Top videos

This video is brought to you by the Stanford Medicine 25 to teach you the common causes of shoulder pain and how to diagnose them by the physical exam.
The Stanford Medicine 25 program for bedside medicine at the Stanford School of Medicine aims to promote the culture of bedside medicine to make current and future clinicians and other healthcare provides better at the art of physical diagnosis and more confident at the bedside of their patients.
Visit us:
Website: http://stanfordmedicine25.stanford.edu/
Blog: http://stanfordmedicine25.stanford.edu/blog.html
Facebook: https://www.facebook.com/StanfordMedicine25
Twitter: https://twitter.com/StanfordMed25
Diagnoses covered in this video:
Rotator Cuff Pathology
Impingement Syndrome
Biceps Tendinopathy
Adhesive Capsulitis (Frozen Shoulder)
Acromioclavicular (AC) Joint Disease
Shoulder Instability
Labral Tears (SLAP Lesions)
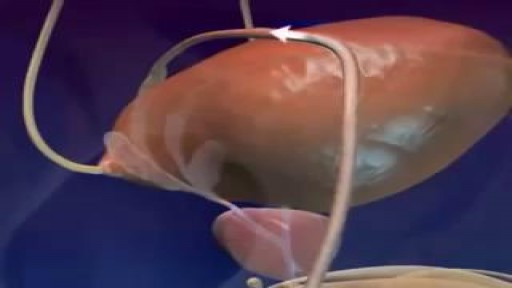
The male orgasm is a common subject but usually misunderstood at the same time. Men are sometimes led to believe that ejaculating often is a bad thing, particularly if you masturbate. The truth is that ejaculation is important to every man due to a number of reasons. The main goal of this post is to shed some light on reasons why men need to ejaculate.
Dilation and curettage (D&C) is a procedure to remove tissue from inside your uterus. Doctors perform dilation and curettage to diagnose and treat certain uterine conditions — such as heavy bleeding — or to clear the uterine lining after a miscarriage or abortion. In a dilation and curettage — sometimes spelled "dilatation" and curettage — your doctor uses small instruments or a medication to open (dilate) your cervix — the lower, narrow part of your uterus. Your doctor then uses a surgical instrument called a curette to remove uterine tissue. Curettes used in a D&C can be sharp or use suction

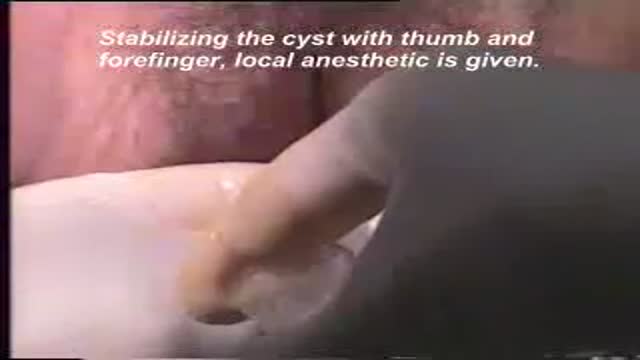
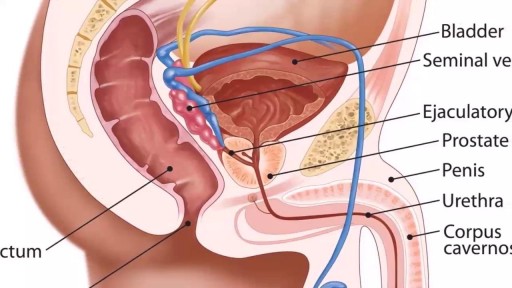
A testicular examination is mainly performed on male patients who present with testicular pathology e.g. pain, swelling, a lump. Although titled testicular examination it involves the examination of the penis, scrotum and testes. As this is an intimate examination it is pertinent to gain a good rapport with your patient, maintain good communication and ensure the patient’s dignity at all times. Remember to offer a chaperone for this skill. For the purposes of your exam, you will most likely be examining a mannequin.

