Top videos

A renal biopsy is a procedure used to extract kidney tissue for laboratory analysis. The word “renal” describes the kidneys. A renal biopsy is also called a kidney biopsy. The test helps your doctor identify the type of kidney disease you have, how severe it is, and the best treatment for it.
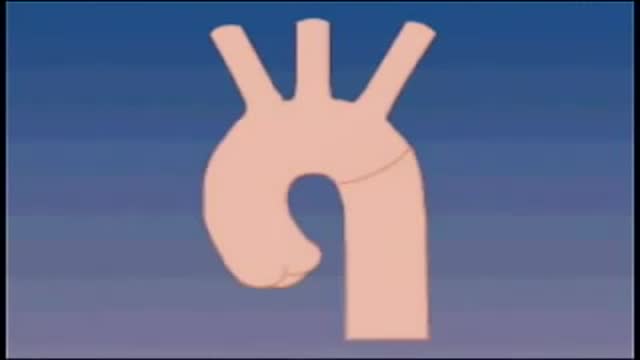
Although the exact cause of abdominal aortic aneurysms is unknown, a number of factors may play a role, including: Tobacco use. ... Hardening of the arteries (atherosclerosis). ... High blood pressure. ... Blood vessel diseases in the aorta. ... Infection in the aorta. ... Trauma. ... Heredity.
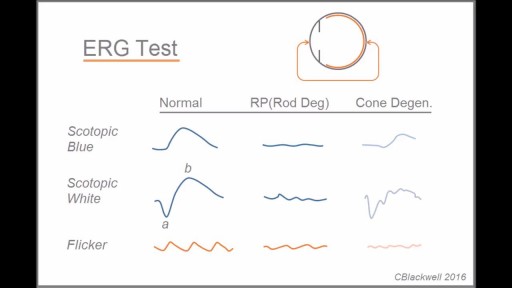
Retinitis pigmentosa is a rare, inherited degenerative eye disease that causes severe vision impairment. Symptoms often begin in childhood. They include decreased vision at night or in low light and loss of side vision (tunnel vision). There's no effective treatment for this condition. Wearing sunglasses may help protect remaining vision.

Occiput or cephalic — the baby's head is down, and the baby is facing the mother's abdomen. This position results in back pain and a prolonged labor. Transverse — the baby is lying crosswise in the uterus, side-to-side over the mother's pelvis, in a horizontal position rather than vertical.

Bone marrow biopsy and bone marrow aspiration are procedures to collect and examine bone marrow — the spongy tissue inside some of your larger bones. Bone marrow biopsy and aspiration can show whether your bone marrow is healthy and making normal amounts of blood cells. Doctors use these procedures to diagnose and monitor blood and marrow diseases, including some cancers, as well as fevers of unknown origin. Bone marrow has a fluid portion and a more solid portion. In bone marrow biopsy, your doctor uses a needle to withdraw a sample of the solid portion. In bone marrow aspiration, a needle is used to withdraw a sample of the fluid portion.
Lack of sunshine causes skin cancer, according to Andreas Moritz. In this video from 2009, he explains why being in the sun is actually good for you and your skin. Find out why your sunscreen is doing more harm than good. Also, you need vitamin D to prevent cancer, and sunscreen may interfere with your exposure to vitamin D from the sun.

💪 Get our Knee Resilience program here: https://e3rehab.com/programs/r....esilience/knee-resil
In this video, I will walk you through a comprehensive rehab program for the most commonly injured knee ligament - the MCL.
💪 PROGRAMS: https://e3rehab.com/programs/
📩 MAILING LIST (exclusive deals, offers, and information): https://e3rehab.com/newsletter/
🏆 COACHING: https://e3rehab.com/coaching/
📝 ARTICLES: https://e3rehab.com/articles/
👕 APPAREL: https://e3rehab.com/clothing/
🎧 PODCAST: https://open.spotify.com/show/....5ZbaI145Bk94Guq7olMJ
AFFILIATES:
👟 Vivo Barefoot: Get 15% off all shoes! - https://www.vivobarefoot.com/e3rehab
📓 MASS (Monthly Research Review): http://bit.ly/E3MASS
📚 CSMi: https://humacnorm.com/e3rehab
🏋️ GYM EQUIPMENT: https://e3rehab.com/affiliates/
Follow Us:
YOUTUBE: https://www.youtube.com/@e3reh....ab?sub_confirmation=
INSTAGRAM: https://www.instagram.com/e3rehab
TWITTER: https://twitter.com/E3Rehab
FACEBOOK: https://www.facebook.com/e3rehab
TIKTOK: https://www.tiktok.com/@e3rehab
Intro (0:00)
Anatomy & Function (0:08)
Classification (1:11)
Treatment Options (1:46)
Bracing (3:30)
Rehab Overview (4:28)
Early Stage (5:27)
Mid-Stage(8:50)
Late Stage/Return to Sport (21:14)
Programming (22:13)
Summary (23:47)
---
Disclaimer: The information presented is not intended as medical advice or to be a substitute for medical counseling but intended for entertainment purposes only. If you are experiencing pain, please seek the appropriate healthcare professional.

Otto Placik MD. a board certified Chicago Illinois based plastic surgeon presents instructional video on post genital surgery (labia minora reduction aka labiaplasty or labioplasty or clitoral hood reduction) massage exercises for treatment of labum minora psot surgical fibrosis or hypersensitivity. Photos pictures and video of anatomic models are reviewed . Great for patients thinking about or planning labiaplasty or vaginal cosmetic surgery

MotionLit can help you multiply the value of your case by portraying the mechanisms of injuries in a 3D Accident Reconstruction Animation. Call (855)850-0650 or visit motionlit.com to learn & earn more for your client!
MotionLit is a one-stop-shop for litigators, offering complete trial services from video production, animation, litigation support, exhibit design, trial technician, and video depositions. Our visuals have proven to help attorneys obtain record-breaking verdicts with our persuasive trial presentations, settlement documentaries, and demonstratives.
Contact Us At:
www.motionlit.com
(213) 291 9141
info@motionlit.com
Follow Us On:
Twitter: @motionlit
Instagram: https://www.instagram.com/motionlit/
Facebook: https://www.facebook.com/MotionLit/
If it is not removed, tooth decay will begin. The acids in plaque damage the enamel covering your teeth. It also creates holes in the tooth called cavities. Cavities usually do not hurt, unless they grow very large and affect nerves or cause a tooth fracture.