Top videos

Peptic ulcers are open sores that develop on the inside lining of your stomach and the upper portion of your small intestine. The most common symptom of a peptic ulcer is stomach pain. Peptic ulcers include: Gastric ulcers that occur on the inside of the stomach Duodenal ulcers that occur on the inside of the upper portion of your small intestine (duodenum) The most common causes of peptic ulcers are infection with the bacterium Helicobacter pylori (H. pylori) and long-term use of aspirin and certain other painkillers, such as ibuprofen (Advil, Motrin, others) and naproxen sodium (Aleve, Anaprox, others). Stress and spicy foods do not cause peptic ulcers. However, they can make your symptoms worse.
Electronystagmography (ENG) is a diagnostic test to record involuntary movements of the eye caused by a condition known as nystagmus. It can also be used to diagnose the cause of vertigo, dizziness or balance dysfunction by testing the vestibular system.
Absence seizures involve brief, sudden lapses of consciousness. They're more common in children than adults. Someone having an absence seizure may look like he or she is staring into space for a few seconds. This type of seizure usually doesn't lead to physical injury. Absence seizures usually can be controlled with anti-seizure medications. Some children who have them also develop other seizures. Many children outgrow absence seizures in their teens.
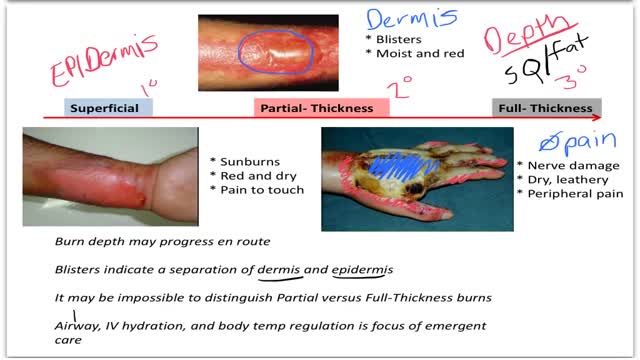
Burns are classified as first-, second-, or third-degree, depending on how deep and severe they penetrate the skin's surface. First-degree burns affect only the epidermis, or outer layer of skin. The burn site is red, painful, dry, and with no blisters. Mild sunburn is an example.

Plantar warts are hard, grainy growths that usually appear on the heels or balls of your feet, areas that feel the most pressure. This pressure also may cause plantar warts to grow inward beneath a hard, thick layer of skin (callus). Plantar warts are caused by the human papillomavirus (HPV). The virus enters your body through tiny cuts, breaks or other weak spots on the bottom of your feet. Most plantar warts aren't a serious health concern and may not require treatment. But plantar warts can cause discomfort or pain. If self-care treatments for plantar warts don't work, you may want to see your doctor to have them removed.

Skin cancer is the most common type of cancer. There are three major types of skin cancer — Basal Cell Carcinoma, Squamous Cell Carcinoma and melanoma. Out of these, Melanoma is the deadliest form of skin cancer. Melanoma appears on the skin as a new spot or growth or a change in an already existing mole. It is often fast growing and can spread to other parts of your body, including your bones, liver, and lungs to form a new cancer.

Carpal tunnel release (part 1). Skin incision and retraction. Procedure performed by Deepak Kapila, MD, Broward Health, Fort Lauderdale, FL. Courtesy of BroadcastMed (http://ortho.broadcastmed.com/....4229/videos/carpal-t
There are hundreds more procedural videos as well as news, features, resources and references on Medscape.com. Join today for free.
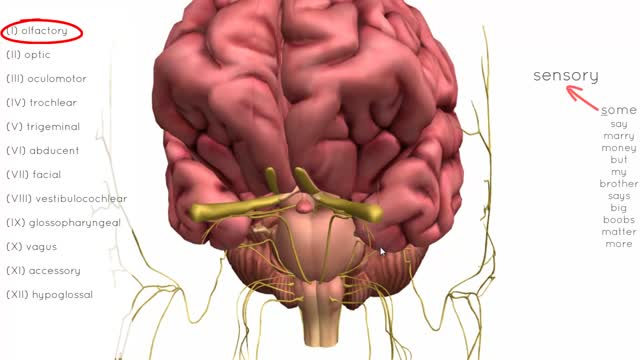
There are twelve cranial nerves in total. The olfactory nerve (CN I) and optic nerve (CN II) originate from the cerebrum. Cranial nerves III – XII arise from the brain stem (Figure 1). They can arise from a specific part of the brain stem (midbrain, pons or medulla), or from a junction between two parts: Midbrain – the trochlear nerve (IV) comes from the posterior side of the midbrain. It has the longest intracranial length of all the cranial nerves. Midbrain-pontine junction – oculomotor (III). Pons – trigeminal (V). Pontine-medulla junction – abducens, facial, vestibulocochlear (VI-VIII). Medulla Oblongata – posterior to the olive: glossopharyngeal, vagus, accessory (IX-XI). Anterior to the olive: hypoglossal (XII). The cranial nerves are numbered by their loca
This new surgical technique provide good stability for all type of fracture even severe comminution. Each fragment are reduced and several pin sleeves are inserted circumferentially and tighten by braded cable through the sleeve box. The final features of surgery seems blooming sunflower 'Himwari in Jananese'.
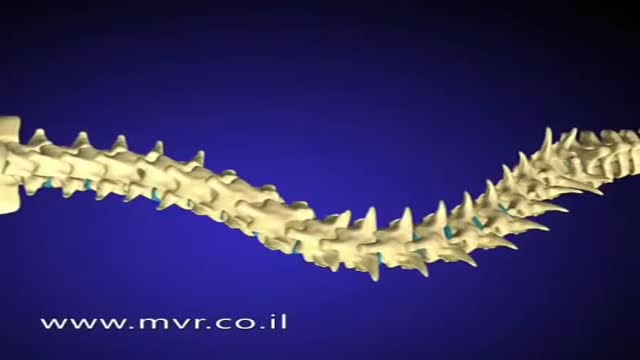
There are several approaches to scoliosis surgery, but all use modern instrumentation systems in which hooks and screws are applied to the spine to anchor long rods. The rods are then used to reduce and hold the spine while bone that is added fuses together with existing bone.

Our mission: Empower you with the tools and support you need for weight loss and live a healthier life. Get started on your weight loss journey today: https://bit.ly/2Ms4JaX