Top videos

Epilepsy surgery is reserved for people whose seizures are not well controlled by seizure medicines. This situation is sometimes called being "medically refractory" or "drug resistant." In children, the definition of medically refractory is even more individualized to the specific child's situation. Surgery may be considered for some children after weeks to months of treatment with seizure medicines.

A peritonsillar abscess forms in the tissues of the throat next to one of the tonsils. An abscess is a collection of pus that forms near an area of infected skin or other soft tissue. The abscess can cause pain, swelling, and, if severe, blockage of the throat. If the throat is blocked, swallowing, speaking, and even breathing become difficult. When an infection of the tonsils (known as tonsillitis) spreads and causes infection in the soft tissues, a peritonsillar abscess may result. Peritonsillar abscesses are generally uncommon. When they do occur they are more likely among young adults, adolescents, and older children.

Rhinoplasty enhances facial harmony and the proportions of your nose. It can also correct impaired breathing caused by structural defects in the nose. Rhinoplasty surgery can change: Nose size in relation to facial balance Nose width at the bridge or in the size and position of the nostrils Nose profile with visible humps or depressions on the bridge Nasal tip that is enlarged or bulbous, drooping, upturned or hooked Nostrils that are large, wide, or upturned Nasal asymmetry If you desire a more symmetrical nose, keep in mind that everyone’s face is asymmetric to some degree. Results may not be completely symmetric, although the goal is to create facial balance and correct proportion.

Function and Anatomy: The hip is a ball and socket type joint, formed by the articulation of the head of the femur with the pelvis. Normal range of motion includes: abduction 45 degrees, adduction 20-30 degrees, flexion 135 degrees, extension 30 degrees, internal and external rotation. Hip pathology can cause symptoms anywhere around the joint, though frequently pain is anterior and radiates to the groin region. Additionally, pathology outside of the hip can be referred to this region. History and exam obviously help in making these distinctions.

Function and Anatomy:
Hinge type joint formed by the articulation of the Ulna and Radius (bones of the forearm), and Humerus (upper arm). Full extension is equal to 0 degrees, full flexion to ~ 150 degrees. Maximum supination (turning hand palm up so that it can hold a bowl of "soup") and pronation (palm down) are both 90 degrees
26 years old man lost his right hand thumb and index fingers with an industrial machine.the thumb amputated part was not found. the thumb is much more important of any other finger in the hand and should be reconstructed by any means. so the index amputated part was filleted and replanted over the thumb stump. the video is taken 1 year after replantation. You can see another videos in my site: https://drliaghatclinic.com, https://instagram.com/liaghatclinic, https://t.me/liaghatclinic

