Top videos
This new surgical technique provide good stability for all type of fracture even severe comminution. Each fragment are reduced and several pin sleeves are inserted circumferentially and tighten by braded cable through the sleeve box. The final features of surgery seems blooming sunflower 'Himwari in Jananese'.
Renal artery stenosis is the narrowing of one or more arteries that carry blood to your kidneys (renal arteries). Narrowing of the arteries prevents normal amounts of oxygen-rich blood from reaching your kidneys. Your kidneys need adequate blood flow to help filter waste products and remove excess fluids. Reduced blood flow may increase blood pressure in your whole body (systemic blood pressure) and injure kidney tissue.
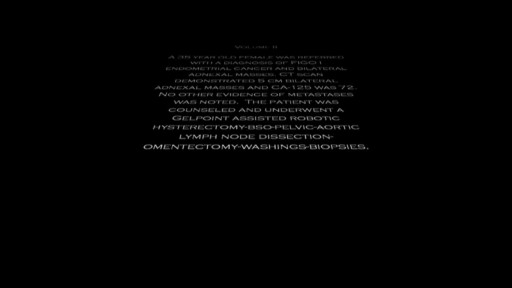
A young patient undergoes state of the art robotic surgery for Ovarian Cancer and Endometrial Cancer in Chicago, IL. The surgery is performed by noted gynecologic oncologist and expert robotic surgeon M. Patrick Lowe MD. Dr Lowe has been performing robotic surgery since 2006 and is one of a few gynecologic oncologist in the United States who utilizes robotics for ovarian cancer.
Multiple sclerosis (MS) affects the brain and spinal cord. Early MS symptoms include weakness, tingling, numbness, and blurred vision. Other signs are muscle stiffness, thinking problems, and urinary problems. Treatment can relieve MS symptoms and delay disease progression.

Focal seizures (also called partial seizures [citation needed] and localized seizures) are seizures which affect initially only one hemisphere of the brain. [citation needed] The brain is divided into two hemispheres, each consisting of four lobes – the frontal, temporal, parietal and occipital lobes.

If you’re wondering ‘what’s the cause of my knee pain?’ or ‘what kind of knee pain do I have?’ the position of your knee pain can often tell you what type of knee pain you have.
You confirm this if you know the common symptoms an aggravations for each type of knee problem. So if you want to know ‘why my knee hurts’... here’s a quick look at the most common type of knee problems...
Patellofemoral Pain Syndrome (Or Runner’s Knee) (Old Name: Chondromalacia Patellae)
Infrapatellar Fat Pad Syndrome (Hoffa's Syndrome)
Patella Tendonitis (Jumper’s Knee)
Prepatellar Bursitis
Osgood-Schlatter Disease
Meniscus Tear
Medial Collateral Ligament Tear
Osteoarthritic Knee Pain
Pes Anserine Bursitis.
Iliotibial Band Syndrome
Quadriceps Tendinopathy
Popliteus Strain
Baker’s Cyst
ACL Or PCL Tear/Rupture
---------------------------------------
Check out my channel...
https://youtube.com/@BodyFixExercises
OTHER VIDEOS:
How To Fix Pain In The Front Of The Knee… (Runner's Knee) https://youtu.be/g0qmx_0enAA
Knee Strengthening Exercises To Prevent Knee Pain
https://youtu.be/Pk-ae_lyx7M
How To Treat Patellar Tendinopathy (Jumper’s Knee) & Quadriceps Tendinopathy
https://youtu.be/MkPwsb-rQwU
---------------------------------------
#bodyfixexercises #kneepainrelief #kneepain