This animation shows you how a tummy tuck is performed at Boerhaave Medical Centre. Curious? Watch the video!
Boerhaave Medical Centre sets itself the goal of providing the highest quality care. Quality not just in terms of treatment, but also in terms of our staff and the before and after care given. By providing thorough information and clear advice in advance, carefully supporting our patients through the procedure and caring for them afterwards, we believe this quality is assured.
Although we are one of the largest clinics in the Netherlands and have built up many years of experience, we continuously strive to improve. After all, the Boerhaave Medical Centre intends to remain a pioneer in the healthcare sector, by working in accordance with the latest medical findings and techniques both now and in the future.
We offer the highest standard of plastic surgery in our cosmetic care department. For 365 days a year, you can also come to us for non-surgical treatments, such as injectables, permanent hair removal and gastric balloons.
We have been awarded the ZKN quality mark and are certified to ISO 9001-2008 for giving advice and carrying out plastic surgery, including after care.
Visit our website for more information: https://www.boerhaave.com/all-....treatments/upperbody
Follow us:
Facebook: https://www.facebook.com/boerhaavemc
Google+: https://plus.google.com/+BoerhaaveNl-Kliniek
Pinterest: https://nl.pinterest.com/BoerhaaveMC/
Instagram: https://www.instagram.com/BoerhaaveMC/
Tonsillectomy (ton-sih-LEK-tuh-me) is the surgical removal of the tonsils, two oval-shaped pads of tissue at the back of the throat — one tonsil on each side. A tonsillectomy was once a common procedure to treat infection and inflammation of the tonsils (tonsillitis). Today, a tonsillectomy is usually performed for sleep-disordered breathing but may still be a treatment when tonsillitis occurs frequently or doesn't respond to other treatments. A tonsillectomy may also be necessary to treat breathing and other problems related to enlarged tonsils and to treat rare diseases of the tonsils.
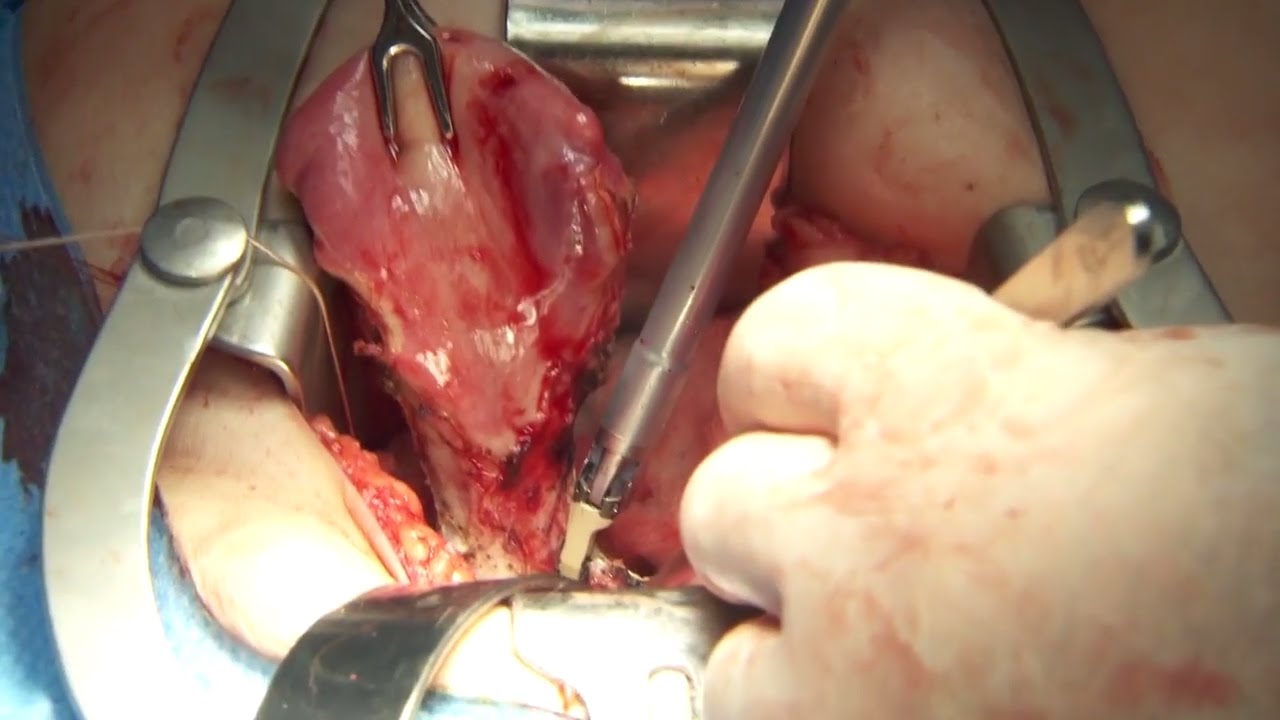
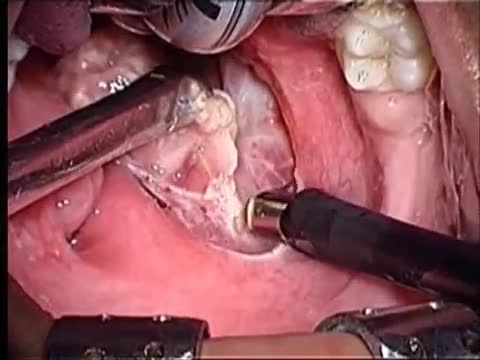
Olympus has extended the value of its award-winning combined surgical energy device, THUNDERBEAT, to open surgical procedures. Watch Dr. Francois Blaudeau master use of THUNDERBEAT Open Extended Jaw (OEJ) in a total abdominal hysterectomy.
http://medical.olympusamerica.com/products/thunderbeat?utm_source=youtube&utm_campaign=Total%20Abdominal%20Hysterectomy%20Surgery%20-%20THUNDERBEAT&utm_medium=description&utm_term=energy&utm_content=surgical

