Top videos
http://smoking-videos.plus101.com
Quit Smoking Forever Formula Videos - How To Quit Smoking In As Fast As 1 Week Without Agitation, Cravings Or Withdrawal Symptoms.You're about to uncover the 3 elements that will rapidly boost your chances of success to quit smoking and not only that, you'll learn ways to escape cravings and how to avoid a relapse that can happen in the future even to people with the most willpower.
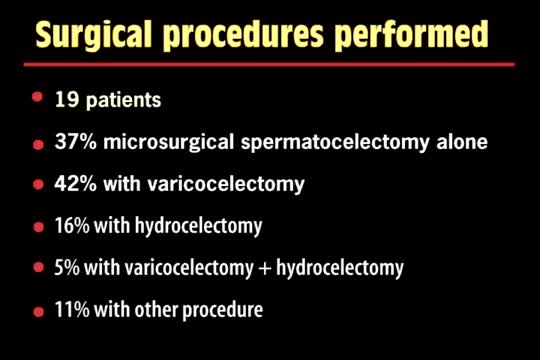
A spermatocelectomy is surgery to remove a spermatocele. A spermatocele is a cyst (sac of fluid) that contains sperm. It forms inside your scrotum on the outside of your testicle. The cyst is most often attached to your epididymis. The epididymis is a tube that stores sperm.

This video shows you how to examine the hand and wrist and how to identify common causes of pain.
This video clip is part of the FIFA Diploma in Football Medicine and the FIFA Medical Network. To enrol or to find our more click on the following link http://www.fifamedicalnetwork.com
The Diploma is a free online course designed to help clinicians learn how to diagnose and manage common football-related injuries and illnesses. There are a total of 42 modules created by football medicine experts. Visit a single page, complete individual modules or finish the entire course.
The network provides the opportunity for clinicians around the world to meet and share ideas relating to football medicine. Ask about an interesting case, debate current practice and discuss treatment strategies. Create a profile and log on to interact with other health professionals from around the globe.
This is not medical advice. The content is intended as educational content for health care professionals and students. If you are a patient, seek care of a health care professional.
If it is not removed, tooth decay will begin. The acids in plaque damage the enamel covering your teeth. It also creates holes in the tooth called cavities. Cavities usually do not hurt, unless they grow very large and affect nerves or cause a tooth fracture.

***SUBSCRIBE WITHIN THE NEXT 28 DAYS FOR A CHANCE TO WIN $1,000!***
Did you know only 20% of our video content is on YouTube? Try out our membership for FREE today! → https://bit.ly/3mWibYe
Try our NCLEX Prep FREE → https://bit.ly/3xYAOkT
Head to https://bit.ly/3mWibYe to get access to the other 80%, along with 800+ study guides, customizable quiz banks with 3,000+ test-prep questions, and answer rationales!
Popular Playlists:
NCLEX Fluid & Electrolytes: https://bit.ly/39BSHXs
Heart Failure (CHF): https://bit.ly/2u5zfDm
Myocardial Infarction (MI): https://bit.ly/3bN9AAk
Addison’s vs. Cushing: https://bit.ly/2STvute
Diabetes Mellitus & DKA vs HHNS: https://bit.ly/37D8nbs
Cardiomyopathy: https://bit.ly/38CwcSg
IV Fluids: Hypertonic, Hypotonic & Isotonic: https://bit.ly/2P45BWx
SIADH vs Diabetes Insipidus: https://bit.ly/2wq6Bhb
Follow us on social media for more EXCLUSIVE content 👋
More Videos: https://bit.ly/37CRttH
Instagram: https://www.instagram.com/simplenursing.com_
TikTok: https://www.tiktok.com/simplenursing
Thank you for the support & for tuning in!
Remember… don’t be scared, BE PREPARED!
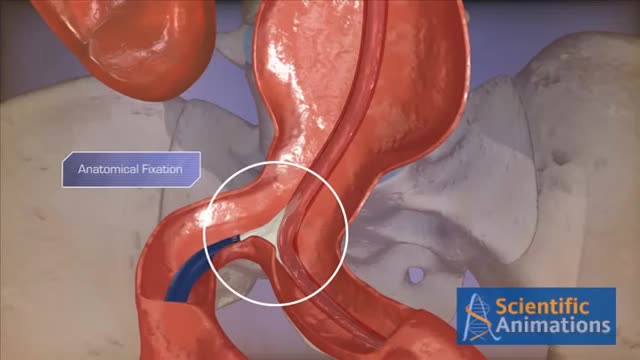
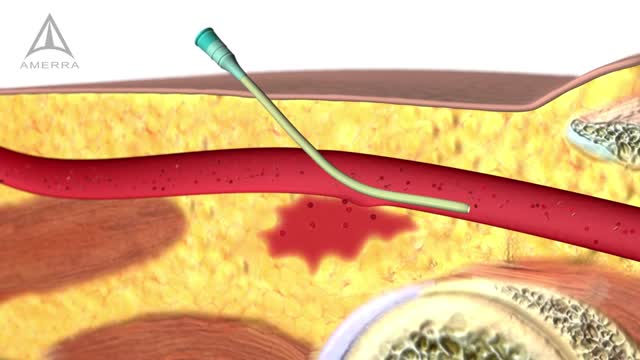
Abdominal aortic aneurysms can weaken the aorta, your body’s largest blood vessel. This can develop into a potentially serious heath problem that can be fatal if the aneurysm bursts, causing massive internal bleeding. Endovascular stent grafting, or endovascular aneurysm repair (EVAR), is a newer form of treatment for abdominal aortic aneurysm that is less invasive than open surgery. Endovascular stent grafting uses an endovascular stent graft to reinforce the wall of the aorta and to help keep the damaged area from rupturing.

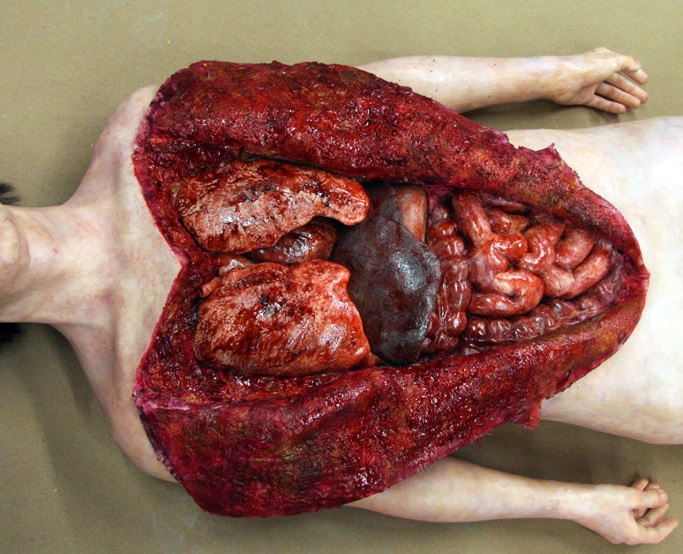
A 76 year-old, female, presented with a three day history of melena without any abdominal pain. She had one episode of hematemesis (about 100 ml blood) in the emergency room, patient has a strong alcoholic drink abuse.
An upper endoscopy with magnification was performed.
multiple ulcers were detected across of the gastric camera,
esophageal varices was also detected

Biceps tenodesis surgery is performed when the biceps tendon is damaged, or the rotator cuff tendon or cartilage ring in the shoulder is torn. The biceps tendon is a strong rope‐like structure connecting the upper end of the biceps muscle to the bones in the shoulder. In biceps tenodesis surgery, the biceps tendon is separated from the shoulder and reattached to the humerus, or the upper arm bone.