Learn Basic Laparoscopic Surgery, the components of a laparoscopic surgical setup, optimal positioning and ergonomics in laparoscopic surgery, and much more. Check out the full course for free here: https://www.incision.care/free-trial
What is Laparoscopic Surgery:
Laparoscopic surgery describes procedures performed using one or multiple small incisions in the abdominal wall in contrast to the larger, normally singular incision of laparotomy. The technique is based around principles of minimally invasive surgery (or minimal access surgery): a large group of modern surgical procedures carried out by entering the body with the smallest possible damage to tissues. In abdominopelvic surgery, minimally invasive surgery is generally treated as synonymous with laparoscopic surgery as are procedures not technically within the peritoneal cavity, such as totally extraperitoneal hernia repair, or extending beyond the abdomen, such as thoraco-laparoscopic esophagectomy. The term laparoscopy is sometimes used interchangeably, although this is often reserved to describe a visual examination of the peritoneal cavity or the purely scopic component of a laparoscopic procedure. The colloquial keyhole surgery is common in non-medical usage.
Surgical Objective of Laparoscopic Surgery:
The objective of a laparoscopic approach is to minimize surgical trauma when operating on abdominal or pelvic structures. When correctly indicated and performed, this can result in smaller scars, reduced postoperative morbidity, shorter inpatient durations, and a faster return to normal activity. For a number of abdominopelvic procedures, a laparoscopic approach is now generally considered to be the gold-standard treatment option.
Definitions
Developments of Laparoscopic Surgery:
Following a number of smaller-scale applications of minimally invasive techniques to abdominopelvic surgery, laparoscopic surgery became a major part of general surgical practice with the introduction of laparoscopic cholecystectomy in the 1980s and the subsequent pioneering of endoscopic camera technology. This led to the widespread adoption of the technique by the early- to mid-1990s. The portfolio of procedures that can be performed laparoscopically has rapidly expanded with improvements in instruments, imaging, techniques and training — forming a central component of modern surgical practice and cross-specialty curricula [2]. Techniques such as laparoscopically assisted surgery and hand-assisted laparoscopic surgery have allowed the application of laparoscopic techniques to a greater variety of pathology. Single-incision laparoscopic surgery, natural orifice transluminal endoscopic surgery, and minilaparoscopy-assisted natural orifice surgery continue to push forward the applications of minimally invasive abdominopelvic techniques; however, the widespread practice and specific indications for these remain to be fully established. More recently, robotic surgery has been able to build on laparoscopic principles through developments in visualization, ergonomics, and instrumentation.
This Basic Laparoscopic Surgery Course Will Teach You:
- Abdominal access techniques and the different ways of establishing a pneumoperitoneum
- Principles of port placement and organization of the operative field
- Key elements of laparoscopic suturing, basic knotting and clip application
Specific attention is paid to the following hazards you may encounter:
- Fire hazard and thermal injury
- Lens fogging
- Contamination of insufflation system
- Complications from trocar introduction
- Limitations of Veress needle technique
- Limitations of open introduction technique
- Complications of the pneumoperitoneum
- Gas embolism
- Mirroring and scaling of instrument movements
- Firing clip applier without a loaded clip
The following tips are designed to improve your understanding and performance:
- Anatomy of a laparoscope
- Checking for optic fiber damage
- "White balance" of camera
- Checking integrity of electrosurgical insulation
- Access at Palmer's point
- Lifting abdominal wall before introduction
- Confirming position of Veress needle
- Umbilical anatomy
- Identification of inferior epigastric vessels under direct vision
- Translumination of superficial epigastric vessels
- Selection of trocar size
- Aiming of trocar
- Working angles in laparoscopic surgery
- Choice of suture material
- Instruments for suturing
- Optimal ergonomics for suturing
- Extracorporeal needle positioning
- Optimal suture lengths
- "Backloading" needle
- Intracorporeal needle positioning
- Hand movements when suturing
- Optimal positioning of scissors
- Extracorporeal knot tying
- Visualization of clip applier around target structure
- Common clip configurations
http://smoking-videos.plus101.com
Quit Smoking Forever Formula Videos - How To Quit Smoking In As Fast As 1 Week Without Agitation, Cravings Or Withdrawal Symptoms.You're about to uncover the 3 elements that will rapidly boost your chances of success to quit smoking and not only that, you'll learn ways to escape cravings and how to avoid a relapse that can happen in the future even to people with the most willpower.

How Does a Bone Heal? All broken bones go through the same healing process. This is true whether a bone has been cut as part of a surgical procedure or fractured through an injury. The bone healing process has three overlapping stages: inflammation, bone production and bone remodeling. Inflammation starts immediately after the bone is fractured and lasts for several days. When the bone is fractured, there is bleeding into the area, leading to inflammation and clotting of blood at the fracture site. This provides the initial structural stability and framework for producing new bone. Diagram of inflammation in a fractured bone Bone production begins when the clotted blood formed by inflammation is replaced with fibrous tissue and cartilage (known as soft callus). As healing progresses, the soft callus is replaced with hard bone (known as hard callus), which is visible on x-rays several weeks after the fracture. Bone remodeling, the final phase of bone healing, goes on for several months. In remodeling, bone continues to form and becomes compact, returning to its original shape. In addition, blood circulation in the area improves. Once adequate bone healing has occurred, weightbearing (such as standing or walking) encourages bone remodeling.

