Top videos
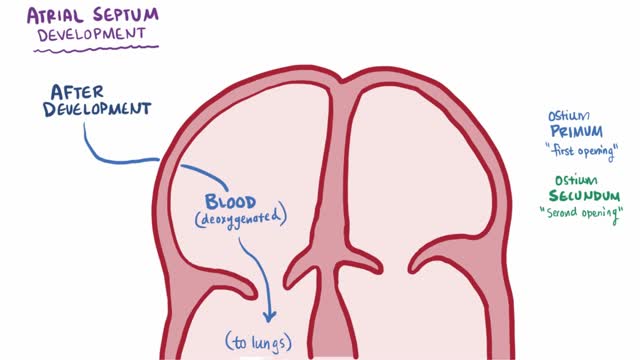
An atrial septal defect (ASD) is a hole in the wall between the two upper chambers of your heart (atria). The condition is present from birth (congenital). Small atrial septal defects may close on their own during infancy or early childhood. Large and long-standing atrial septal defects can damage your heart and lungs. Small defects may never cause a problem and may be found incidentally. An adult who has had an undetected atrial septal defect for decades may have a shortened life span from heart failure or high blood pressure that affects the arteries in the lungs (pulmonary hypertension). Surgery may be necessary to repair atrial septal defects to prevent complications.

Bone tumors include abnormal healing of an injury, inherited conditions, radiation therapy. It can also be caused by bone cancer or another cancer that has spread to the bone from other parts of the body. A bone tumor may cause a painless mass. Some people have dull, aching pain. And in some cases, minor injury causes a fracture near the tumor. Treatments include surgery and radiation. Some noncancerous tumors go away without treatment
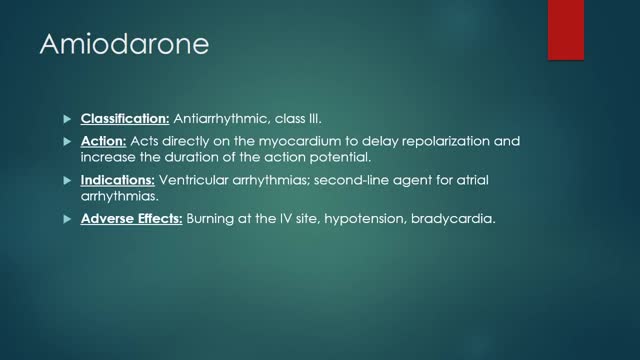
Why is this medication prescribed? Amiodarone is used to treat and prevent certain types of serious, life-threatening ventricular arrhythmias (a certain type of abnormal heart rhythm when other medications did not help or could not be tolerated. Amiodarone is in a class of medications called antiarrhythmics. It works by relaxing overactive heart muscles. How should this medicine be used? Amiodarone comes as a tablet to take by mouth. It is usually taken once or twice a day. You may take amiodarone either with or without food, but be sure to take it the same way each time.Follow the directions on your prescription label carefully, and ask your doctor or pharmacist to explain any part you do not understand. Take amiodarone exactly as directed. Do not take more or less of it or take it more often than prescribed by your doctor.

The term dermoid cyst does not appear to be restricted to a single kind of lesion nor is it used in only a single medical discipline. The term dermoid cyst can be found in the vocabulary of dermatologists, dermatopathologists, general pathologists, gynecologists, neurosurgeons, or pediatricians. If asked, all of these clinicians would most probably define and describe dermoid cysts differently. For example, gynecologists and general pathologists might say that a dermoid cyst is a cystic tumor of the ovary. In contrast, neurosurgeons tend to view a dermoid cyst is associated with a congenital cyst of the spine or an intracranial congenital cyst. For pediatricians and dermatologists, dermoid cyst means subcutaneous cysts, which are usually congenital.[1]
Wolff-Parkinson-White (WPW) syndrome, an extra electrical pathway between your heart's upper and lower chambers causes a rapid heartbeat. The extra pathway is present at birth and fairly rare. The episodes of fast heartbeats usually aren't life-threatening, but serious heart problems can occur. Treatment can stop or prevent episodes of fast heartbeats. A catheter-based procedure (ablation) can permanently correct the heart rhythm problems. Most people with an extra electrical pathway experience no fast heartbeat. This condition, called Wolff-Parkinson-White pattern, is discovered only by chance during a heart exam. Although WPW pattern is often harmless, doctors might recommend further evaluation before children with WPW pattern participate in high-intensity sports.

EART (Health Education and Rescue Training) Wilderness First Aid is an intensive course that covers patient examination and evaluation, body systems and anatomy, wound care, splinting, environmental emergencies, and backcountry medicine. Hands-on simulations provide first-hand training in treating patients. This is an excellent course taught by experienced Wilderness First Responders and Emergency Medical Technicians and is highly recommended to all wilderness travelers. People who pass the courses will receive a Wilderness First Aid certification from the Emergency Care and Safety Institute (ECSI) which is good for 2 years. Participants who successfully pass CPR and HEART Wilderness First Aid will have met the First Aid requirements for OA Leader Training.
Shingles is a viral infection that causes a painful rash. Although shingles can occur anywhere on your body, it most often appears as a single stripe of blisters that wraps around either the left or the right side of your torso. Shingles is caused by the varicella-zoster virus — the same virus that causes chickenpox. After you've had chickenpox, the virus lies inactive in nerve tissue near your spinal cord and brain. Years later, the virus may reactivate as shingles. While it isn't a life-threatening condition, shingles can be very painful. Vaccines can help reduce the risk of shingles, while early treatment can help shorten a shingles infection and lessen the chance of complications.

Hirsutism is stiff and pigmented body hair, appearing on the body where women don't commonly have hair — primarily the face, chest and back. When excessively high androgen levels cause hirsutism, other signs may develop over time, a process called virilization. Signs of virilization may include: Deepening voice Balding Acne Decrease in breast size Enlargement of the clitoris

Mouth ulcers are sores that appear in the mouth, often on the inside of the cheeks. Mouth ulcers, also known as aphthous ulcers, can be painful when eating, drinking or brushing teeth. Occasional mouth ulcers are usually harmless and clear up on their own. Seek medical advice if they last longer than 3 weeks or keep coming back. Mouth ulcers cannot be caught from someone else. Up to 1 in 5 people get recurrent mouth ulcers.
Thalassemia is an inherited blood disorder characterized by less hemoglobin and fewer red blood cells in your body than normal. Several types of thalassemia exist, including alpha-thalassemia, beta-thalassemia intermedia, Cooley's anemia and Mediterranean anemia. Hemoglobin is the substance in your red blood cells that allows them to carry oxygen. The low hemoglobin and fewer red blood cells of thalassemia may cause anemia, leaving you fatigued. If you have mild thalassemia, you may not need treatment. But, if you have a more severe form of thalassemia, you may need regular blood transfusions. You can also take steps on your own to cope with fatigue, such as choosing a healthy diet and exercising regularly.