Top videos
Pink eye (conjunctivitis) is an inflammation or infection of the transparent membrane (conjunctiva) that lines your eyelid and covers the white part of your eyeball. When small blood vessels in the conjunctiva become inflamed, they're more visible. This is what causes the whites of your eyes to appear reddish or pink. Pink eye is commonly caused by a bacterial or viral infection or an allergic reaction. It may affect one or both eyes. Pink eye can be irritating, but it rarely affects your vision. Treatments can help ease the discomfort of pink eye. Because pink eye can be contagious, early diagnosis and treatment can help limit its spread.
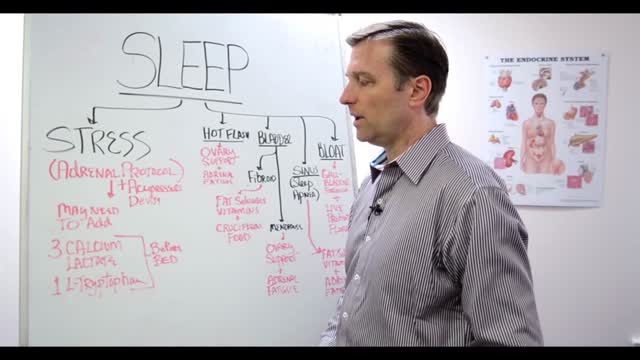
A sleep disorder, or somnipathy, is a medical disorder of the sleep patterns of a person or animal. Some sleep disorders are serious enough to interfere with normal physical, mental, social and emotional functioning. Polysomnography and actigraphy are tests commonly ordered for some sleep disorders.

Hypertensive emergencies encompass a spectrum of clinical presentations in which uncontrolled blood pressures lead to progressive or impending end-organ dysfunction. In these conditions, the BP should be lowered aggressively over minutes to hours. Neurologic end-organ damage due to uncontrolled BP may include hypertensive encephalopathy, cerebral vascular accident/cerebral infarction, subarachnoid hemorrhage, and/or intracranial hemorrhage.[1] Cardiovascular end-organ damage may include myocardial ischemia/infarction, acute left ventricular dysfunction, acute pulmonary edema, and/or aortic dissection. Other organ systems may also be affected by uncontrolled hypertension, which may lead to acute renal failure/insufficiency, retinopathy, eclampsia, or microangiopathic hemolytic anemia.[1] With the advent of antihypertensives, the incidence of hypertensive emergencies has declined from 7% to approximately 1% of patients with hypertension.[2] In addition, the 1-year survival rate associated with this condition has increased from only 20% (prior to 1950) to a survival rate of more than 90% with appropriate medical treatment
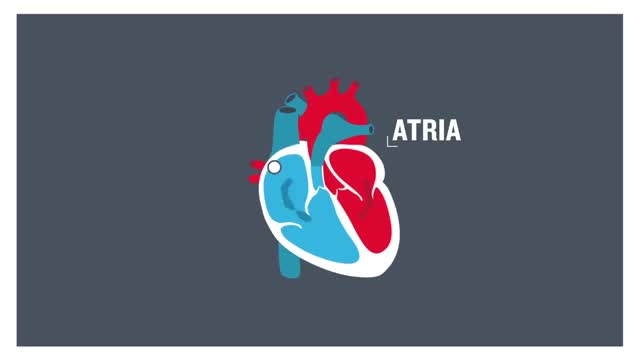
Atrial flutter (AFL) is a type of abnormal heart rate, or arrhythmia. It occurs when the upper chambers of your heart beat too fast. When the chambers in the top of your heart (atria) beat faster than the bottom ones (ventricles), it complicates your heart rhythm

In as many as 80% of cases, doctors don’t find the exact reason for a curved spine. Scoliosis without a known cause is what doctors call “idiopathic.” Some kinds of scoliosis do have clear causes. Doctors divide those curves into two types -- structural and nonstructural. In nonstructural scoliosis, the spine works normally, but looks curved. Why does this happen? There are a number of reasons, such as one leg’s being longer than the other, muscle spasms, and inflammations like appendicitis. When these problems are treated, this type of scoliosis often goes away.