www.diabetes.org > Living With Diabetes > Treatment and Care > Medication > Insulin & Other Injectables Share: Print PageText Size:A A A Listen How Do Insulin Pumps Work? If you have been diagnosed with diabetes, you may feel overwhelmed by all the new information you have learned and will continue to learn about managing your diabetes. You already know your main goal should be to get your blood glucose (sugar) levels under control in order to increase your chances of a complication-free life. Many people know this, but need to know how to achieve good diabetes management, while balancing the day-to-day demands of diabetes with other life demands. An insulin pump can help you manage your diabetes. By using an insulin pump, you can match your insulin to your lifestyle, rather than getting an insulin injection and matching your life to how the insulin is working. When you work closely with your diabetes care team, insulin pumps can help you keep your blood glucose levels within your target ranges. People of all ages with type 1 diabetes use insulin pumps and people with type 2 diabetes have started to use them as well. - See more at: http://www.diabetes.org/living-with-diabetes/treatment-and-care/medication/insulin/how-do-insulin-pumps-work.html?referrer=https://www.google.com/#sthash.XD56v351.dpuf
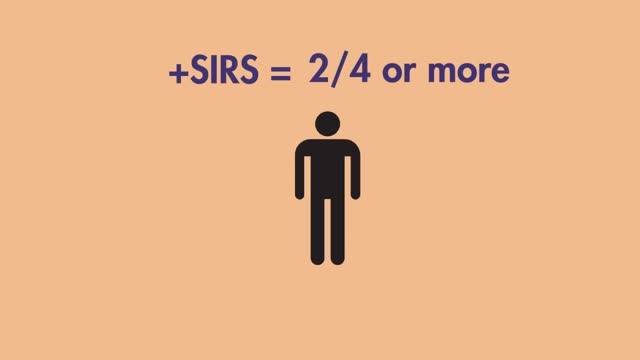
Learn the SIRS Criteria and how to calculate it. Greater than or equal to 2 or more of the following: Temperature Fever of greater than 38°C (100.4°F) or Less than 36°C (96.8°F) Heart Rate Greater than 90 beats per minute Respiratory Rate Greater than 20 breaths per minute or PaCO2 of less than 32mm Hg White Blood Cell Count Greater than 12,000cells/mm³ or Less than 4,000cells/mm³ or Greater than 10% Bands

Function and Anatomy:
Hinge type joint formed by the articulation of the Ulna and Radius (bones of the forearm), and Humerus (upper arm). Full extension is equal to 0 degrees, full flexion to ~ 150 degrees. Maximum supination (turning hand palm up so that it can hold a bowl of "soup") and pronation (palm down) are both 90 degrees

The E.coli bacteria has claimed 14 lives and infected more than 300 hundred in the country. It has now spread to other European states.
Facing an increasing number of cases, German health authorities warned people to avoid eating raw cucumber, tomatoes and lettuce.
Reinhard Burger, President of Robert Koch Institute, said, "As for the present situation there is no reason to give the all-clear yet and it is possible the original source of the infection is still active and could lead to further infections."
The first cases of the EHEC outbreak were noticed in Northern Germany, but infections are now spreading across the country.
Cases haves spiked compared to other years, and are still rising.
Daniel Bahr, German Health Minister, said, "The result is that we unfortunately still have to prepare for a rising number of cases. Exercising caution is still recommended and we ask our citizens to be particularly careful. "
But, the German government says it's working around the clock to stop the outbreak and clarify how it arose.
Ilse Aigner, German Agriculture Minister, said, "Together, we face a big challenge to piece together hundreds or thousands of mosaic pieces from Germany and abroad into an overall picture that gives us a clear answer on how this terrible infection arose. "
In the meantime, experts are advising not to eat pre-packaged or prepared salad, which may contain the bacteria.
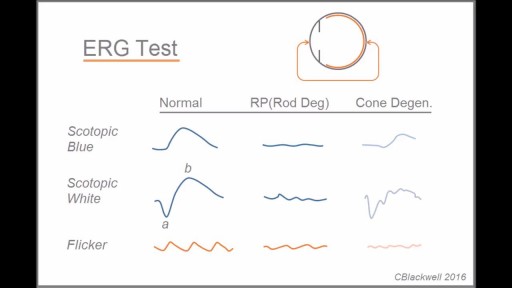
Retinitis pigmentosa is a rare, inherited degenerative eye disease that causes severe vision impairment. Symptoms often begin in childhood. They include decreased vision at night or in low light and loss of side vision (tunnel vision). There's no effective treatment for this condition. Wearing sunglasses may help protect remaining vision.

Initial treatment of a deviated septum may be directed at managing the symptoms of the tissues lining the nose, which may then contribute to symptoms of nasal obstruction and drainage. Your doctor may prescribe: Decongestants. Decongestants are medications that reduce nasal tissue swelling, helping to keep the airways on both sides of your nose open. Decongestants are available as a pill or as a nasal spray. Use nasal sprays with caution, however. Frequent and continued use can create dependency and cause symptoms to be worse (rebound) after you stop using them. Decongestants have a stimulant effect and may cause you to be jittery as well as elevate your blood pressure and heart rate. Antihistamines. Antihistamines are medications that help prevent allergy symptoms, including obstruction and runny nose. They can also sometimes help nonallergic conditions such as those occurring with a cold. Some antihistamines cause drowsiness and can affect your ability to perform tasks that require physical coordination, such as driving. Nasal steroid sprays. Prescription nasal corticosteroid sprays can reduce inflammation in your nasal passage and help with obstruction or drainage. It usually takes from one to three weeks for steroid sprays to reach their maximal effect, so it is important to follow your doctor's directions in using them. Medications only treat the swollen mucus membranes and won't correct a deviated septum.