Top videos
http://smoking-videos.plus101.com
Quit Smoking Forever Formula Videos - How To Quit Smoking In As Fast As 1 Week Without Agitation, Cravings Or Withdrawal Symptoms.You're about to uncover the 3 elements that will rapidly boost your chances of success to quit smoking and not only that, you'll learn ways to escape cravings and how to avoid a relapse that can happen in the future even to people with the most willpower.

Rhinoplasty enhances facial harmony and the proportions of your nose. It can also correct impaired breathing caused by structural defects in the nose. Rhinoplasty surgery can change: Nose size in relation to facial balance Nose width at the bridge or in the size and position of the nostrils Nose profile with visible humps or depressions on the bridge Nasal tip that is enlarged or bulbous, drooping, upturned or hooked Nostrils that are large, wide, or upturned Nasal asymmetry If you desire a more symmetrical nose, keep in mind that everyone’s face is asymmetric to some degree. Results may not be completely symmetric, although the goal is to create facial balance and correct proportion.
Renal replacement therapies are a set of interventions and techniques aimed at replacement of the filtering function of the kidneys. These include both dialysis and renal transplant. In this presentation we will talk about the indication and modalities of dialysis. This includes hemodialysis, peritoneal dialysis and continuous renal replacement therapies. The circuit diagram of each modalities along with its procedure and complications are also discussed.

Brachytherapy or localized radiation treatment can be used in certain patients with breast cancer. Depending on tumor size and other factor, physicians may use APBI or accelerated partial breast irradiation. Dr. Elizabeth Tapen, a radiation oncologist, reviews brachytherapy for breast cancer.

Epilepsy surgery is reserved for people whose seizures are not well controlled by seizure medicines. This situation is sometimes called being "medically refractory" or "drug resistant." In children, the definition of medically refractory is even more individualized to the specific child's situation. Surgery may be considered for some children after weeks to months of treatment with seizure medicines.
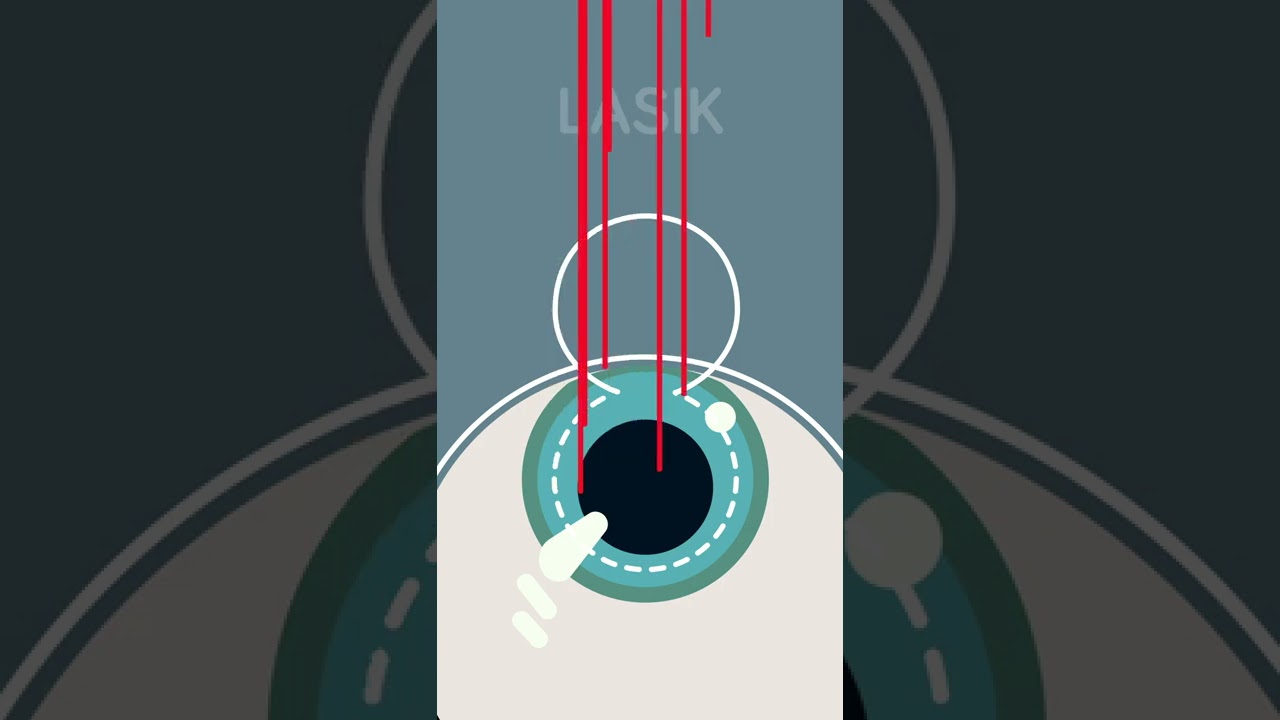
Ever considered getting laser eye surgery, but didn’t know how it worked? Allow us to help!
There are three different main types of laser eye surgery: LASIK, SMILE, and Surface Laser Treatments, and each can be explained pretty easily.
LASIK uses two lasers to open up a thin flap on the surface of the cornea, and then reshapes the cornea underneath. The flap is then placed back over the reshaped cornea, and heals independently with time.
SMILE uses one laser to reshape the cornea through a small, self-healing hole.
And Surface Eye Treatments remove the clear skin over the eye, to then reshape the cornea underneath with - you guessed it - a laser!