Dr. Debbie Song at Gillette Children's describes in detail selective rhizotomy surgery.
A selective dorsal rhizotomy is an operation performed to treat spasticity. It is thought that high tone and spasticity arise from abnormal signals that are transmitted through sensory or dorsal nerve roots to the spinal cord. In a selective dorsal rhizotomy we identify and cut portions of the dorsal nerve roots that carry abnormal signals thereby disrupting the mechanisms that lead to spasticity. Potential patients go through a rigorous assessment that includes an in-depth gait and motion analysis as well as a physical therapy evaluation.
They are evaluated by a multidisciplinary team that includes a pediatric rehabilitation doctor, a neurosurgeon, and an orthopedist, Appropriate patient selection is vital. Ideal candidates for selective dorsal rhizotomy are children who are between four and ten years of age, have a history of being born prematurely, and have a diagnosis of diplegia cerebral palsy. These patients usually walk independently or with the assistance of crutches or a walker. They typically function at a level one, two, or three in the gross motor function classification system or gmfcs. A selective dorsal rhizotomy involves the coordinated efforts of the neurosurgery, physiatry, anesthesia and nursing teams. The operation entails making an incision in the lower back that is approximately six to eight inches long. We perform what we call a laminoplasty in which we remove the back part of the spinal elements from the lumbar one or l1 to l5 levels. At the end of the procedure the bone is put back on. We identify and open up the Dural sac that contain the spinal fluid spinal cord and nerve roots. Once the Dural sac is opened ,we expose the lumbar and upper sacral nerve roots that transmit information to and from the muscles of the lower extremities.
At each level we isolate the dorsal nerve root, which in turn is separated into as many as 30 smaller thread light fruitlets.
Each rootlet is then electrically stimulated. Specialized members of the physiatry team look for abnormal responses in the muscles of the legs as each rootless is being stimulated. If an abnormal response is observed then the rootlet is cut.
If a normal response is observed, then the rootlet is not cut. We usually end up cutting approximately 20 to 40 percent of the rootlets. The Dural sac is sutured closed and the l1 through l5 spinal elements are put back into anatomic position, thus restoring normal spinal alignment. The overlying tissues and skin are then closed and the patient is awoken from surgery. The entire operation takes between four and five hours. A crucial component to the success of our rhizotomy program is the extensive rehabilitation course following surgery. With their tone significantly reduced after a rhizotomy, patients relearn how to use their muscles to walk more efficiently through stretching, strengthening, and gait training. Approximately one to two years after a rhizotomy patients undergo repeat gait and motion analysis. The orthopedic surgeons assess the need for interventions to correct bone deformities, muscle contractures, poor motor control, impaired balance, or other problems related to cerebral palsy.
At Gillette we work closely with patients and families to ensure that our selective dorsal rhizotomy program meets their goals for enhancing their function and improving their quality of life.
VISIT https://www.gillettechildrens.org/ to learn more
0:00 Why choose selective dorsal rhizotomy?
0:56 Who is a good candidate for selective dorsal rhizotomy?
1:31 What does a selective dorsal rhizotomy entail?
3:26 What is recovery from selective dorsal rhizotomy like?

Pediatric surgeons at Texas Children’s Hospital West Campus perform general surgical procedures such as circumcisions, removal of foreign objects, hernia repair, and suturing of minor lacerations. While more complex surgeries take place at the Texas Children’s Main Campus, pre-operative and follow-up outpatient care for those procedures is available at the West Campus.
Everything about Texas Children’s Hospital West Campus is dedicated to the health and wellness of children. As greater Houston's first suburban hospital designed exclusively for children, we offer the expert care you've come to trust from Texas Children's Hospital coupled with a location that's convenient and accessible for area families. Our facility is located just off the westbound feeder road of the Katy Freeway (at I-10 and Barker Cypress).
For more information about Texas Children's Hospital West Campus, visit http://www.texaschildrens.org/....Locate/In-the-Commun
Meet Dr. Allen Milewicz, chief of community surgery at Texas Children's West Campus
https://www.youtube.com/watch?v=uMoCdipuKfA&index=16&list=PLiN68C9rloPBD-E9ChWhVy73h7V3SEMlm