may include muscle pains, vomiting and confusion) depends on the extent of the muscle damage, and whether kidney failure develops. The mainstay of treatment is generous intravenous fluids, but could include dialysis or hemofiltration.
Rhabdomyolysis and its complications are significant problems for those injured in disasters such as earthquakes and bombing. Relief efforts in areas struck by earthquakes often include medical teams with skills and equipment for treatment of survivors with rhabdomyolysis. The disease and its mechanisms were first fully elucidated during the Blitz of London in 1941.