We get excited when people graduate! May it be graduating from physiotherapy or even graduating onto a new progression of an exercise! Today you move onto new challenges as Mike & Tyler demonstrate the final side plank progression. Kitchener Massage Therapy - http://www.strivept.ca/massage-therapy-kitchener.html

It sounds like you're questioning whether or not your water may have broken, and this can actually be a hard thing for a lot of women to tell. Usually if your water breaks, it's just a trickle of fluid, and you're afraid to admit it to anyone because you think you peed your pants. And it is normal to pee your pants when you're pregnant because the bladder is right below the uterus, and if the baby moves just right, it might kick out a little bit of urine. So if you feel a trickle or a little tiny gush of fluid, what you want to do is put a pad or a pantie-liner on after going to the bathroom and emptying your bladder, and wait an hour and see if fluid continues to come out. And if it does, then you're not having bladder leakage issues - your water is probably broken.

New research from Mount Sinai Health System says these surgeries have limited effectiveness and can be economically unjustifiable when they're done on patients with less severe symptoms.
» Subscribe to NBC News: http://nbcnews.to/SubscribeToNBC
» Watch more NBC video: http://bit.ly/MoreNBCNews
NBC News is a leading source of global news and information. Here you will find clips from NBC Nightly News, Meet The Press, and original digital videos. Subscribe to our channel for news stories, technology, politics, health, entertainment, science, business, and exclusive NBC investigations.
Connect with NBC News Online!
Visit NBCNews.Com: http://nbcnews.to/ReadNBC
Find NBC News on Facebook: http://nbcnews.to/LikeNBC
Follow NBC News on Twitter: http://nbcnews.to/FollowNBC
Follow NBC News on Google+: http://nbcnews.to/PlusNBC
Follow NBC News on Instagram: http://nbcnews.to/InstaNBC
Follow NBC News on Pinterest: http://nbcnews.to/PinNBC
New Study Questions Effectiveness Of Knee Replacement Surgery | NBC Nightly News