Come Rimanere Incinta Subito, Probabilità Di Rimanere Incinta A 40 Anni, Primi Sintomi Gravidanza---- http://come-rimanere-incinta.info-pro.co --- Esperta in Medicina Cinese, Specializzata in Trattamenti per la Salute e in Nutrizione, Consulente per la Salute, Dopo Aver Provato in Prima Persona l'Infertilità e Averla Sconfitta ti Insegna Come: Rimanere Incinta in Modo Rapido e del Tutto Naturale in Soli 2 Mesi Dare alla Luce Bambini Sani e Forti Invertire il Problema dell'Infertilità, sia Maschile che Femminile Migliorare la Qualità della Tua Vita...Drasticamente! Scopri Come Ha Vinto la Sua Infertilità e Ha Insegnato a Migliaia di Donne in Tutto il Mondo Come Eliminare Tutti i Problemi dell'Infertilità e Come Rimanere Incinta in Modo Rapido e, Soprattutto, del Tutto Naturale Blog: http://bit.ly/2F3k8xR Se Stai Lottando con Tutte le Tue Forze per Rimanere Incinta e Nonostante Tutto Ancora Non Hai Ottenuto Risultati, Questa Sarà la Lettera Più Importante che Potrai Mai Leggere... Clicca sul link http://come-rimanere-incinta.info-pro.co
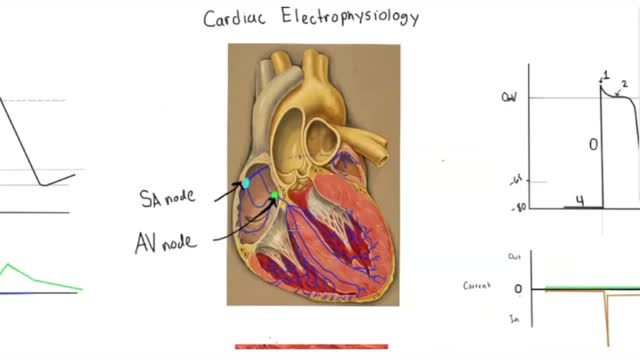
Electrophysiology studies test the electrical activity of your heart to find where an arrhythmia (abnormal heartbeat) is coming from. These results can help you and your doctor decide whether you need medicine, a pacemaker, an implantable cardioverter defibrillator (ICD), cardiac ablation or surgery.
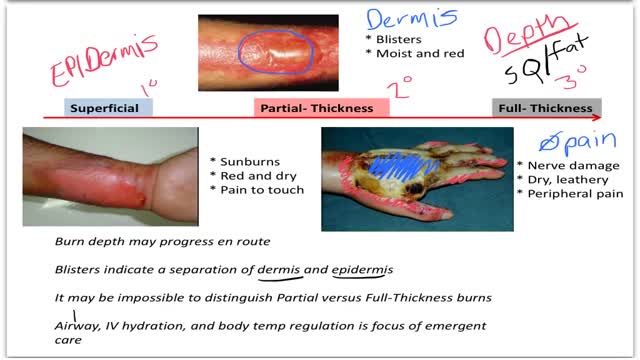
Burns are classified as first-, second-, or third-degree, depending on how deep and severe they penetrate the skin's surface. First-degree burns affect only the epidermis, or outer layer of skin. The burn site is red, painful, dry, and with no blisters. Mild sunburn is an example.

Today, we're going to expand on our past postural work and exercises. We have taken a look at a few variations of this exercise. The next progression is to move into standing against the wall. This exercise hits many different spots including your pecs and mid-back. The key is to breathe and work on it slowly. Stick with it and you'll make some change! Check us out on Social Media! Facebook: https://www.facebook.com/striveptandperformance/ Instagram: https://www.instagram.com/striveptandperf/ Twitter: https://twitter.com/StrivePTandPerf Blog: http://www.strivept.ca/blog