Rhode Island Hospital's outpatient dialysis program cares for patients with chronic kidney disease. Learn more about the program, which includes a new, state of the art dialysis center in East Providence. http://www.rhodeislandhospital.....org/outpatient-dial

What goes into providing anesthesia for cardiac surgery where a patient's heart is completely arrested? In this video, I take you into the operating room during a surgery and talk with Dr. Benji Salter, program director for Mt. Sinai Hospital's cardiothoracic anesthesiology fellowship program.
While no patient information is shown in this video, the patient did provide written consent for filming to occur during surgery. Permission was also obtained from Mount Sinai Hospital's Department of Anesthesiology as well as the hospital's Press Office.
Chapters
0:00 Start
0:44 Surgery background
1:40 Case preparation
2:45 Anesthesia equipment
6:21 Echocardiography
7:16 Preparing for bypass
8:34 Stopping the heart
9:06 Fellowship
10:46 Why cardiac anesthesia?
11:52 Coming off of bypass
13:06 Post-op recovery
The information in this video is not intended nor implied to be a substitute for professional medical advice, diagnosis or treatment. All content, including text, graphics, images, and information, contained in this video is for general information purposes only and does not replace a consultation with your own doctor/health professional.
#Anesthesiology #Residency #MedicalSchool
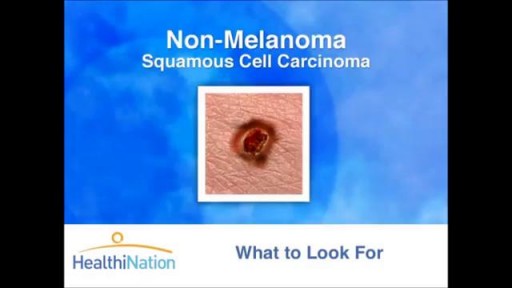
The Skin Cancer Foundation, founded in 1979 by dermatologist and Mohs surgeon Perry Robins, MD, is a global organization solely devoted to educating the public and medical community about skin cancer prevention, early detection, and treatment

Brachytherapy or localized radiation treatment can be used in certain patients with breast cancer. Depending on tumor size and other factor, physicians may use APBI or accelerated partial breast irradiation. Dr. Elizabeth Tapen, a radiation oncologist, reviews brachytherapy for breast cancer.
Renal replacement therapies are a set of interventions and techniques aimed at replacement of the filtering function of the kidneys. These include both dialysis and renal transplant. In this presentation we will talk about the indication and modalities of dialysis. This includes hemodialysis, peritoneal dialysis and continuous renal replacement therapies. The circuit diagram of each modalities along with its procedure and complications are also discussed.
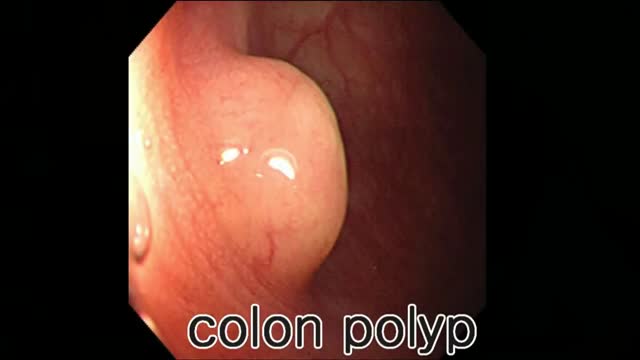
Colon polyp facts Colon polyps are growths on the inner lining of the colon and are very common. Colon polyps are important because they may be, or may become malignant (cancerous). They also are important because based on their size, number, and microscopic anatomy (histology); they can predict which patients are more likely to develop more polyps and colon cancer. Changes in the genetic material of cells lining the colon are the cause of polyps. There are different types of colon polyps with differing tendencies to become malignant and abilities to predict the development of more polyps and cancer. It is important to recognize families with members who have familial genetic conditions causing polyps because some of these conditions are associated with a very high incidence of colon cancer, and the cancer can be prevented or discovered early.