Top videos

This animation shows you how a tummy tuck is performed at Boerhaave Medical Centre. Curious? Watch the video!
Boerhaave Medical Centre sets itself the goal of providing the highest quality care. Quality not just in terms of treatment, but also in terms of our staff and the before and after care given. By providing thorough information and clear advice in advance, carefully supporting our patients through the procedure and caring for them afterwards, we believe this quality is assured.
Although we are one of the largest clinics in the Netherlands and have built up many years of experience, we continuously strive to improve. After all, the Boerhaave Medical Centre intends to remain a pioneer in the healthcare sector, by working in accordance with the latest medical findings and techniques both now and in the future.
We offer the highest standard of plastic surgery in our cosmetic care department. For 365 days a year, you can also come to us for non-surgical treatments, such as injectables, permanent hair removal and gastric balloons.
We have been awarded the ZKN quality mark and are certified to ISO 9001-2008 for giving advice and carrying out plastic surgery, including after care.
Visit our website for more information: https://www.boerhaave.com/all-....treatments/upperbody
Follow us:
Facebook: https://www.facebook.com/boerhaavemc
Google+: https://plus.google.com/+BoerhaaveNl-Kliniek
Pinterest: https://nl.pinterest.com/BoerhaaveMC/
Instagram: https://www.instagram.com/BoerhaaveMC/

External cephalic version, or version, is a procedure used to turn a fetus from a breech position or side-lying (transverse) position into a head-down (vertex) position before labor begins. When successful, version makes it possible for you to try a vaginal birth.

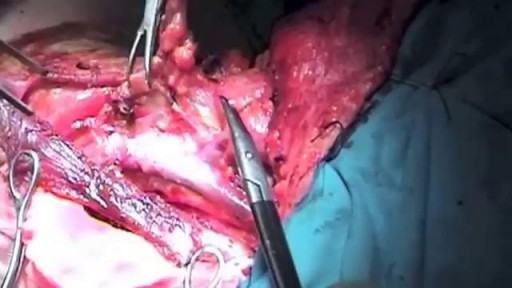
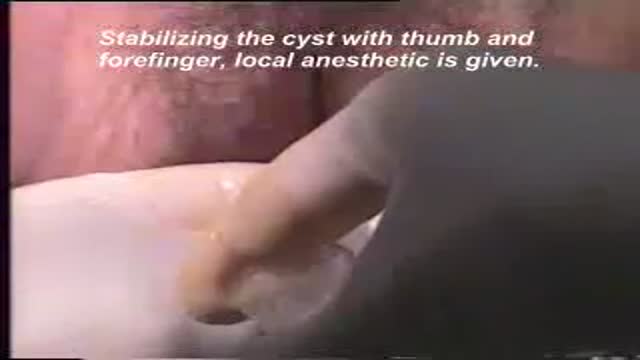
This poor old lady came with swelling in her left buttock for 10 days.She had history of injection in her buttocks two weeks back. She developed painful swelling and redness in her left gluteal region with difficulty in walking.It was diagnosed as injection abscess left gluteal region which needs incision and drainage under local anesthesia.Patient part painted and drapped.2% Lignocaine with adrenaline was infiltrated around the swelling for proper filed block.I use no-11 blade for stab incision over the swelling at the most fluctuating point of the abscess.You can watch how pus was flowing out from the cavity.The aim is to drain all pus from the abscess cavity.Finger exploration is essential to break all loculi inside the cavity, to know the depth and extend of the cavity and to fascilitate proper drainage of residual pus.after pus evacuation,, the cavity should be irrigated with normal saline and betadine solution.lastly the cavity to be packed with betadine soaked guage pieces.Proper dressing is essential.the dressing to be changed after 24 hours.daily dressing is essential with a good antibiotic coverage.the cavity usually obliterates within a period of seven to ten days.

Pediatric surgeons at Texas Children’s Hospital West Campus perform general surgical procedures such as circumcisions, removal of foreign objects, hernia repair, and suturing of minor lacerations. While more complex surgeries take place at the Texas Children’s Main Campus, pre-operative and follow-up outpatient care for those procedures is available at the West Campus.
Everything about Texas Children’s Hospital West Campus is dedicated to the health and wellness of children. As greater Houston's first suburban hospital designed exclusively for children, we offer the expert care you've come to trust from Texas Children's Hospital coupled with a location that's convenient and accessible for area families. Our facility is located just off the westbound feeder road of the Katy Freeway (at I-10 and Barker Cypress).
For more information about Texas Children's Hospital West Campus, visit http://www.texaschildrens.org/....Locate/In-the-Commun
Meet Dr. Allen Milewicz, chief of community surgery at Texas Children's West Campus
https://www.youtube.com/watch?v=uMoCdipuKfA&index=16&list=PLiN68C9rloPBD-E9ChWhVy73h7V3SEMlm

A testicular examination is mainly performed on male patients who present with testicular pathology e.g. pain, swelling, a lump. Although titled testicular examination it involves the examination of the penis, scrotum and testes. As this is an intimate examination it is pertinent to gain a good rapport with your patient, maintain good communication and ensure the patient’s dignity at all times. Remember to offer a chaperone for this skill. For the purposes of your exam, you will most likely be examining a mannequin.