Learn Basic Laparoscopic Surgery, the components of a laparoscopic surgical setup, optimal positioning and ergonomics in laparoscopic surgery, and much more. Check out the full course for free here: https://www.incision.care/free-trial
What is Laparoscopic Surgery:
Laparoscopic surgery describes procedures performed using one or multiple small incisions in the abdominal wall in contrast to the larger, normally singular incision of laparotomy. The technique is based around principles of minimally invasive surgery (or minimal access surgery): a large group of modern surgical procedures carried out by entering the body with the smallest possible damage to tissues. In abdominopelvic surgery, minimally invasive surgery is generally treated as synonymous with laparoscopic surgery as are procedures not technically within the peritoneal cavity, such as totally extraperitoneal hernia repair, or extending beyond the abdomen, such as thoraco-laparoscopic esophagectomy. The term laparoscopy is sometimes used interchangeably, although this is often reserved to describe a visual examination of the peritoneal cavity or the purely scopic component of a laparoscopic procedure. The colloquial keyhole surgery is common in non-medical usage.
Surgical Objective of Laparoscopic Surgery:
The objective of a laparoscopic approach is to minimize surgical trauma when operating on abdominal or pelvic structures. When correctly indicated and performed, this can result in smaller scars, reduced postoperative morbidity, shorter inpatient durations, and a faster return to normal activity. For a number of abdominopelvic procedures, a laparoscopic approach is now generally considered to be the gold-standard treatment option.
Definitions
Developments of Laparoscopic Surgery:
Following a number of smaller-scale applications of minimally invasive techniques to abdominopelvic surgery, laparoscopic surgery became a major part of general surgical practice with the introduction of laparoscopic cholecystectomy in the 1980s and the subsequent pioneering of endoscopic camera technology. This led to the widespread adoption of the technique by the early- to mid-1990s. The portfolio of procedures that can be performed laparoscopically has rapidly expanded with improvements in instruments, imaging, techniques and training — forming a central component of modern surgical practice and cross-specialty curricula [2]. Techniques such as laparoscopically assisted surgery and hand-assisted laparoscopic surgery have allowed the application of laparoscopic techniques to a greater variety of pathology. Single-incision laparoscopic surgery, natural orifice transluminal endoscopic surgery, and minilaparoscopy-assisted natural orifice surgery continue to push forward the applications of minimally invasive abdominopelvic techniques; however, the widespread practice and specific indications for these remain to be fully established. More recently, robotic surgery has been able to build on laparoscopic principles through developments in visualization, ergonomics, and instrumentation.
This Basic Laparoscopic Surgery Course Will Teach You:
- Abdominal access techniques and the different ways of establishing a pneumoperitoneum
- Principles of port placement and organization of the operative field
- Key elements of laparoscopic suturing, basic knotting and clip application
Specific attention is paid to the following hazards you may encounter:
- Fire hazard and thermal injury
- Lens fogging
- Contamination of insufflation system
- Complications from trocar introduction
- Limitations of Veress needle technique
- Limitations of open introduction technique
- Complications of the pneumoperitoneum
- Gas embolism
- Mirroring and scaling of instrument movements
- Firing clip applier without a loaded clip
The following tips are designed to improve your understanding and performance:
- Anatomy of a laparoscope
- Checking for optic fiber damage
- "White balance" of camera
- Checking integrity of electrosurgical insulation
- Access at Palmer's point
- Lifting abdominal wall before introduction
- Confirming position of Veress needle
- Umbilical anatomy
- Identification of inferior epigastric vessels under direct vision
- Translumination of superficial epigastric vessels
- Selection of trocar size
- Aiming of trocar
- Working angles in laparoscopic surgery
- Choice of suture material
- Instruments for suturing
- Optimal ergonomics for suturing
- Extracorporeal needle positioning
- Optimal suture lengths
- "Backloading" needle
- Intracorporeal needle positioning
- Hand movements when suturing
- Optimal positioning of scissors
- Extracorporeal knot tying
- Visualization of clip applier around target structure
- Common clip configurations

As a pediatric surgeon at NewYork-Presbyterian/Weill Cornell Medical Center, Dr. Nitsana Spigland treats newborns, children, teens, and young adults requiring surgical interventions. She specializes in antenatal counseling and newborn congenital malformations.
Learn more about Dr. Spigland at: https://www.nyp.org/physician/nspigland.