Top videos
University of California, Berkeley engineers have built the first dust-sized, wireless sensors that can be implanted in the body, bringing closer the day when a Fitbit-like device could monitor internal nerves, muscles or organs in real time.
There are four major blood groups determined by the presence or absence of two antigens – A and B – on the surface of red blood cells: Group A – has only the A antigen on red cells (and B antibody in the plasma) Group B – has only the B antigen on red cells (and A antibody in the plasma) Group AB – has both A and B antigens on red cells (but neither A nor B antibody in the plasma) Group O – has neither A nor B antigens on red cells (but both A and B antibody are in the plasma)

Recommended range without diabetes is 70 to 130mg/dL. (The standard for measuring blood glucose is "mg/dL" which means milligrams per deciliter.) If your blood glucose level is above 130mg/dL, that's fasting hyperglycemia. Fasting hyperglycemia is a common diabetes complication.

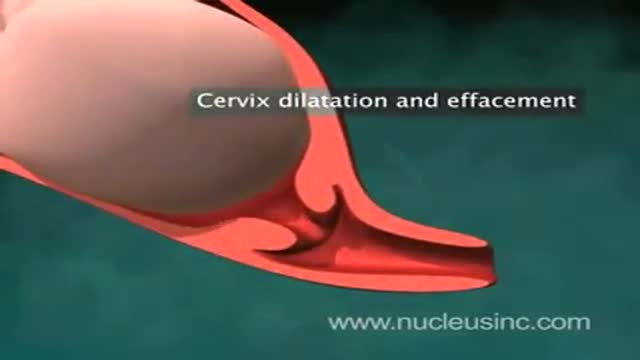
MotionLit can help you multiply the value of your case by portraying the mechanisms of injuries in a 3D Accident Reconstruction Animation. Call (855)850-0650 or visit motionlit.com to learn & earn more for your client!
MotionLit is a one-stop-shop for litigators, offering complete trial services from video production, animation, litigation support, exhibit design, trial technician, and video depositions. Our visuals have proven to help attorneys obtain record-breaking verdicts with our persuasive trial presentations, settlement documentaries, and demonstratives.
Contact Us At:
www.motionlit.com
(213) 291 9141
info@motionlit.com
Follow Us On:
Twitter: @motionlit
Instagram: https://www.instagram.com/motionlit/
Facebook: https://www.facebook.com/MotionLit/