Surgeons in London removed a woman's brain tumor during a very unusual procedure. CBS News' Tina Kraus reports, the patient's love of music helped guide the surgery.
Subscribe to the CBS News Channel HERE: http://youtube.com/cbsnews
Watch CBSN live HERE: http://cbsn.ws/1PlLpZ7
Follow CBS News on Instagram HERE: https://www.instagram.com/cbsnews/
Like CBS News on Facebook HERE: http://facebook.com/cbsnews
Follow CBS News on Twitter HERE: http://twitter.com/cbsnews
Get the latest news and best in original reporting from CBS News delivered to your inbox. Subscribe to newsletters HERE: http://cbsn.ws/1RqHw7T
Get your news on the go! Download CBS News mobile apps HERE: http://cbsn.ws/1Xb1WC8
Get new episodes of shows you love across devices the next day, stream CBSN and local news live, and watch full seasons of CBS fan favorites like Star Trek Discovery anytime, anywhere with CBS All Access. Try it free! http://bit.ly/1OQA29B
---
CBSN is the first digital streaming news network that will allow Internet-connected consumers to watch live, anchored news coverage on their connected TV and other devices. At launch, the network is available 24/7 and makes all of the resources of CBS News available directly on digital platforms with live, anchored coverage 15 hours each weekday. CBSN. Always On.

Site enhancement oil, often called "santol" or "synthol" (no relation to the Synthol mouthwash brand), refers to oils injected into muscles to increase the size or change the shape. Some bodybuilders, particularly at the professional level, inject their muscles with such mixtures to mimic the appearance of developed muscle where it may otherwise be disproportionate or lagging. This is known as "fluffing".Synthol is 85% oil, 7.5% lidocaine, and 7.5% alcohol. It is not restricted, and many brands are available on the Internet. The use of injected oil to enhance muscle appearance is common among bodybuilders, despite the fact that synthol can cause pulmonary embolisms, nerve damage, infections, sclerosing lipogranuloma,[60] stroke,[55] and the formation of oil-filled granulomas, cysts or ulcers in the muscle. Rare cases might require surgical intervention to avoid further damage to the muscle and/or to prevent loss of life. Sesame oil is often used in such mixtures, which can cause allergic reactions such as vasculitis.

For a full Surgical Airway Techniques resource: https://bit.ly/2rb9Nud
Video courtesy of Gauri Mankekar, MBBS, MS, PhD

http://www.amerra.com In this patient education video from Colorectal Surgical Associates in Houston, Texas, learn more about the single incision laparoscopic colectomy procedure. This minimally invasive procedure uses a mini incision that
results in less pain, fewer complications, earlier recovery, and a smaller scar. Colorectal cancer is the second leading cause of cancer death in the United States. For more information please visit our website: www.csamd.com or call (713)-790-0600.

Dr. Debbie Song at Gillette Children's describes in detail selective rhizotomy surgery.
A selective dorsal rhizotomy is an operation performed to treat spasticity. It is thought that high tone and spasticity arise from abnormal signals that are transmitted through sensory or dorsal nerve roots to the spinal cord. In a selective dorsal rhizotomy we identify and cut portions of the dorsal nerve roots that carry abnormal signals thereby disrupting the mechanisms that lead to spasticity. Potential patients go through a rigorous assessment that includes an in-depth gait and motion analysis as well as a physical therapy evaluation.
They are evaluated by a multidisciplinary team that includes a pediatric rehabilitation doctor, a neurosurgeon, and an orthopedist, Appropriate patient selection is vital. Ideal candidates for selective dorsal rhizotomy are children who are between four and ten years of age, have a history of being born prematurely, and have a diagnosis of diplegia cerebral palsy. These patients usually walk independently or with the assistance of crutches or a walker. They typically function at a level one, two, or three in the gross motor function classification system or gmfcs. A selective dorsal rhizotomy involves the coordinated efforts of the neurosurgery, physiatry, anesthesia and nursing teams. The operation entails making an incision in the lower back that is approximately six to eight inches long. We perform what we call a laminoplasty in which we remove the back part of the spinal elements from the lumbar one or l1 to l5 levels. At the end of the procedure the bone is put back on. We identify and open up the Dural sac that contain the spinal fluid spinal cord and nerve roots. Once the Dural sac is opened ,we expose the lumbar and upper sacral nerve roots that transmit information to and from the muscles of the lower extremities.
At each level we isolate the dorsal nerve root, which in turn is separated into as many as 30 smaller thread light fruitlets.
Each rootlet is then electrically stimulated. Specialized members of the physiatry team look for abnormal responses in the muscles of the legs as each rootless is being stimulated. If an abnormal response is observed then the rootlet is cut.
If a normal response is observed, then the rootlet is not cut. We usually end up cutting approximately 20 to 40 percent of the rootlets. The Dural sac is sutured closed and the l1 through l5 spinal elements are put back into anatomic position, thus restoring normal spinal alignment. The overlying tissues and skin are then closed and the patient is awoken from surgery. The entire operation takes between four and five hours. A crucial component to the success of our rhizotomy program is the extensive rehabilitation course following surgery. With their tone significantly reduced after a rhizotomy, patients relearn how to use their muscles to walk more efficiently through stretching, strengthening, and gait training. Approximately one to two years after a rhizotomy patients undergo repeat gait and motion analysis. The orthopedic surgeons assess the need for interventions to correct bone deformities, muscle contractures, poor motor control, impaired balance, or other problems related to cerebral palsy.
At Gillette we work closely with patients and families to ensure that our selective dorsal rhizotomy program meets their goals for enhancing their function and improving their quality of life.
VISIT https://www.gillettechildrens.org/ to learn more
0:00 Why choose selective dorsal rhizotomy?
0:56 Who is a good candidate for selective dorsal rhizotomy?
1:31 What does a selective dorsal rhizotomy entail?
3:26 What is recovery from selective dorsal rhizotomy like?